Influenza viruses are highly contagious viruses that are transmitted from person to person, usually by the airborne route. Persons in semi-closed or crowded environments, such as students and residents of nursing homes, are at high risk of exposure. The illness attack rate in children ranges from 14% to 40% yearly. Fatality rates are highest in persons who have chronic medical conditions, such as chronic obstructive lung disease, cardiovascular disease, and diabetes mellitus, particularly if they are elderly. The effectiveness of influenza vaccine in preventing or attenuating illness varies, depending primarily on (1) the degree of similarity between the virus strains included in the vaccine and those that circulate during the influenza season, and (2) the age and immunocompetence of the vaccine recipient. When there is a good match between vaccine and circulating viruses, influenza vaccine has been shown to prevent illness in approximately 70% to 90% of healthy persons less than 65 years of age. Adverse events following influenza vaccine include mild, local reactions at the injection site (up to 20%) and occasionally fever in approximately 1% of vaccinees.
Despite the availability of an effective vaccine, only 55% of persons 65 years of age and older reported receiving influenza vaccine in 1994. Vaccination levels are even lower in persons less than 65 years of age with highrisk medical conditions. Important procedures to improve vaccination rates are (1) assessment of a practice's or medical facility's current vaccination rates, (2) identification of target populations for vaccination, (3) formation of a specific goal (ie, percentage of target population to be immunized), (4) development of a plan of action, and (5) provision of ongoing feedback to the individual physicians about vaccination rates of their own patients.
KEY WORDS. influenza; influenza virus; amantadine; rimantadine; education, medical, continuing. (J Fam Pract 1997:45:107-124).
Influenza outbreaks of varying severity occur every winter (Figure 1). In each of nine recent US epidemics, there were more than 20,000 estimated influenza-associated deaths; the figure climbed to more than 40,000 excess deaths in selected epidemics.[1] Furthermore, during some epidemics of influenza type A, there have been approximately 172,000 extra hospitalizations due to influenza and pneumonia.[2] The cost of a severe influenza epidemic has been estimated to be almost $12 billion.[3]
Influenza outbreaks strain the health care system. In 11% of office visits to family physicians during the peak of the influenza season were for influenza-like illness.[4]
Influenza Virus
Influenza is caused by infection with influenza types A or B, which are RNA viruses of the orthomyxovirus family. Influenza virus has two surface antigens that are used for subtyping influenza A viruses: hemagglutinin (H) and neuraminidase (N). Subtypes are classified by H and N antigen type; H1N1, H2N2, and H3N2 are the three influenza A subtypes known to have caused disease in humans since 1918. These antigens periodically change, leading to antigenic shift and drift. Antigenic shift is a major change in the subtypes and occurs in influenza type A only. The result of a shift is a new strain to which there is little or no prior immunity. Subsequently, a pandemic (worldwide epidemic) usually results, with high attack rates occurring in all age groups. Minor changes in the antigenic types are called antigenic drift and occur on a regular basis. Antigenic drift can occur for both types A and B. Changes in the influenza virus due to drift are classified by designating prototype viruses such as A/Texas/36/91.
Influenza type C, one of many viruses that cause the common cold syndrome, does not cause severe disease or predispose to complications.
Influenza Communicability
Influenza is extremely contagious and is transmitted from person to person, usually by the airborne route. Consequently, persons in semi-closed or crowded environments, such as students, prisoners, and residents of nursing homes, are at high risk of exposure. In nursing homes, attack rates can approach 60%[5,6] and case-fatality rates can reach 30%.[7] Infected persons are most contagious during the period of peak symptoms. The incubation period is usually 2 days (range 1 to 4 days).
Clinical Description, Differential Diagnosis, And Complications
Influenza is an acute, usually self-limited, febrile illness. Inflammation of the nasal mucosa, pharynx, conjunctiva, and respiratory tract commonly occurs. The symptoms vary greatly according to age (Table 1). The primary symptoms of influenza in children are cough, rhinorrhea, and croup; whereas, the primary symptoms in adults are cough, myalgia, headache, and sore throat. In the elderly, cough alone or cough with headache are most common.
[TABULAR DATA NOT REPRODUCIBLE IN ASCII]
The diagnosis of influenza (or, more specifically, an influenza-related respiratory illness) is made on clinical grounds, given that an outbreak is occurring in the community. Influenza viral cultures from nasal or pharyngeal swabs, nasal aspirates, or washes can be done when a definitive diagnosis is needed. However, the clinical diagnosis suffices for treatment during outbreak situations. Viral culture requires a minimum of 24 hours to demonstrate virus and 1 to 2 additional days to identify the virus type or subtype. Thus, a culture is helpful in determining the etiology of local epidemics, but not in individual case management. A rapid (<15-minute) diagnostic test for influenza A antigen in a clinical specimen is also available; it has a sensitivity of 100% and a specificity of 91.6%.[8] This should permit quick assessment so that an antiviral agent can be recommended for treatment if type A is present (see section on amantadine and rimantadine). Alternatively, antiviral treatment can be initiated for patients whose symptoms are compatible with influenza, when influenza A viruses are circulating in the community.
The differential diagnosis of influenza includes many respiratory viral infections such as respiratory syncytial virus, parainfluenza virus, adenovirus, and enterovirus, as well as mycoplasma, chlamydia, streptococcal pharyngitis, atypical pneumonia caused by one of these agents, and Q fever. In uncomplicated influenza, the white blood cell count is normal in the majority of cases,[9] but lymphopenia is common.[10] Chest x-ray films are abnormal in about 10% of influenza cases, provided a secondary infection has not occurred.
The complications of influenza are secondary bacterial pneumonia (most commonly caused by Streptococcus pneumoniae, Staphylococcus aureus, and Haemophilus influenzae),[11] worsening of chronic respiratory and cardiac diseases, sinusitis, otitis media, and, rarely, primary viral pneumonia or Reye syndrome, which is associated with salicylate use concomitant with influenza type A or B infection in children. During the influenza season, hospitalizations increase due to pneumonia, acute bronchitis, chronic respiratory disease, and congestive heart failure.[12]
Characteristics of Persons Most Likely to Have Complications
The fatality rate from influenza is highest in persons who have chronic medical conditions, such as chronic obstructive lung disease, cardiovascular disease, and diabetes mellitus, particularly if they are elderly. Influenza has a higher case-fatality rate in middle-aged persons with chronic medical conditions than persons [greater than or equal to] 65 years of age who are well (Table 2). Thus, the approach to influenza vaccine indications needs to incorporate the presence of chronic medical conditions in addition to well-known age criteria.
[TABULAR DATA NOT REPRODUCIBLE IN ASCII]
The elderly, due in part to a high rate of chronic medical conditions, are the population with the highest age-specific case-fatality rate from influenza. More than 90% of the deaths due to influenza occur in persons 65 years of age and older.[1] Furthermore, the hospitalization rate for influenza is high in the elderly. For instance, in recent years, persons 65 years of age and older accounted for 35% to 46% of hospitalizations for influenza-like illness (ILI), although they accounted for only 9% to 10% of office Visits for ILI.[4,13]
Characteristics of Persons Most Likely to Contract Influenza
In contrast to the case-fatality rate, the illness attack rate is highest in children (14% to 40% yearly).[14] Infection is most likely to occur during the winter. Transmission in schools plays a major role in propagating influenza outbreaks, as seen by the rapid rise in student cases following holiday recesses.[15] Children frequently infect their families, as suggested by the increase in school absenteeism just prior to a noted increase in absenteeism among manufacturing employees and by the higher risk of infection for families with children than those without children.[15,16] Another indication of the importance of children in influenza transmission is the success of a vaccination program that targeted grade-school and high-school children in order to limit an outbreak in an entire community.[17]
Influenza Vaccine
The influenza vaccines currently licensed contain inactivated (killed) virus. There are two types of inactivated influenza vaccine: intact (whole) and split virus. Split-virus vaccines have fewer adverse events in children. Only the split-virus vaccines are recommended for children younger than 13 years old; adults may receive either type of vaccine. The dose is 0.5 mL intramuscularly (IM) except for children younger than 3 years old. Children 6 months through 35 months of age should receive 0.25 mL IM. Influenza vaccine should be administered intramuscularly -- into the deltoid muscle in older children and adults, and into the anterolateral thigh in young children.
Influenza Vaccine Efficacy
The effectiveness of influenza vaccine in preventing or attenuating illness varies, depending primarily on (1) the degree of similarity between the virus strains included in the vaccine and those that circulate during the influenza season, and (2) the age and immunocompetence of the vaccine recipient. When there is a good match between vaccine and circulating viruses, influenza vaccine has been shown to prevent illness in approximately 70% of healthy persons less than 65 years of age. When the match between vaccine and circulating virus is poor, efficacy is less. Reported efficacy also varies by the type of research design used.
Elderly persons and persons with certain chronic diseases may develop lower postvaccination antibody titers than healthy young adults and thus may remain susceptible to influenza illness. However, even if they develop influenza illness despite vaccination, the vaccine lowers the risk of severe disease and complications. This is true both for elderly persons in nursing homes and in the community at large. Among elderly persons residing in nursing homes, influenza vaccine can be 50% to 60% effective in preventing hospitalization and pneumonia, and [greater than or equal to] 80% effective in preventing death, even though efficacy in preventing influenza illness may be in the range of 30% to 40%. Achieving a high rate of vaccination among nursing home residents can reduce the spread of infections in a facility, thus preventing disease through herd immunity. Among elderly persons in the community, the effectiveness of influenza vaccine in preventing hospitalization during the influenza season for all causes of pneumonia and influenza ranges from 30% to 70%.[1,18-23] Furthermore, influenza vaccination resulted in a 37% reduction in hospitalization due to congestive heart failure in one study[23] and was 27% to 54% effective in reducing mortality from all causes.[19,23]
Immunity from influenza vaccine wanes following vaccination and may not persist beyond a year. Hence, annual vaccination just prior to the influenza season is recommended. It may take up to 2 weeks after vaccination for protection to develop.
Cost-effectiveness of Influenza Vaccine
In noninstitutionalized elderly adults, influenza vaccination has been documented to reduce the cost of hospitalization due to acute and chronic respiratory disease and congestive heart failure, resulting in a direct savings of $117 per vaccinee per year.[23] Other studies estimated the cost at $13 per year of healthy life gained[24] and $145 per year of life gained.[25] In summary, influenza vaccination has been documented to be cost-effective and, at times, cost-saving.
Adverse Events
Possible adverse events following influenza vaccine include mild, local reactions at the inflection site[26] and occasionally fever. Since it is not a live vaccine, it cannot cause influenza. The current vaccines are considerably purer than vaccines produced prior to 1968, and thus cause far fewer adverse events. In October 1976 through January 1977, a vaccine containing influenza A/New Jersey was associated with Guillain-Barre syndrome (the swine flu episode)[27]; the attributable risk was estimated at 8.8 cases per 1 million vaccinations. This influenza vaccine is no longer in use. Subsequent influenza vaccines have not been clearly associated with an increased incidence of Guillain-Barre syndrome, although estimating the risk of this rare condition is difficult.[1]
Indications for Influenza Vaccine
Influenza vaccine is recommended for persons at risk for influenza complications and their contacts. Persons who are 6 months of age and older with chronic pulmonary, cardiovascular, renal, metabolic, or immunosuppressive diseases, as well as all those 65 years of age and older should receive annual influenza vaccination in the fall (Table 3).
[TABULAR DATA NOT REPRODUCIBLE IN ASCII]
Influenza vaccine is not recommended for infants younger than 6 months of age. Previously unvaccinated children less than 9 years of age should receive two doses, at least 1 month apart, in the first year that they receive influenza vaccine.[1]
Beginning each September, when vaccine for the upcoming influenza season becomes available, persons at high risk who are seen by health care providers should be offered influenza vaccine so that vaccination opportunities are not missed. The optimal time for organized vaccination campaigns for persons in high-risk groups is usually from October through mid-November.[1]
Persons who are in contact with chronically ill patients, eg, health care providers and home care providers, should receive influenza vaccine yearly so that they are not a source of transmission (Table 4). It is unfortunate that only about one-eighth to one-third of medical personnel are immunized each year[28,29] despite the risk that they pose to patients. To reduce transmission in crowded environments, residents of nursing homes and other chronic care facilities should be immunized.
[TABULAR DATA NOT REPRODUCIBLE IN ASCII]
Since the target groups for influenza and pneumococcal vaccines overlap, providers should assess the need for pneumococcal vaccine when administering influenza vaccine to high-risk persons. Influenza vaccine can be administered simultaneously, but at different injection sites, with pneumococcal vaccine or routine childhood vaccines.
Contraindications
The main contraindication to influenza vaccine is anaphylaxis to eggs or other vaccine components. Persons who can eat eggs without experiencing a reaction generally can be vaccinated. Skin testing can help differentiate those who have a true immediate hypersensitivity reaction to egg protein from those who do not. A protocol is available for influenza vaccine administration to persons who have a true allergy to egg protein yet need influenza vaccine due to high-risk conditions.[30] This protocol should be used only in a setting where emergency equipment is available.[30] Influenza vaccine contains small amounts of thimerosal, a mercurial antibacterial agent that acts as a preservative. Severe allergy to this component is rare. Allergy to duck dander or duck meat is not a contraindication. Influenza vaccination should be delayed in persons who have an acute, febrile illness. A person who has a contraindication to influenza vaccine may be a candidate for amantadine or rimantadine prophylaxis.
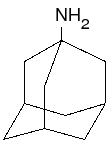
Amantadine and Rimantadine
Amantadine and rimantadine are effective antiviral drugs for the prophylaxis and treatment of influenza type A infections; they are not effective against influenza type B infections. They may be used prophylactically in high-risk groups, eg, persons who have not been vaccinated or need additional control measures, during epidemics of influenza A. Providers may contact their state or local health departments or the CDC Voice Information Service at (404) 332-4555 to find out the most current information about influenza outbreaks, including the type of influenza virus involved. Amantadine and rimantadine should not be considered as substitutes for influenza vaccination unless influenza vaccine is contraindicated. They are 70% to 90% effective in preventing influenza type A.[1] Amantadine or rimantadine prophylaxis should be considered in the following situations:
1. One of these antiviral agents should be administered as an adjunct to vaccination in persons who are at increased risk for influenza complications and have not been immunized until after influenza type A has begun in a community. They should be given for 2 weeks after vaccination because 2 weeks are required for adequate antibody levels to develop in adults following vaccination.
2. Antiviral drugs may be indicated for immunodeficient persons, eg, those with HIV infection, who are at risk for influenza complications and are expected to have a poor antibody response to influenza vaccine due to their immunodeficiency.
3. Antiviral drugs may be used throughout the influenza season for persons who have valid contraindications to influenza vaccine.
4. Amantadine or rimantadine should be considered for unvaccinated medical personnel and for unvaccinated household contacts of persons who are at high risk for influenza complications. For persons who have a valid influenza vaccine contraindication, prophylaxis may be continued throughout the influenza season. For those who were recently vaccinated, prophylaxis may be given for the 2 weeks needed for antibodies to develop.
5. During influenza type A outbreaks in institutions that house high-risk persons, eg, nursing homes, amantadine or rimantadine should be given to all unvaccinated employees and to all residents regardless of vaccination status. Prophylaxis should be considered for all employees, regardless of their vaccination status, if the outbreak is caused by a variant strain of influenza A that may not be controlled by the vaccine.
Antiviral drugs can be administered prophylactically to anyone who wishes to avoid influenza A illness, after considering the risks and benefits in consultation with their healthcare provider.
In the treatment of influenza, both amantadine and rimantadine decrease the duration of fever and symptoms when administered within 48 hours of the onset of the illness. Treatment may be begun on clinical grounds if influenza type A is known to be circulating in the community. Drug-resistance may develop during treatment of infected persons with either medication. To reduce this possibility, treatment should be discontinued after 3 to 5 days, or within 24 to 48 hours of the disappearance of symptoms. Although there is no evidence that drug-resistant viruses are more virulent than drug-sensitive viruses, persons taking amantadine or rimantadine treatment might transmit drug-resistant influenza virus to other persons. Thus, they should avoid contact with uninfected persons as much as possible while they are infectious.
The Food and Drug Administration (FDA) has
[TABULAR DATA NOT REPRODUCIBLE IN ASCII]
Sponsored by the Association of Teachers of Preventive Medicine, the Centers for Disease Control and Prevention, the Department of Family Medicine and Clinical Epidemiology of the University of Pittsburgh School of Medicine, and the Center for Continuing Education in the Health Science of the University of Pittsburgh.
Audience
The intended audience for these materials is primary care physicians.
AAFP Credit
This program has been reviewed and is acceptable for 2.0 prescribed hours by the American Academy of Family Physicians. Term of approval is one year from beginning distribution date of August 1, 1997, with option to request renewal.
To obtain AAFP credit, the physician should read the article, work through the thought problems, (answers are provided), take the posttest, and return the posttest with a check for $22.00, payable to the University of Pittsburgh. The posttest and check should be mailed to the attention of Ellen R. Ahwesh, Department of Family Medicine, M-200 Scaife Hall, 3550 Terrace Street, Pittsburgh, PA 15261.
Disclosure Statement
In accordance with the policies on disclosure of the Accreditation Council for Continuing Medical Education and the Faculty Advisory Committee for Continuing Education in the Health Sciences of the University of Pittsburgh, presenters for their program have identified no personal relationships with a health care product company which, in the context of their topics, could be perceived as a real or apparent conflict of interest.
Objectives
At the end of this session, every learner should be able to accomplish the following core set of objectives: (1) evaluate a given patient who has symptoms and identify possible diagnoses, (2) explain the general epidemiology of influenza, including the risk of contracting disease in confined environments, eg, nursing homes, (3) given a patient scenario, recommend influenza vaccination appropriately, according to occupation, health status, environmental risk factors, and age guidelines, (4) describe general influenza vaccine safety and adverse events, (5) given an office setting, (a) describe the process of choosing a target patient group and a goal, ie, vaccination rate, for influenza vaccination, (b) devise office procedures to improve provider ability to recommend influenza vaccination, if indicated, and (c) select office procedures to improve patient compliance, given that patients may not routinely visit their physician during the ideal time period. approved both amantadine and rimantadine for prophylaxis of influenza type A in persons 1 year of age and older. Amantadine has been approved for the treatment of persons 1 year of age and older (including adults). Although rimantadine is efficacious in the treatment of adults with influenza, there is a lack of data regarding the efficacy of rimantadine for treatment of influenza in children. Hence, rimantadine is approved for the treatment of influenza only in adults 18 years of age and older.
The dosage for amantadine and rimantadine varies by weight, age, and medical condition (Table 5). Amantadine is not recommended during lactation and should be used during pregnancy only if the benefits outweigh the risks.
Amantadine and rimantadine are generally well tolerated. Adverse events associated with amantadine include mild central nervous system (CNS) symptoms, eg, light-headedness, insomnia, confusion, anxiety, which are dose-related and resolve with discontinuation. In one controlled study, 13% of rimantadine recipients, in comparison with 6% of rimantadine recipients, withdrew owing to CNS adverse events.[31] Activities that require mental alertness, eg, hazardous activities and driving, should be avoided until a patient has been on amantadine for several days. Both agents have been reported to aggravate underlying seizure disorders. Occasionally, amantadine can exacerbate congestive heart failure. Increased atropine-like effects may occur if amantadine is given concurrently with anticholinergic drugs.
The Undervaccination Problem
Only 55% of persons 65 years of age and older reported receiving influenza vaccine in 1994.[32] Vaccination levels are even lower in persons less than 65 years of age with high-risk medical conditions (CDC: unpublished data). Vaccination rates are also lower in African-americans and persons below the poverty level. Influenza vaccination rates for high-risk patients in practices without specific interventions to improve compliance are often low (eg, 4% to 28%).[2,33-36] Close contacts of persons at high risk for complications and medical personnel are often inadequately immunized. In one Veterans Affairs Hospital study, only 24% of staff physicians and 4% of postgraduate trainees reported that they had been vaccinated the previous year.[29] In an outbreak in a Veterans Affairs institution and 118 staff members (including 74 nurses, 8 staff physicians, and 13 residents) became ill.[28] Most of the infections in patients were likely acquired nosocomially, either from other patients or staff.[28]
Strategies for Implementing Influenza Vaccine Recommendations
Successful vaccination programs have combined education for health care workers, publicity and education targeted at potential recipients, a plan for identifying persons at high risk (usually by medical-record review), and efforts to remove administrative and financial barriers that prevent persons from receiving the vaccine. Since Medicare started providing coverage in 1993 for influenza vaccination, the financial barriers for elderly persons have been greatly reduced. Settings for influenza vaccination programs, and strategies for each, are described below.
Office Procedures to Improve Vaccination Compliance
The most important procedures to improve vaccination rates are (1) assessment of the practice's vaccination rates, (2) identification of target populations for vaccination, (3) formation of a specific goal (ie, percentage of target population to be immunized), (4) development of a plan of action, and (5) provision of ongoing feedback to the individual physicians about vaccination rates of their own patients. Buffington et al[37] achieved a 30% increase in influenza vaccination rates in intervention practices over control practices (50% to 66%, P [is less than].001). Interventions were weekly feedback on influenza vaccination rates (weekly total and cumulative total) to physicians and the graphing of these results on an office chart (Figure 2). The impact of assessment of vaccination rates and feedback to physicians cannot be overestimated; they are among the most important changes that predict improvement in vaccination rates in ambulatory settings.
Other proactive office procedures that can increase compliance with vaccinations are: (1) Ask office staff to routinely evaluate the vaccination status of patients prior to the physician seeing the patient. This can be done at the time of registration (perhaps with the aid of a computer) or by nursing personnel when they obtain vital signs. Colored stickers, checklists, or inked rubber stamps are practical ways to communicate the need for vaccinations. (2) Send reminder postcards in the fall to encourage yearly influenza vaccination. (3) Use of a team approach in which nurses, not physicians, administer influenza vaccine. (4) Write standing orders to allow nurses to administer influenza vaccine without needing to get a new order for each patient.[38] (5) Provide information pamphlets about influenza. The pamphlet should state that the vaccine itself cannot cause influenza and that the current vaccines cause fewer adverse events than older ones. (6) Display posters in the waiting room about influenza vaccine; these are available from professional organizations such as the American Lung Association. (7) For large practices, establish "walk-in" influenza vaccination stations in the busiest clinic areas during November.[39,40] The stations should operate according to a written protocol and be staffed by nursing personnel who have received appropriate training about vaccinations. These office practices are also applicable to hemodialysis centers, specialty clinics, and travel clinics. Gyorkos et al[41] conducted an analysis of influenza vaccination strategies and found that system-oriented strategies, eg, standing orders for nurses, were the most powerful; the pooled vaccination rate increase was 39% (95% confidence interval of 30% to 49%). The client-oriented strategies, eg, postcard reminders, and provider-oriented strategies, eg, chart reminders, resulted in vaccination rate increases of 12% and 18%, respectively.
Increasing Vaccination in Nursing Homes and Other Residential Long-term
Care Facilities
Vaccination should be routinely provided to all residents of chronic-care facilities with the concurrence of attending physicians rather than by obtaining individual vaccination orders for each patient. Consent for vaccination should be obtained from the resident or a family member at the time of admission to the facility, and all residents should be vaccinated at one time, immediately preceding the influenza season.
Influenza Vaccination at Hospital Discharge
Many (39% to 82% depending on the age group and study) of those who die of influenza and pneumonia were hospitalized within the preceding year or vaccination season.[42,43] This suggests that hospitalization may be a marker for increased risk for a serious influenza infection. Hence, persons discharged from a hospital between September and March should be offered influenza vaccine. Fedson has shown that a hospital-based influenza vaccination program carried out according to a specific protocol by nurses and ward secretaries can be effective in increasing influenza immunization rates.[44]
Vaccinating Health Care Workers
Administrators of all health care facilities should offer influenza vaccine to all personnel before the influenza season. Particular emphasis should be placed on vaccination of persons who care for members of high-risk groups, eg, staff of intensive-care units, and employees of nursing homes. Using a mobile cart to take vaccine to hospital wards or other work sites and making vaccine available during night and weekend work shifts can enhance compliance.
Influenza Vaccination Strategies for Other Settings
Unvaccinated residents/attendees of retirement communities and recreation centers should be offered vaccine on site before the influenza season. Other settings or situations for implementing influenza vaccination include facilities that provide episodic or acute care (eg, urgent care centers), outpatient facilities providing continuing care to high-risk patients (eg, dialysis centers), home care providers (eg, visiting nurses), and travel clinics.
Thought Problems
Scenario 1 Florence Smith, a 45-year-old, presents to the emergency department complaining of cough productive of yellow sputum, pleuritic chest pain, generalized myalgia, chills, and fever. Her symptoms started 9 days ago with pharyngitis, cough, myalgia, and fever, at which time her primary care physician diagnosed influenza; influenza was occurring in the community. Subsequently, her symptoms improved. However, yesterday her symptoms worsened and the cough became productive. Her vaccination record reveals that she received adult tetanus and diphtheria toxoids (Td) 5 years ago. She has diabetes mellitus. Vital signs today disclosed a temperature of 39.2 [degrees] C (102.6 [degrees] F) and respirations of 27 per minute. She has labored respirations and rales in the right mid-lung field. Arterial blood gas results reveal hypoxemia. See Figure 3 for her chest x-ray film and Figure 4 for her sputum Gram stain.
Thought Problems
1. What is the differential diagnosis for her chief complaint? What are the common organisms? 2. Which diagnostic tests are needed? 3. What treatment is needed and where should it be administered? 4. Was the diagnosis of influenza appropriate? 5. Should Ms Smith have received influenza vaccine? If so, what time of year should it be administered?
Scenario 2 Jonathan, a 5-year-old with asthma, has a cough, fever, and clear rhinorrhea. He attends kindergarten. Two days after Jonathan's illness started, his 31-year-old father acquired symptoms of cough, fever, generalized myalgia, sore throat, and headache. Jonathan's 70-year-old grandmother, who takes care of him twice per week, now has a cough and fever, 3 days after taking care of him. His grandmother had an uneventful cholecystectomy 1 month ago December) and is being seen by her physician every 3 months for hypertension.
Thought Problems 6. Are their diseases related? 7. Were these cases preventable? 8. a. Where was influenza most likely to have been contracted initially? b. What age group has the highest age-specific attack rate? 9. Jonathan's grandmother is being seen by her primary care physician 1 day after her cough started. Should any treatment be given?
Scenario 3 Last winter, Poneyville experienced an influenza epidemic with increased pneumonia hospitalizations and deaths in comparison with levels seen in previous winters. Dr Ford, a primary care physician in Poneyville, was assigned the hospital duties for his practice. One of the practice's faithful patients died after being admitted for staphylococcal pneumonia following influenza. Because Dr Ford wished to prevent influenza from occurring in other patients in the practice, he requested that a chart audit of influenza vaccine coverage be conducted (Figure 5).
Thought Problems 10. Was the chart audit important? How good is the influenza vaccination coverage in the practice? 11. Why is the vaccination coverage suboptimal? 12. What can be done to improve influenza vaccination rates, given that this is a busy practice with several different providers?
Scenario 4 Mrs Gaither, a 68-year-old, is in your office because her husband was hospitalized yesterday for complications of influenza (type A). Mrs Gaither has chronic renal failure and has not received any vaccinations this year. She recalls a friend who had "a bad case of flu" following influenza vaccination. She has a history of urticaria following exposure to duck feathers, but she does eat eggs. Currently, she suffers from allergic rhinitis. Her mother has a history of clonic-tonic (grand mal) convulsions.
Thought Problems 13. What treatment should Mrs Gaither receive? 14. Can influenza vaccine cause "flu"? 15. Given that she has an allergy to duck feathers, should she receive influenza vaccine? 16. What are the side effects of amantadine and rimantadine? 17. Which groups of patients have the highest influenza fatality rates?
Scenario 5 Rufus Cook, an otherwise healthy 35-year-old, developed a cough, myalgia, and fever yesterday. His physician, Dr A-M. Bradley, diagnosed influenza this morning. Influenza type A is in the community. This afternoon, Dr Bradley received a fax from Mr Cook's employer, Crestview Care Center, a nursing home (Figure 6). After reading the fax, Dr Bradley called Crestview Care Center and found that five residents had developed symptoms consistent with influenza.
Thought Problems 18. What can be done for Mr Cook? When can he return to work? 19. What should be done for the nursing home residents and other employees with whom Mr Cook was working? 20. Could this episode have been prevented?
Scenario 6 Scott is a 19-month-old with chronic lung disease caused by premature birth. He is in the office today (November) for a well-child care visit. He has received three doses of live oral poliovirus vaccine (OPV), three doses of diphtheria and tetanus toxoids and pertussis vaccine (DTP), four doses of Haemophilus influenzae type b (HIB) conjugate vaccine, and three doses of hepatitis B vaccine.
Thought Problems 21. Does Scott need influenza vaccination? 22. Given that Scott has never received influenza vaccine, if he were to be vaccinated, how many doses would he need? What type of vaccine should he receive? 23. Can influenza vaccine be administered simultaneously with other vaccines? 24. Do any of Scott's contacts need influenza vaccine?
ANSWERS TO THOUGHT PROBLEMS
Scenario 1 1. This case represents secondary bacterial pneumonia following influenza; the differential diagnosis includes primary bacterial pneumonia and spread of an initial bacterial infection of the upper respiratory tract to the lungs. Common organisms include Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus. 2. A blood culture and a culture of a good sputum sample are needed. Streptococcus and Staphylococcus are gram-positive cocci; gram-positive cocci are shown in Gram stain (Figure 4). 3. This patient needs hospitalization and supplemental oxygen administration. She needs to be treated quickly, ie, in the emergency department, with intravenous antibiotics. 4. Influenza can be diagnosed appropriately upon clinical grounds as long as influenza is known to be occurring in the community. Her physician could also have used rapid antigen detection methods to diagnose influenza A infection. 5. Yes, diabetes mellitus is an important indication for influenza vaccination. The optimal time for influenza vaccination is typically October to mid-November, before the peak of the influenza season. Vaccine should be offered up to and even after influenza activity is documented in a community, which has been as late as April in some years.
Scenario 2 6. Yes, these are all manifestations of influenza. Influenza has different clinical presentations, depending upon the age of the patient (Table 1). The incubation period for influenza is 1 to 5 days, which is consistent with the scenario. 7. Persons with chronic respiratory disease, such as asthma, should be vaccinated against influenza. The Advisory Committee on Immunization Practices (ACIP) recommends vaccinating persons who could transmit influenza to high-risk persons, such as household members in families with an asthma patient. All persons age 65 or older should receive influenza vaccine. Hence, influenza was potentially preventable in all three persons. Chronic-care visits (eg, hypertension visit for Jonathan's grandmother) and hospital discharge (eg, following cholecystectomy) are important but often overlooked opportunities to administer vaccinations. 8. a. Jonathan most likely contracted influenza in kindergarten. b. School-aged children have the highest age-specific attack rate and are the primary transmission route for influenza. Since most are healthy, they suffer relatively few serious complications. However, they can transmit it to elderly adults, who have a higher complication rate. Vaccination of school-aged children has prevented an influenza outbreak (Monto AS, Davenport FM, Napier JA, Francis T Modification of an outbreak of influenza in Tecumseh, Michigan by vaccination of schoolchildren. J Infect Dis 1970; 122:16-25). 9. Rimantadine or amantadine can be given therapeutically to persons who contract influenza type A, provided that either drug is started within 48 hours of the onset of symptoms. They are effective only against influenza type A. Central nervous system (CNS) side effects can occur with either drug and are more likely in the elderly. Rimantadine has been documented to cause fewer CNS side effects than does amantadine.
Scenario 3 10. Assessment, ie, the chart audit, is very important. The problem must be quantified before meaningful, well-informed action will occur. The vaccine coverage rates are poor; the values given are typical for many practices. 11. Possible reasons for low vaccination rates follow:
a. Some physicians and staff underestimate disease severity and infectiousness.
b. Physicians do not realize that Medicare reimburses for influenza vaccination.
c. Most physicians have not done quality assurance studies about vaccine coverage in their practice; hence, they do not realize that vaccination rates are low.
d. Missed opportunities occur when physicians forget to address influenza vaccination when there is an opportunity, eg, acute and chronic care visits and hospital discharge.
e. Physicians use invalid vaccine contraindications, such as mild acute illnesses.
f. Vaccination indications based on occupation and chronic medical conditions are often overlooked.
g. Patients may not realize their need for vaccination.
h. Some patients are uncertain or fearful of adverse events following vaccination. 12. Vaccination rates can be improved by the following:
a. Setting a target vaccination rate for the practice and monitoring progress; this is one of the most powerful interventions.
b. Comparing vaccination rates of different practices in a competitive spirit and awarding prizes for the highest rates.
c. Sending postcard reminders to patients or using an autodialing machine to deliver telephone messages about needed vaccinations.
d. Having office staff inquire about vaccination status at registration or during measurement of vital signs. Colored stickers, checklists, or inked rubber stamps help to communicate the information.
e. Placing computer-generated "tickler" reminders on patient charts.
f. Displaying vaccination posters and pamphlets in the office waiting room.
g. Issuing standing orders for the nurse to administer influenza vaccine according to a protocol, without the need for an individual physician order for each patient. An office nurse can deliver vaccination services during influenza vaccine season, allowing a patient to receive vaccinations without seeing a physician.
h. Writing standing orders for nursing homes to vaccinate all patients.
i. During the late fall, opening an influenza vaccination clinic that is staffed by nurses.
j. Participating in mass media campaigns or public service announcements (as a benefit to the practice, these may provide free publicity).
Scenario 4 13. Mrs Gaither should receive an influenza antiviral agent (rimantadine or amantadine) and influenza vaccination. Rimantadine or amantadine should be administered for 2 weeks, until antibodies develop from influenza vaccine. Mrs Gaither has chronic renal failure, which is an indication for vaccination. Vaccination is also indicated because of her age ([greater than or equal to] 65 years). Because influenza is in the community, she is at risk for influenza and should be vaccinated even though antiviral agents may protect her from her husband's infection. Because she has chronic renal failure, the dose of amantadine or rimantadine needs to be reduced if her creatinine clearance is [less than or equal to] 50 mL/min/1.73 [m.sup.2] or [less than or equal to] 10 mL/min, respectively. Rimantadine and amantadine are effective only for treatment or prophylaxis of influenza type A infections. 14. Influenza vaccine cannot cause influenza or "flu" because it is inactivated. In adults, systemic symptoms following influenza vaccination are similar to those of placebo injection.[26] 15. Allergy to duck feathers, allergic rhinitis, and a family history of convulsions are not valid contraindications to influenza vaccination. However, anaphylaxis to influenza vaccine and severe egg allergies are valid contraindications. Acute febrile illness is a valid reason to postpone vaccination temporarily. 16. The side effects of influenza antiviral agents are: increased risk of seizures in persons with a seizure disorder, CNS effects (nervousness, anxiety, lightheadedness, difficulty concentrating, agitation, delirium, hallucinations, and marked behavioral changes), and gastrointestinal side effects (nausea and anorexia). CNS side effects occur more frequently with amantadine than rimantadine. Because both drugs are renally excreted, dosage reductions are needed in the elderly and in persons with renal insufficiency. In addition, rimantadine is metabolized in the liver; hence, persons with severe liver disease need a reduced dose. 17. Persons 65 years of age or older with two or more high-risk medical conditions (eg, diabetes mellitus, chronic lung disease, hemodynamically significant cardiac disease, chronic renal disease) have the highest fatality rates from influenza (Table 2).
Scenario 5 18. Mr Cook can receive amantadine or rimantadine as ther-apy for 3 to 5 days. He can return to work when he is no longer contagious and is off antiviral therapy For adults, the period of communicability is usually 3 to 5 days from the onset of clinical illness. 19. Influenza is highly contagious, particularly in closed environments such as nursing homes. All the nursing home residents are at risk because of Mr Cook and should receive amantadine or rimantadine for 2 weeks as part of outbreak control regardless of their vaccination status. All residents who become ill should be isolated until symptoms improve in order to help control the outbreak and decrease the risk of spreading drug-resistant virus that might develop. If any nursing home residents have not already received influenza vaccination, they should receive it now. Antibody production following vaccination takes up to 2 weeks. Hence, it will not protect residents who were exposed to Mr Cook, but it may limit transmission within the nursing home and from outside sources. Antiviral prophylaxis should be considered for unvaccinated staff. If the influenza strain is not similar to that in the vaccine, all staff should consider taking an antiviral agent for prophylaxis. 20. The entire episode could have been prevented or limited in the following ways: (1) Medical personnel and others in contact with high-risk persons should receive influenza vaccine on a yearly basis as part of standard protocol. (2) The nursing home should implement a standard protocol wherein all residents are vaccinated each year unless they have a valid contraindication. For instance, part of standard admission orders could include influenza vaccine administration in the fall. (3) The nursing home should have a contingency plan for prompt administration of an influenza antiviral agent in the event of an outbreak.
Scenario 6 21. Scott needs influenza vaccination. Anecdotal evidence suggests that high-risk children are often overlooked regarding influenza vaccination. (He also needs MMR, varicella vaccine, and if the third dose of DTP was given at least 6 months ago, he needs the fourth dose of DTaP; these vaccines can be given simultaneously with influenza vaccine.) 22. Scott, as any child 6 months of age and older with a high-risk condition, should receive influenza vaccine. Children younger than 9 years old should receive two doses, 1 month apart, in the first year that they are vaccinated against influenza. In subsequent years, they should receive one dose. Children younger than 13 years old should receive the split-virus type of influenza vaccine. 23. Influenza vaccine can be administered simultaneously with other vaccines. 24. Household contacts of persons at high risk for influenza complications should receive influenza vaccine.
REFERENCES
[1.] Centers for Disease Control and Prevention. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 1996; 45(RR-5):1-24.
[2.] Barker WH. Excess pneumonia and influenza associated hospitalization during influenza epidemics in the United States, 1970-78. Am J Public Health 1986; 76:761-5.
[3.] Williams WW, Hickson MA, Kane MA, Kendal AP, Spika JS, Hinman AR. Immunization policies and vaccine coverage among adults. The risk for missed opportunities [published erratum appears in Ann Intern Med 1988; 109:3481. Ann Intern Med 1988-,108:616-25.
[4.] Chapman LE, Tipple MA, Folger SG, et al. Influenza-United States, 1988-89. MMWR 1993; 42(l):9-22.
[5.] Strassburg MA, Greenland S, Sorvillo FJ, Lieb LE, Habel IA. Influenza in the elderly: report of an outbreak and a review of vaccine effectiveness reports. Vaccine 1986; 4(1):38-44.
[6.] Meiklejohn G, Hall H. Unusual outbreak of influenza A in a Wyoming nursing home. Smith SC, Sikes RK. J Am Geriatr Soc 1987; 35(8):742-6.
[7.] Goodman RA, Orenstein WA, Munro TF, et al. Impact of influenza A in a nursing home. JAMA 1982; 247:1451-3.
[8.] Waner JL, Todd SJ, Shalaby H, Murphy P, Wall LV. Comparison of Directigen FLU-A with viral isolation and direct immunofluorescence for the rapid detection and identification of influenza A virus. J Clin Microbiol 1991; 29:479-82.
[9.] Stuart-Harris CH, Schild GC. Influenza: the virus and the disease. Littleton, Mass: Publishing Sciences Group, 1976: 98.
[10.] Kilbourne ED. Influenza. New York, NY: Plenum Medical Book Co, 1987:193.
[11.] Centers for Disease Control and Prevention. National immunization program. Epidemiology and prevention of vaccine-preventable diseases. 3rd ed. Atlanta, Ga: Centers for Disease Control and Prevention, 1996.
[12.] McBean AM, Babish JD, Warren JL. The impact and cost of influenza in the elderly. Arch Intern Med 1993; 153:2105-11.
[13.] Kent JH, Chapman LE, Schmeltz LM, Regnery HL, Cox NJ, Schonberger LB. Influenza surveillance-United States, 1991-92. MMWR 1992; 41(5):3543.
[14.] Sullivan KM, Monto AS, Longini IM Jr. Estimates of the US health impact of influenza. Am J Public Health 1993; 83:1712-16.
[15.] Glezen WP, Couch RB, Taber LH, et al. Epidemiologic observations of influenza B virus infections in Houston, Texas, 1976-1977. Am J Epidemiol 1980; 111:13-22.
[16.] Longini IM Jr, Monto AS, Koopman JS. Statistical procedures for estimating the community probability of illness in family studies; rhinovirus and influenza. Int J Epidemiol 1984; 13(1):99-106.
[17.] Monto AS, Davenport FM, Napier JA, Francis T. Modification of an outbreak of influenza in Tecumseh, Michigan by vaccination of schoolchildren. J Infect Dis 1970; 122:16-25.
[18.] Foster DA, Talsma AN, Furumoto-Dawson A, et al. Influenza vaccine effectiveness in preventing hospitalization for pneumonia in the elderly. Am J Epidemiol 1992; 136:296-307.
[19.] Fedson DS, Wajda A, Nicol JP, Hammond GW, Kaiser DL, Roos LL. Clinical effectiveness of influenza vaccine in Manitoba. JAMA 1993; 270:1956-61.
[20.] Barker WH, Mullooly JP. Effectiveness of inactivated influenza vaccine among non-institutionalized elderly persons. In: Kendal AP, Patriarc PA, eds. Options for the control of influenza. New York, NY: Alan R. Liss, 1988:169-82.
[21.] Gross PA, Hermogenes AW, Sacks HS, Lau J, Levandowski RA. The efficacy of influenza vaccine in elderly persons. A meta-analysis and review of the literature. Ann Intern Med 1995; 123:518-27.
[22.] Govaert ThME, Thijs CTMCN, Masurel N, Sprenger MJW, Dinant GJ, Knottnerus JA. The efficacy of influenza vaccination in elderly individuals. A randomized double-blind placebo-controlled trial. JAMA 1994; 272:1661-5.
[23.] Nichol KL, Margolis KL, Wuorenma J, Sternberg T. The efficacy and cost effectiveness of vaccination against influenza among elderly persons living in the community. N Engl J Med 1994; 331:778-84.
[24.] Riddiough MA, Sisk JE, Bell JC. Influenza vaccination. JAMA 1983; 249:3189-95.
[25.] Centers for Disease Control. Final results: Medicare influenza vaccine demonstration-selected states, 1988-1992. MMWR 1993; 42(31):6014.
[26.] Margolis KL, Nichols KL, Poland GA, Pluhar RE. Frequency of adverse reactions to influenza vaccine in the elderly. A randomized, placebo-controlled trial. JAMA 1990; 264:1139-41.
[27.] Schonberger LB, Bregman DJ, Sullivan-Bolyai JZ, et al. Guillain-Barre syndrome following vaccination in the National Influenza Immunization Program, United States, 1976-1977. Am J Epidemiol 1979; 110: 105-23.
[28.] Pachucki CT, Pappas SA, Fuller GF, Krause SL, Lentino JR, Schaaff DM. Influenza A among hospital personnel and patients. Implications for recognition, prevention, and control. Arch Intern Med 1989; 149:77-80.
[29.] Pachucki CT, Lentino JR, Jackson GG. Attitudes and behavior of health care personnel regarding the use and efficacy of influenza vaccine [letter]. J Infect Dis 1985; 151:1170-1.
[30.] Murphy KR, Strunk RC. Safe administration of influenza vaccine in asthmatic children hypersensitive to egg proteins. J Pediatr 1985; 106:931-3.
[31.] Dolin R, Reichman RC, Madore HP, Maynard R, Linton PN, Webber-Jones J. A controlled trial of amantadine and rimantadine in the prophylaxis of influenza A infection. N Engl J Med 1982; 307:580-4.
[32.] Centers for Disease Control and Prevention. Influenza and pneumococcal vaccination coverage levels among persons aged [greater than or equal to] 65 years-united States, 1973-1993. MMWR 1995; 44:506-7, 513-15.
[33.] Cohen DI, Littenberg B, Wetzel C, Neuhauser D. Improving physician compliance with preventive medicine guidelines. Med Care 1982; 20:1040-5.
[34.] Gelfman DM, Witherspoon JM, Buchsbaum DG, Centor RM. Short-term results of an immunization compliance program. Virginia Med 1986; 113(9):532-4.
[35.] Barton MB, Schoenbaum SC. Improving influenza vaccination performance in an HMO setting: the use of computer-generated reminders and peer comparison feedback. Am J Public Health 1990; 80:534-6.
[36.] Douglas KC, Rush DR, O'Dell M, Monroe A, Ausmus M. Adult immunization in a network of family practice residency programs. J Fam Pract 1990; 31:513-20.
[37.] Buffington J, Bell KM, LaForce FM. A target-based model for increasing influenza immunizations in private practice. Genesee Hospital Medical Staff. J Gen Intern Med 1991; 6:204-9.
[38.] Margolis KL, Lofgren RP, Korn JE. Organizational strategies to improve influenza vaccine delivery. A standing order in a general medicine clinic. Arch Intern Med 1988; 148:2205-7.
[39.] Nichol KL, Korn JE, Margolis KL, Poland GA, Petzel RA, Lofgren RP. Achieving the national health objective for influenza immunization: success of an institution-wide vaccination program. Am J Med 1990; 89:156-60.
[40.] Nichol KL. Long-term success with the national health objective for influenza vaccination: an institution-wide model. J Gen Intern Med 1992; 7:595-600.
[41.] Gyorkos TW, Tannenbaum TN, Abrahamowicz M, et al. Evaluation of the effectiveness of immunization delivery methods. Can J Public Health 1994; 85(suppl 1):S14-S30.
[42.] Fedson DS, Wajda A, Nicol JP, Roos LL. Disparity between influenza vaccination rates and risks for influenza-associated hospital discharge and death in Manitoba in 1982-1983. Ann Intern Med 1992; 116:550-5.
[43.] Barker WH, Mullooly JP. Pneumonia and influenza deaths during epidemics: implications for prevention. Arch Intern Med 1982; 142:85-9.
[44.] Fedson DS, Kessler HA. A hospital-based influenza immunization program, 1977-78. Am J Public Health 1983; 73:442-5.
The Teaching Immunization for Medical Education (TIME) Project
This article, including the thought problems that follow this section, was written as a component of the Teaching Immunization for Medical Education (TIME) Project, a multiyear project guided by a national advisory committee of experts in the fields of immunization and medical education. The project is a collaborative effort of the Centers for Disease Control and Prevention, the Association of Teachers of Preventive Medicine (ATPM), and the University of Pittsburgh School of Medicine. The goal of the project is to enhance the educational preparation of physicians through an innovative curriculum on immunization and vaccine-preventable diseases, thereby influencing the immunization practices of physicians in the effort to increase vaccination levels. Information about continuing medical education (CME) modules on other vaccine-preventable diseases and case-based materials designed for medical students and residents may be obtained by directly contacting ATPM, Suite 204, 1511 South Ritchie Highway, Arnold, MD 21012; telephone 800-789-6737, fax 800-678-7102. Some CME modules will be available at the ATPM World Wide
COPYRIGHT 1997 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group