FRANCES HUDSON, 78, is in your intensive care unit (ICU) with pneumonia and septic shock. She's mechanically ventilated and is receiving intravenous (I.V.) fluids and dopamine for blood pressure support, I.V. antibiotics, and antipyretics.
When you perform your morning assessment, you notice diffuse petechiae, hematuria, bleeding from her venipuncture site, epistaxis, and bloody stools. She also has ecchymotic areas over bony prominences. When you suction her, her sputum is blood-tinged.
What's the situation?
Shortly after Ms. Hudson was admitted to the ICU last night with pneumonia, she developed septic shock. Her vital signs were stable last night.
Her morning lab results reveal an elevated white blood cell count, hemoglobin level of 8 grams/dl, and platelet count of 50/mm^sup 3^. Her prothrombin time has increased to 20 seconds; her activated partial thromboplastin time, to 42 seconds. Her fibrinogen level is reduced, but her fibrin degradation products level is increased, and a D-dimer screen is elevated.
What's your assessment?
Ms. Hudson's sudden-onset bleeding and her abnormal lab values indicate disseminated intravascular coagulation (DIC), a condition characterized by the malfunction of clotting factors. In DIC, thrombosis occurs faster than clots can be lysed. Microthrombi cause vessel occlusion and tissue ischemia, and diffuse hemorrhaging results because clotting factors are used to form thrombi rather than combating bleeding.
Left untreated, DIC can lead to tissue ischemia and hypoxia, blood stasis, acidemia, and death. Even with treatment, the mortality rate is 50% to 80%. Potential triggers of DIC include massive trauma, neoplasms, vascular disorders, liver disease, drug reactions, and severe infections. In Ms. Hudson's case, endotoxins from bacteria breakdown in sepsis caused endothelial damage and activated the clotting cascade.
What must you do immediately?
Your interventions will focus on removing the triggering event or condition (pneumonia and septic shock), preventing and reducing tissue ischemia, and minimizing bleeding. Maintain vascular volume by providing fluid replacement, continuing to administer vasopressor medications, and continuing mechanical ventilation for respiratory support.
Observe bleeding precautions, and administer fresh frozen plasma and packed red blood cells, as ordered. Cryoprecipitate may be given if Ms. Hudson needs fibrinogen, and platelets also may be ordered. These blood products improve oxygen-carrying capacity, provide fluid volume expansion, and increase availability of clotting factors in the bloodstream.
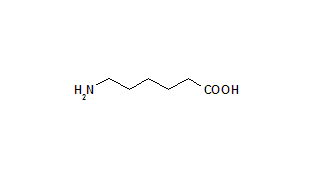
Antifibrinolytics such as aminocaproic acid (Amicar) should also be considered. Antithrombin III may be ordered to treat moderate to severe DIC when the patient's antithrombin III levels are very low.
Heparin therapy, although controversial, is another option. Heparin makes clotting factors available in the bloodstream, but because it's an anticoagulant, it can also cause more bleeding. Administer it with extreme caution.
What should be done later?
Monitor Ms. Hudson for complications of DIC, including hypovolemia, acute renal failure, infection, and acute respiratory distress syndrome.
Ms. Hudson's condition slowly improves. After 7 days in the ICU, she's stable enough to be transferred to the medical/surgical unit. Because of DIC's high mortality rate, closely monitor all high-risk patients and intervene aggressively at the first sign of trouble.
BY KATHERINE A. ATASSI, RN, CNA, OCN, MSN
MINDY L. HARRIS, RN, CNA, MSN
Instructors * West Virginia University Institute of Technology * Montgomery, W.Va.
Copyright Springhouse Corporation Mar 2001
Provided by ProQuest Information and Learning Company. All rights Reserved