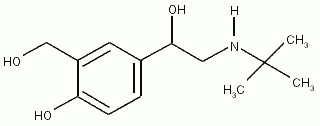
Study objective: This study compares the safety and efficacy of HFA 134a salbutamol sulfate (Airomir in the 3M CFC-free system [3M Pharmaceuticals]) and CFC 11/12 salbutamol (Ventolin [Allen & Hanburys]) in a cumulative dose-response (1, 1, 2, 4, 8 inhalations at 30-min intervals) study in asthmatic patients.
Design: Randomized, single-blind, two-period crossover study.
Participants: Twenty-four stable mild to moderate asthmatics.
Measurements and results: At all cumulative inhalations, the changes in [FEV.sub.1] (absolute, percent, and percent predicted) and FVC were equivalent. There was also no significant difference in heart rate, serum potassium level, BP, 12-lead ECG, Holter monitor recordings, or adverse events. Both HFA 134a salbutamol sulfate and CFC 11/12 salbutamol displayed a significant dose-response for [FEV.sub.1], [FEF.sub.2.sub.5.sub.-.sub.7.sub.5.sub.%], FVC, serum potassium, heart rate, and systolic BP.
Conclusions: HFA 134a salbutamol sulfate and CFC 11/12 salbutamol produced clinically and statistically similar airway responses and side effects. These results indicate that HFA 134a salbutamol sulfate would be a safe and effective substitute for CFC 11/12 salbutamol.
Key words: aerosol propellants; albuterol; asthma; bronchodilators; chlorofluorocarbon; hydrofluoroalkanes; ozone; potassium; salbutamol sulfate; spirometry
Since metered-dose inhalers (MDIs) were introduced in 1956, the use of MDIs has expanded to become the dominant delivery system for pulmonary medications. All currently marketed MDIs use chlorofluorocarbon (CFC) propellants (usually a mixture of CFC-12 [[[CCl.sub.2]F.sub.2]] with CFC-11 [[CCl.sub.3]F] and/or CFC-114 [[[[CClF.sub.2]CClF.sub.2]CClF.sub.2]]). Worldwide in 1988, approximately 5,000 tons of CFCs were used in MDIs, representing 0.5% of the annual CFC production.(1) Other uses included aerosol propellants for consumer products (spray cans), refrigerants, industrial solvents, and as a foam-blowing agent for polystyrene and polyurethane. Although CFCs are, in general, stable and nontoxic in the lower atmosphere, in the stratosphere, slow decomposition of CFCs by solar radiation results in free chlorine radicals, which in turn, catalyze the destruction of ozone.(2) The ozone-destroying potential of CFCs is proportional to the chlorine content.(3) Destruction of the ozone layer allows increased transmission of ultraviolet radiation (UV-C and UV-B) to the earth's surface. Hydrofluoroalkanes (HFA) such as HFA 134a contain no chlorine and cannot be degraded to produce free radicals catalyzing ozone destruction. In addition, the long residence times of CFC in the stratosphere (60 to 200 years) contributes to the greenhouse effect resulting in global warming, whereas HFA 134a (residence time 15.5 years) produces less of a greenhouse effect (HFA 134a has 8.7% of the halo-carbon global warming potential of CFC 12).(4)
In 1978, aerosol propellants were banned for non-medical purposes in North America and some Nordic countries. In 1987, under the auspices of the United Nations Environmental Programme, the Montreal Protocol on Substances that Deplete the Ozone Layer was developed calling initially for a 50% reduction in CFC use by 1998.(5) The Protocol has since been revised several times and now calls for the elimination of CFC production by January 1, 1996, except for uses agreed to be essential. One hundred twenty-two nations have agreed to the Montreal Protocol. Exemptions for essential uses of CFCs are reviewed by the United Nations Environment Programme, Technology and Economic Assessment Panel. Recommended exemptions for essential uses include MDIs for asthma and COPD, special hazards fire protection in the Russian Federation (eg, nuclear submarines), and specific cleaning and bonding applications for the space shuttle. Recommendations for exemptions for the manufacture of MDIs totaled approximately 8,700 metric tons for 1997.(6) Even if the medical use of CFCs were permanently permitted, the economics of manufacturing smaller amounts might result in their discontinuation.
Experimental Design
Subjects were studied on 3 separate days (one screening visit followed by two study visits) over a maximum of 18 days during which no change in their asthma medications was permitted. Study days were separated by 24 h to 8 days. The subjects were block-randomized in groups of eight to receive one of the two treatment sequences. Prior to each visit, inhaled [beta]-agonists, inhaled anticholinergics, and methylxanthine-containing foods or beverages were withheld for 8 h or more, alcohol-containing food and beverages were withheld for 12 h or more, treatment with oral [beta]-agonsts cromolyn sodium and long-acting theophylline compounds was withheld for 24 h or more, and treatment with ultra-long-acting theophylline compounds (once-a-day dosing), antihistamines, aspirin and other nonsteroidal anti-inflammatory drugs was withheld for 48 h or more.
The initial screening evaluation (day 1) consisted of a medical history, vital signs, physical examination, 12-lead ECG, clinical laboratory tests, and spirometry before and after bronchodilation (CFC 11/12 salbutamol). MDI technique was evaluated and corrected using a placebo canister (CFC 11/12).
The second and third study days were conducted at the same time of day (2 h). A peripheral IV catheter was inserted for serial blood sampling. Baseline vital signs, serum potassium, and spirometry were obtained. Baseline [FEV.sub.1] was required to be within 15% of screening [FEV.sub.1] and between 35% and 85% of the predicted value. MDI technique was reviewed. Subjects received 1, 1, 2, 4, and 8 inhalations of either HFA 134a salbutamol sulfate or CFC 11/12 salbutamol at 30-min intervals for a cumulative total of 16 inhalations. At each dose level, the inhalations were administered at approximately 45-s intervals and the maximum time from first inhalation (time 0) to last inhalation was 6 min. Following each dose, heart rate (122 min after the first inhalation), BP (142 min), serum potassium (162 min), and spirometry (182 min) were performed.
[ILLUSTRATION OMITTED]
[ILLUSTRATION OMITTED]
[ILLUSTRATION OMITTED]
[ILLUSTRATION OMITTED]
[ILLUSTRATION OMITTED]
[ILLUSTRATION OMITTED]
Data Analysis
Analysis of variance methods appropriate for a two-period crossover design were used. Factors were sequence, subject within sequence, treatment, and log dose. For each treatment, the log dose-response curves for [FEV.sub.1], [FEF.sub.2.sub.5.sub.-.sub.7.sub.5.sub.%], and FVC were estimated, and linear and quadratic polynomial contrasts were tested. Two approaches were used to test the equivalence of the two treatments. First, an estimate of the within-subject variability in lung function was defined from data from a previous study in which subjects underwent two repeated CFC 11/12 salbutamol sulfate treatment sessions.(12) Twice the within-subject SD from the mean lung function value resulting from the replicated treatment provides a measure of bioequivalence in this study--the equivalence interval. Testing of the null hypothesis of inequivalence of the treatment groups at each cumulative dose level was performed using the two one-sided tests procedure.(13) The p value represents the greater of the probabilities that the actual mean difference in lung function lies above or below the equivalence interval (the observed mean difference could fall on either side of the zero difference midpoint). If both are rejected with a p value of less than 0.05, the alternative hypothesis that the two treatments are equivalent is accepted. Post hoc analyses of covariance (ANCOVA) were performed for [FEV.sub.1] and [FEF.sub.2.sub.5.sub.-.sub.7.sub.5.sub.%]. For the second approach to defining equivalence, the 90% confidence intervals (CIs) for the difference between the two treatment means were obtained at each cumulative dose level. This implies a 90% chance the actual difference lies within the CI (the observed difference is the midpoint). A 95% CI would be larger and more likely to include the zero difference point. Therefore, the 90% CI is a more conservative measure.
[ILLUSTRATION OMITTED]
[ILLUSTRATION OMITTED]
The incidence of abnormal results of clinical laboratory tests and adverse events was compared between groups using Fisher's Exact Test. Comparisons for continuous variables used Student's t test. A p value of [less than or equal to]0.05 was considered statistically significant.
[ILLUSTRATION OMITTED]
[ILLUSTRATION OMITTED]
RESULTS
Both HFA 134a salbutamol sulfate (p[less than]0.0001) and CFC 11/12 salbutamol (p[less than]0.0001) displayed a significant log-linear cumulative dose response for [FEV.sub.1], which is apparent after one inhalation and still increasing up to 16 cumulative inhalations (Fig 1). At all cumulative inhalations, the observed mean difference fell within the equivalence interval (p[less than]0.001) for percentage, absolute, and percent predicted change in [FEV.sub.1]. At higher cumulative doses (8 and 16 inhalations), there was a nonsignificant trend toward a larger response with HFA 134a salbutamol sulfate for absolute, percent, and percent predicted change in [FEV.sub.1]. ANCOVA (dependent variable postdose [FEV.sub.1]) revealed that the predose [FEV.sub.1] (covariate) was significant (p[less than]0.0001), the factor of treatment (HFA 134a salbutamol sulfate vs CFC 11/12 salbutamol) was not significant (p=0.314), and the factor of cumulative inhalations was significant (p[less than]0.0001). The interaction of treatment with cumulative inhalations was not significant (p=0.057), indicating that the trend of larger response with HFA 134a salbutamol sulfate at higher doses was not statistically significant after adjustment for predose [FEV.sub.1]. The 90% CI (Fig 1) does not include zero at 8 and 16 cumulative inhalations, indicating a similar trend toward a larger response with HFA 134a salbutamol sulfate.
[ILLUSTRATION OMITTED]
[ILLUSTRATION OMITTED]
[ILLUSTRATION OMITTED]
[ILLUSTRATION OMITTED]
A significant (p[less than]0.001) log-linear dose-response relationship for absolute and percent change in FVC from predose FVC (Fig 2) was also present for both salbutamol preparations. The effect was apparent after 1 inhalation and still increasing up to 16 cumulative inhalations. At all cumulative inhalations, the observed mean difference fell within the equivalence interval (p[less than]0.001) for absolute and percent change in FVC. The 90% CI was less than 0.2 L and less than 5% change at all cumulative inhalations.
Both salbutamol preparations showed significant (p[less than]0.001) log-linear cumulative dose-response relationships for absolute change in [FEF.sub.2.sub.5.sub.-.sub.7.sub.5.sub.%] from predose [FEF.sub.2.sub.5.sub.-.sub.7.sub.5.sub.%] (Fig 3). The quadratic contrasts (dose-response fit) were also significant (p=0.018), for HFA 134a, but not for CFC 11/12 salbutamol (p=0.066). For change in [FEF.sub.2.sub.5.sub.-.sub.7.sub.5.sub.%], the observed mean difference fell within the equivalence interval (p[less than]0.025). The 90% CI for the difference in absolute change from predose [FEF.sub.2.sub.5.sub.-.sub.7.sub.5.sub.%] was less than 0.5 L/s. The baseline [FEF.sub.2.sub.5.sub.-.sub.7.sub.5.sub.%] (Table 1) was significantly different (p=0.009) between the two treatments. ANCOVA (dependent variable postdose [FEF.sub.2.sub.5.sub.-.sub.7.sub.5.sub.%]) revealed that the predose [FEF.sub.2.sub.5.sub.-.sub.7.sub.5.sub.%] (covariate) approached statistical significance (p=0.060), and the factors of treatment (p=0.032) and cumulative inhalations (p[less than]0.0001) were significant. The interaction of treatment with cumulative inhalations was not significant (p=0.342). Starting from different baseline mean values (2.08 and 2.34 L/s, respectively), with a single inhalation, HFA 134a salbutamol sulfate and CFC 11/12 salbutamol reached nearly the same absolute mean value (2.93 and 2.97 L/s, respectively). Response to subsequent inhalations showed a between-treatment difference of 0.11 L/s or less well within the equivalence interval. The between-drug difference in response from baseline [FEF.sub.2.sub.5.sub.-.sub.7.sub.5.sub.%] appears to be reflected only in the response to the first inhalation.
(15) Podrid PJ. Potassium and ventricular arrhythmias. Am J Cardiol 1990; 65:33E-44E
(16) Haalboom JRE, Deenstra M, Struyvenberg A. Hypokalaemia induced by inhalation of fenoterol. Lancet 1985; 1:1125-27
(17) Crane J, Burgess C, Beasley R. Cardiovascular and hypokalaemic effects of inhaled salbutamol, fenoterol and isoprenaline. Thorax 1989; 44:136-40
COPYRIGHT 1996 American College of Chest Physicians
COPYRIGHT 2004 Gale Group