Urology has seen dramatic changes over the past 20 years. It has moved from an open surgical specialty with few drug treatments to a specialty that has enthusiastically embraced endoscopic (minimally invasive) techniques and new drug treatments for common conditions such as erectile dysfunction and urinary incontinence. The advances that have occurred in the past few years have been mainly in treatment of diseases that are becoming more common as the population ages. These include the two most common urological malignancies, prostate and bladder cancer, as well as lower urinary tract symptoms in older men and urinary incontinence and urinary tract infections, particularly in older women.
Methods
This review concentrates on advances in urology that affect large patient groups and that are having an impact on both community and hospital practice. We have used information gained from attendance at large major urological conferences, which cover all subspecialties within urology, to help select the topics for this article. We also obtained the views of colleagues with subspecialist interests.
Urinary incontinence
There are two main types of urinary incontinence, urge incontinence and stress incontinence. Urge urinary incontinence is due to involuntary contractions of the detrusor muscle during bladder filling, whereas stress incontinence occurs when physical exertion raises the bladder pressure and is due to incompetence of the urethral sphincter mechanism.
Urge urinary incontinence is age related. Bladder training and antimuscarinic drugs remain the principal treatments. Treatment with oxybutynin is often difficult as the dose has to be titrated and it has a high incidence of troublesome side effects. Tolterodine has a similar therapeutic effect but with fewer side effects. Other new preparations such as oxybutynin extended release and propiverine also seem promising.[1] In patients resistant to conservative measures, new surgical techniques such as neuromodulation (bilateral stimulation of sacral (S3) nerve roots) and detrusor myectomy (fig 1) are being used instead of ileocystoplasty, which is a major procedure and produces its own long term problems.
[Figure 1 ILLUSTRATION OMITTED]
Stress urinary incontinence has become a more common reason for referral as women seek to remain active for longer and often wish to increase their sporting pursuits. Weight reduction, stopping smoking, and pelvic floor exercises should be standard in all women with stress incontinence and will produce satisfactory improvement in 30% of women.[2] The type of surgical repair used to be chosen on the basis of the presumed pathophysiology (suspension for urethral hypermobility and sling for internal sphincter deficiency). Current thinking is that virtually all patients with sphincter incontinence have a combination of the two problems.[3] Suspensions are suitable only for women in whom hypermobility is the primary problem, whereas slings are successful in either group. Two high quality randomised controlled multicentre trials are currently being conducted in the United Kingdom concerning the surgical treatment of stress incontinence. Colposuspension (the open Burch procedure) is being compared with a new suburethral sling procedure (the transvaginal tape) in a Newcastle based study and with laparoscopic colposuspension in a second study organized by the University of Manchester. The first study will shortly report the results of six month follow up. The Manchester study will finish recruiting in early 2001 and report later next year. However, although the early results of surgical treatment for stress incontinence are often promising, the effects after two years can be disappointing. Longer follow up for all trials is therefore essential.
The management of incontinence has been defined by new clear algorithms.[4] The first step is to ensure that each patient receives a proper structured initial evaluation by appropriately trained staff. This principle is also endorsed in the Department of Health's recent publication Good Practice in Continence Services.[5] Urinary incontinence is very common, but most people do not desire or require radical treatment. The first international consultation on incontinence, sponsored by the World Health Organization, emphasises the value of non-medical, non-surgical treatments such as bladder training for urge incontinence and pelvic floor rehabilitation for stress incontinence. The consultation used a "quasi Cochrane" approach to analyse the evidence for its recommendations.[6]
Older men with lower urinary tract symptoms
The nomenclature used to describe this group of patients has changed.[7] The most recent WHO sponsored consultation held in Paris in 2000 recommended that as well as lower urinary tract symptoms the terms benign prostatic enlargement and bladder outlet obstruction should become standard. Benign prostatic hyperplasia will then be used exclusively to describe the characteristic histological picture.[8]
Lower urinary tract symptoms suggestive of bladder outlet obstruction are usually treated empirically in primary care, and two effective classes of drugs are now available. The new [Alpha] adrenergic antagonists, tamsulosin and alfuzosin, produce fewer side effects than previous drugs in the same group.[9] Finasteride (a 5-[Alpha] reductase inhibitor) has been shown to reduce the size of large prostates (volume [is greater than] 40 [cm.sup.3]), although it takes six to eight months to produce its full effect.[9] It provides some protection against the complications of bladder outlet obstruction, including acute retention.[10]
In surgery, interest has focused on the use of less invasive procedures that cause less morbidity than transurethral resection of prostate. Numerous techniques that aim to destroy prostatic tissue by heat--for example, by laser, vaporisation, radio frequency, or ultrasound--have been and are being evaluated, but insufficient data are available from randomised controlled trials to determine whether they are cost effective and produce sustained benefit. Traditional transurethral resection uses cautery, and new methods of incising prostatic tissue are now being evaluated that may have advantages, including reduced blood loss.[11] The holmium yttrium-aluminium-garnet laser technique is the closest to traditional transurethral resection in that it removes tissue under endoscopic control. This is now a recommended surgical technique.[12] However, traditional transurethral resection by an experienced surgeon with modern equipment is highly effective and safe.
Oncology
Prostate cancer is increasingly detected at an earlier stage by serum measurement of prostate specific antigen.[13] Although prostate specific antigen is probably the best available blood test for detecting any cancer, it still has somewhat limited specificity and sensitivity. Its value has been improved by techniques such as monitoring change in concentration with time (velocity), assessing concentration in relation to prostate volume and to age, and, most recently, measuring the free to total prostate specific antigen ratio (the lower the ratio the greater the chance of prostate cancer being detected by biopsy). Controversy continues about the treatment of apparently localised prostate cancer. However, radical treatment is generally not justified in patients with a prostate specific antigen concentration over 20 [micro]g/l, as the tumour will often extend beyond the prostatic capsule.[14] The grade of tumour and the life expectancy of the patient also influence the final decision. Patients with well differentiated tumours may do well without treatment, whereas those with poorly differentiated tumours usually do badly. Most men have moderately well differentiated tumours and are likely to benefit from radical treatment if they have a life expectancy of more than 10 years.
Radical prostatectomy has two important complications: incontinence and impotence. A new method of radical prostatectomy by laparoscopy seems to reduce morbidity and hospital stay.[15] The complications of radical prostatectomy have prompted the use of new types of brachytherapy; transperineal implantation of radioactive iodine or palladium seeds has attracted great publicity, particularly in the United States.[16] However, the technique is not being evaluated in a randomised controlled trial to determine whether it is better than watchful waiting.[17] The NHS is currently funding a trial in three British centres on the feasibility of mounting a randomised controlled study of treatments for early prostate cancer.
Endo-urology
New instruments such as the flexible ureterorenoscope have made it possible to inspect the whole of the urinary tract, from kidney to urethra, via the urethra. Many kidney conditions can now be treated less invasively by a percutaneous approach through the loin, retrograde approaches through the urethra, bladder, and ureter, or laparoscopy. Almost all patients with upper urinary tract stones can now have them removed endoscopically or by lithotripsy (box).[18] Endoscopic techniques are also used in combination with other new technologies. Lasers applied through ureteroscopes and cystoscopes can be used to destroy transitional cell carcinomas in both the upper and lower urinary tracts as well as to disintegrate urinary tract stones. Many of these procedures can now be performed as day cases, often under local anaesthesia.
Improved and earlier imaging with ultrasonography, computed tomography, or magnetic resonance imaging has resulted in early diagnosis of relatively small renal cell carcinomas. Laparoscopic surgery is being evaluated to assess whether it has equivalent disease free survival to open surgery with fewer complications and reduced morbidity and costs. A similar analytical approach is needed to assess whether laparoscopic transplant nephrectomy, now common in the United States, should be used more widely.
Endo-urology is costly in terms of both staff and equipment. New techniques must therefore be shown to produce benefits for both patients (reduced morbidity) and society (reduced costs) before being widely used.
Andrology
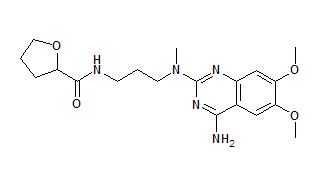
Much has been written about sildenafil, which has revolutionised the treatment of erectile dysfunction. However, in some countries, including the United Kingdom, the cost of sildenafil is not reimbursed by the state for most men with erectile dysfunction. General practitioners in the United Kingdom can now prescribe the drug privately, and several guidelines have been produced to inform and educate general practitioners about the investigation and treatment of erectile dysfunction (www.bui.ac.uk).[19] Insertion of penile prostheses is still required for men in whom sildenafil is ineffective and who do not respond to or dislike intracavernosal injections or vacuum devices, particularly men with diabetes, cardiovascular disease, or neurological disease (fig 2). Surgical treatment may also be required in some patients with Peyronie's disease.
[Figure 2 ILLUSTRATION OMITTED]
Paediatric urology
In the United Kingdom the emergence of clinical governance is greatly changing paediatric urology. For example, surgical management of the rare condition bladder exstrophy will be concentrated in two centres. This is important as surgery for exstrophy still leaves many patients with continence and sexual problems.[20] Some advances have brought almost as many problems as they solve: the advent of prenatal ultrasonography has led to the diagnosis of spina bifida, hydronephrosis, urethral valves, oligohydramnios, and even bladder exstrophy before birth. Many parents elect to have the pregnancy terminated if the prenatal diagnosis suggests a poor prognosis. The accuracy of the diagnosis is often uncertain, particularly in terms of predicting renal function. Prenatal insertion of vesicoamniotic shunts in babies with urethral obstruction may benefit some, but often the degree of renal dysplasia means that intervention is unhelpful. The diagnosis of unilateral hydronephrosis means that the pregnancy is surrounded by uncertainty for the parents, and the postnatal investigations of the baby sometimes turn out to be unnecessary.[21]
Looking to the future
The evidence base relating to recent advances in urology is deficient in several respects. Little information is available on cost effectiveness or the effect on quality of life. Randomised controlled trials are the best way to assess new methods of management. New drugs have to be evaluated in randomised controlled trials, and the appropriate authorities monitor any developments. However, devices and new surgical techniques can be introduced without evidence of efficacy in many parts of Europe. Governments should insist that, after brief pilot studies, new devices and treatments are available only within randomised controlled trials until they are shown to be effective, safe, and cost effective in the widest sense. However, responsiveness and funding are important obstacles to this goal. Most countries are reducing government funding for the assessment of technological developments in medicine, making researchers ever more reliant on commercial financial support We hope that this process can be re-evaluated so that in future genuine advances in urology can be developed and made available to patients as rapidly as possible.
Recent advances
Urology is increasingly becoming superspecialised
Urological conditions such as prostate cancer, urinary incontinence, and lower urinary tract symptoms are becoming more prevalent as the population ages
Effective drug treatments have been developed for incontinence and erectile dysfunction
Less invasive procedures are increasingly replacing open surgery for many urological conditions
Management of stones in urinary tract
Kidney
Extracorporeal shockwave lithotripsy Percutaneous nephrolithotomy
Ureter
Extracorporeal shockwave lithotripsy Ureteroscopy with electrohydraulic lithotripsy Laser lithotripsy
Bladder
Endoscopic litholopaxy with stone forceps Electrohydraulic lithotripsy Laser lithotripsy Open surgery (for "hen's egg" sized stones)
Online resources
British Association of Urological Surgeons: www.baus.org.uk
The principal organisation in the UK for urological surgeons; the site lists all major national and international meetings and deals with continuing urological education
Bristol Urological Institute: www.bui.ac.uk
Contains reviews, urological guidelines for general practice, and information on the institute's courses and meetings
Uroweb: www.uroweb.org
Displays poster presentations, has a comprehensive slide and literature library, and highlights congress information and subspecality presentations and reviews
Continence Foundation: www.continence-foundation.org.uk
Provides information for the public on symptoms, treatments, products, publications, and organisations as well as specific pages for healthcare professionals
US National Institutes of Health--Urology Section: www.niddk.nih.gov/health/urolog/urolog.htm
Displays statistical information; contains online easy to read publications (in Spanish as well as English)
American Urological Association: www.auanet.org
Information on major international meetings, as well as information for patients and the media, available through Uromart, which displays news on how and where to buy urological products
We thank David Frank, Clive Gingell, Anthony Timoney, and Frank Keeley for their comments.
Competing interests: PA has consulted for and received fees for attending, speaking at, and organising meetings and funds for research and staff from several organisations that produce drugs and devices used in lower urinary tract dysfunction. AW has acted as consultant to C R Bard, Conticare, Eli Lilly, Medtronic, Zeneca, TAP, Pharmacia, and Merck and taken part in or lectured at meetings organised by the last four companies.
[1] Bulmer P, Abrams P. The overactive bladder. Reviews in Contemporary Pharmacotherapy 2000;11:1-10.
[2] Wilson PD, Bo K, Bourcier A, Hay-Smith J, Staskin D, Nygaard I, et al. Conservative management in women. In: Abrams P, Khoury S, Wein A, eds. Incontinence-proceedings of first international consultation on incontinence. London: Health Publications, 1998:585-94.
[3] DeLancey JOL, Fowler CJ, Keane D, Macarak E, Mostwin J, Elbadawi A, et al. Pathophysiology. In: Abrams P, Khoury S, Wein A, eds. Incontinence-proceedings of first international consultation on incontinence. Geneva: World Health Organization, 1998:280-6.
[4] Abrams P, Lowry SK, Wein AJ, Bump R, Denis L, Kalache A, et al. Assessment and treatment of urinary incontinence. Lancet 2000;355:2153-8.
[5] Department of Health. Good practice in continence services. London: Doll, 2000.
[6] Abrams P, Khoury S, Wein A, eds. Incontinence-proceedings of first international consultation on incontinence. Geneva: World Health Organization, 1998.
[7] Abrams P. New words for old: lower urinary tract symptoms for prostatism. BMJ 1994;69:929-30.
[8] Abrams P, McConnell J, Roehrborn C, Khoury S, Debruyne F, Denis L, et al. Recommendations for terminology. In: Fifth WHO sponsored international consultation on benign prostatic hyperplasia. Geneva: WHO (in press).
[9] Bell R, Abrams P. The evidence-base for medical intervention. In: McNicholas T, Kirby M, Miles A, eds. The effective management of BPD and LUTS. London: Aesculapius Medical Press, 2000:79-98.
[10] McConnell JD, Bruskewitz R, Walsh P, Andriole G, Lieber M, Holtgrewe HL, et al. The effect of finasteride on the risk of acute urinary retention and the need for surgical treatment among men with benign prostatic hyperplasia. N Engl J Med; 338:557-63.
[11] De la Rosette JJMCH. Future perspectives. Eur Urol 1999;35:173-6.
[12] Abrams P, McConnell J, Roehrborn C, Khoury S, DeBruyne F, Denis L, et al. Surgical treatments subcommittee. In: Fifth WHO sponsored international consultation on benign prostatic hyperplasia. Geneva: WHO (in press).
[13] Murphy M, Johnston C, Whelan P, Rider L, Lloyd SN. Changing trends in prostatic cancer. BJU Int 1999;83:786-91.
[14] Partin AW, Yoo J, Carter HB, Pearson JD, Chan DW, Epstein JI, et al. The use of prostate specific antigen, clinical stage and Gleason score to predict pathological stage in men with localised prostate cancer. J Urol 1993;50:110.
[15] Guillonneau B, Vallancien G. Laparoscopic radical prostatectomy: the Montsouris technique. J Urol 2000;163:1643-9.
[16] Stone NN, Stock RG. Prostate brachytherapy: treatment strategies. J Urol 1999:162:421-6.
[17] Dearnaley DP, Kirby RS, Kirk D, Malone P, Simpson RJ, Williams G. Diagnosis and management of early prostate cancer. Report of a British Association of Urological Surgeons working party. BJU Int 1999;83: 18-33.
[18] Whitfield HN. The management of ureteric stones. 2. Therapy. BJU Int 1999;84:916-21.
[19] Ralph D, Bloomfield M, Dinsmore W, Gingell C, McNicholas T. UK management guidelines for erectile dysfunction. London: Royal Society of Medicine, 1999:3-19.
[20] De Jong TPVM. Treatment of bladder exstrophy and epispadias. Eur Urol 1999;36:1-7.
[21] Ulman I, Jayanthi VR, Koff SA. The long-term follow-up of severe newborn hydronephrosis initially managed without surgery. BJU Int 1999;83 (suppl 3):73.
Bristol Urological Institute, Bristol BS10 5NB
Paul Abrams professor of urology
Alan Wein professor
Correspondence to: P Abrams p_abrams@bui.ac.uk
BMJ 2000;321:1393-6
COPYRIGHT 2000 British Medical Association
COPYRIGHT 2001 Gale Group