Study objectives: Cardiac surgery with cardiopulmonary bypass (CPB) is associated with major inflammatory triggers that cause marked activation of the microcirculation. This inflammatory response is associated with significant organ dysfunction. How this response causes organ dysfunction is not well understood; consequently, few interventions exist to prevent or treat it. In other acute inflammatory conditions, such as sepsis, increased coagulation activation in the microcirculation may be a cause of organ injury. We documented the association between coagulation activation and organ dysfunction to investigate whether coagulation activation also plays a role in organ injury following cardiac surgery with CPB.
Design: Prospective study of 30 patients undergoing cardiac surgery with CPB. Prothromhin fragment (PTF) 1 + 2 and plasminogen activator inhibitor (PAI) activity were measured, and levels correlated with postoperative measures of organ function including the left-ventricular stroke work index, the Pa[O.sub.2]/fraction of inspired oxygen (FI[O.sub.2]) ratio, and creatinine levels.
Results: PTF levels increased eightfold (p < 0.05), and PAI activity increased threefold (p < 0.05) over the first 4 h after CPB. PTF levels were correlated with deteriorations in the left-ventricular stroke work index (p = 0.04), the Pa[O.sub.2]/FI[O.sub.2] ratio (p = 0.02), and creatinine levels (p = 0.02).
Conclusions: Levels of coagulation activation are associated with markers of postoperative organ dysfunction. Additional studies are warranted to investigate whether strategies that limit coagulation activation are associated with reductions in postoperative organ dysfunction.
Key words: cardiac surgery; disseminated-intravascular coagulation; inflammation
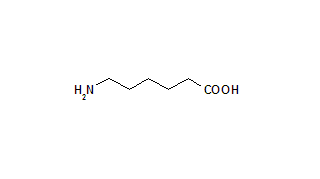
Abbreviations: CI = cardiac index; CPB = cardiopulmonary bypass; EACA = [epsilon]-aminocaproic acid; FI[O.sub.2] = fraction of inspired oxygen; LVSWI = left-ventricular stroke work index. MAP = mean arterial pressure. PAI= plasminogen activator inhibitor; PCWP = pulmonary capillary wedge pressure; PTF = prothrombin fragment. TF = tissue factor
**********
Cardiac surgery with cardiopulmonary bypass (CPB) is associated with major inflammatory triggers, including contact of blood with the bioactive surface of the bypass circuit and ischemic-reperfusion injury to the heart and lungs. (1,2) These inflammatory triggers cause marked activation of the microcirculation throughout the body. (3-11) This inflammatory response is associated with significant organ dysfunction in the immediate postoperative period. (12-14) How the inflammatory response causes organ dysfunction is not well understood; consequently, there are as yet few interventions to prevent or treat it.
Inflammation and coagulation activation are intimately linked, Inflammation up-regulates microvascular expression of tissue factor (TF), which triggers coagulation activation, and microvascular expression of plasminogen activator inhibitor (PAI)-1, which inhibits activation of fibrinolysis. Inflammation also down-regulates natural anticoagulant proteins, such as protein C, protein S, thrombomodulin, and antithrombin. (15-17) These anticoagulant proteins are particularly active at the microcirculatory level. These inflammatory responses can result in ischemic tissue injury due to microvascular thrombosis. (18-20)
Evidence from a number of studies (20-30) suggests that microvascular thrombosis may be an important mechanism through which inflammation causes organ injury. In a range of inflammatory conditions, including sepsis, multitrauma, severe hypoxia following circulatory arrest, and the hemolytic uremic syndrome, levels of coagulation activation and histologic evidence of microvascular thrombosis were both associated with the development of organ injury. Furthermore, a multicenter trial (31) of patients with severe sepsis found that the administration of activated protein C (an anticoagulant) reduced both organ injury and mortality.
Whether or not microvascular thrombosis contributes to organ dysfunction following cardiac surgery with CPB is not known. Therefore, we documented the association between coagulation activation and organ dysfunction to investigate whether coagulation activation may play a role in organ dysfunction following cardiac surgery with CPB.
MATERIALS AND METHODS
Prothrombin fragment (PTF) 1 + 2 (a marker of coagulation activation) and PAI activity (a marker of inhibition of fibrinolysis) were measured, and levels correlated with postoperative measures of organ function including the left-ventricular stroke work index (LVSWI), the Pa[O.sub.2]/fraction of inspired oxygen (FI[O.sub.2]) ratio, and creatinine levels. The Pa[O.sub.2]/FI[O.sub.2] ratio and serum creatinine levels were chosen because these markers have been widely used and validated in previous scoring systems of organ dysfunction, including both the acute physiology and chronic health evaluation and the sequential organ failure assessment scores. The LVSWI was used as our marker of cardiac function because impaired myocardial contractility is the primary cause of cardiac dysfunction after CPB. (32)
Patient Selection
We studied patients scheduled for first-time nonemergency cardiac surgery with CPB. Patients with any of the following preoperative features were excluded from the study: creatinine > 200 [micro]mol/L, bilirubin > 28 [micro]mol/L, or severe airways disease. The study was approved by the St. Vincent's Hospital Human Research Ethics Committee. All patients gave written informed consent before participation in the study.
Data Collection
PTF levels and PAI activity were measured before induction, and at 0, 1, 2, 3, and 4 h after CPB. The Pa[O.sub.2]/FI[O.sub.2] ratio was calculated before induction and at 1, 2, 3, and 4 h after CPB. The cardiac index (CI), mean arterial pressure (MAP), heart rate, pulmonary capillary wedge pressure (PCWP), and LVSWI were recorded following anesthetic induction and at 1, 2, 3, and 4 h after CPB. Creatinine levels were measured on the first, second, third, and fifth postoperative days.
Arterial samples were collected in prechilled sodium-citrate tubes (9:1, blood/anticoagulant [volume/volume]), centrifuged at 4,000 revolutions per minute for 15 min, and the plasma stored at -70[degrees]C. PTF was assayed by enzyme-linked immunoassays (Enzygnost PTF 1 + 2; Behring; Marburg, Germany). PAI activity was assessed with a functional assay that reflects the antifibrinolytic actions of PAI-1 and the fibrinolytic action of tissue plasminogen activator (Berichrom PAI; Behring). (33)
Intravascular pressures were recorded at end-expiration, using standard strain gauge pressure transducers calibrated to zero at the midaxillary line fourth intercostal space and coupled to a monitor with a calibrated screen. The cardiac output was measured by the thermodilution technique, with 10 mL of 5% glucose at room temperature. All readings were performed in triplicate, with each reading accepted if within 10% of the others. The average was recorded. A six-lumen Swan-Ganz VIP catheter was used (Baxter-Healthcare; Irvine, CA). Hemodynamic variables were calculated using a standard formula: LVSWI = (MAP - PCWP) x (CI/heart rate) x (0.0136). Chilled heparinized syringes (Terumo Corporation; Tokyo, Japan) were used to obtain arterial gases. The Pa[O.sub.2] was immediately analyzed in the ICU (Ciba-Corning Diagnostics Corporation; East Walpole, MA).
Preoperative left ventricular function was routinely assessed by either contrast ventriculogram or transesophageal echocardiography. A score was given using a scale of 1 to 5 as follows: 1, severe impairment; 2, moderate impairment; 3, mild impairment; 4, hypertrophy; and 5, normal.
Anesthesia and Surgical Management
Patients were induced with fentanyl, propofol, and pancuronium. Anesthesia was maintained with isoflurane or propofol. Patients received 5 g of [epsilon]-aminocaproic acid (EACA) IV prior to the onset of CPB and 5 g into the pump-prime. CPB was performed with a membrane oxygenator (Cobe-Cardiovascular; Arvado, CO). Patients were heparinized (initial dose, 300 U/kg) to maintain an activated clotting time using kaolin > 400 s. The pump was primed with a combination of plasmalyte, colloid, bicarbonate, and calcium chloride. A roller pump was used. On CPB, the mixed venous oxygen saturation was maintained at > 70% and MAP > 60 mm Hg. Arrest of the heart was managed using a combination of anterograde and retrograde blood cardioplegia or with cold crystalloid antegrade cardioplegia. Patients were cooled to approximately 31[degrees]C. Patients were actively rewarmed to 37[degrees]C before discontinuation of CPB.
ICU Management
MAP was maintained at 60 to 110 mm Hg. Hypotension in the setting of hypovolemia was managed with 1V normal saline solution, plasma expander, or albumin. Hypotension associated with normovolemia was managed with an ionotrope infusion. Norepinephrine was used if the CI was > 2.5 L/min/[m.sup.2], whereas epinephrine was used if the CI was < 2.5 L/min/[m.sup.2]. Hypertension was treated with infusions of glyceryl-trinitrate and/or sodium nitroprusside. Patients with an uncomplicated course were discharged on the first postoperative day to the cardiothoracic ward.
Statistical Analysis
One-way, repeated-measures analysis of variance examined variables measured repeatedly over time, if significant; the Dunnett t test was used for post hoc testing. The Spearman rank correlation examined the relationship between hemostatic markers and measures of organ function. For repeatedly measured variables, other than creatinine, the mean of the after CPB measurements was used as a summary value for this analysis. For creatinine, the maximum postoperative level was used. The Wilcoxon signed-rank test was used to compare paired data. Multivariate linear regression was used to identify whether PTF levels were independently associated with measures of organ dysfunction. Statistical analysis was performed using software (Statview, Version 5; SAS Institute; Cary, NC).
RESULTS
Patients Studied
Thirty patients were studied. Baseline patient characteristics are shown in Table 1. Their average age was 67 years (63% were male), and baseline left ventricular function was well preserved. One patient was administered preoperative IV heparin. This patient also received aspirin 4 days before surgery. No other patient received preoperative aspirin, heparin, warfarin, or a nonsteroidal antiinflammatory drug. All patients were in sinus rhythm at baseline. Eleven patients required cardiac pacing during the initial 4 h of postoperative observation. The remainder were in sinus rhythm during this period. All patients survived to hospital discharge. Operative and postoperative characteristics are shown in Table 2.
PTF
The peak PTF level, 1 h after CPB, of 6.8 nmol/L was eightfold above baseline levels. Thereafter, levels fell but remained above baseline throughout the 4 h of observation (p < 0.05, Dunnett t test; Fig 1).
[FIGURE 1 OMITTED]
PAI Activity
In contrast to PTF, PAI activity showed a delayed increase from 1 h after CPB (p < 0.05, Dunnett t test). The peak level of 7.7 U/mL was threefold above baseline levels. This was reached at 3 h after CPB (Fig 1).
LVSWI and Other Hemodynamic Variables
The LVSWI fell after CPB. The nadir of 27 g/m/[m.sup.2] at 4 h after CPB was 50% below the baseline level of 54 g/m/[m.sup.2] (p < 0.05, Dunnett t test; Fig 2). The CI initially fell below baseline levels after CPB. The nadir of 2.5 L/min/[m.sup.2] was reached at 2 h after CPB (p < 0.05, Dunnett t test). The heart rate increased and remained between 82 and 86 beats/ min after CPB (p < 0.05, Dunnett t test). The MAP remained significantly below baseline levels at all time points after CPB (p < 0.05, Dunnett t test). PCWP levels did not change significantly from baseline levels.
The total fluid balance at 16 h after CPB was 1.7 L positive. Intraoperative milrinone and epinephrine were used in 16% and 23% of patients, respectively. Postoperative epinephrine and norepinephrine were used in 20% and 16% of patients, respectively.
Pa[O.sub.2]/FI[O.sub.2] Ratio
The Pa[O.sub.2]/FI[O.sub.2] ratio fell from 376 mm Hg at baseline (prior to intubation) to 287 mm Hg at 1 h after CPB (p < 0.05, Dunnett t test). Levels remained low throughout the 4 h of observation (Fig 2).
[FIGURE 2 OMITTED]
Creatinine Levels
The maximum creatinine level over the first 5 postoperative days was 109 [micro]mol/L. This level was significantly higher than the baseline level of 95 [micro]mol/L (p < 0.05, Wilcoxon signed-rank test; Fig 3).
[FIGURE 3 OMITTED]
Hemostatic Markers and Organ Function
The correlations between hemostatic markers and measures of organ function are shown in Table 3 and Figure 4. PTF levels were correlated with the LVSWI (p = 0.04; [rho] = -0.39), Pa[O.sub.2]/FI[O.sub.2] ratio (p = 0.02; [rho] = -0.43), and creatinine levels (p = 0.02; [rho] = 0.45). PAI activity was not correlated with any measures of organ function.
Multivariate Regression:
The association between the LVSWI and PTF levels was similar (p = 0.07) after adjusting for preoperative LVSWI levels and postoperative ionotrope use. The association between the Pa[O.sub.2]/FI[O.sub.2] ratio and PTF levels was the same (p = 0.02) after adjusting for preoperative Pa[O.sub.2]/FI[O.sub.2] levels and postoperative PCWP levels. The association between postoperative creatinine levels and PTF was also similar
DISCUSSION
Cardiac surgery with CPB is associated with major inflammatory triggers including contact of blood with the foreign surface of the bypass circuit and ischemic-reperfusion injury to the heart and lungs. (1,2) These insults activate the microcirculation throughout the body, (3-11) and this results in organ dysfunction in the immediate postoperative period. (12-14) Microvascular activation may cause organ dysfunction due to microvascular thrombosis. Inflammation upregulates microvascular expression of TF, which triggers coagulation activation, and microvascular expression of PAI-1, which inhibits fibrinolysis activation. (18-20)
We found that coagulation activation increased markedly following cardiac surgery with CPB. The peak PTF level of 6.7 nmol/L, at 1 h after CPB, was eightfold above baseline levels. The extent of the increase in PTF levels was remarkable in view of the anticoagulant/anti-inflammatory interventions undertaken, including high-dose heparin (approximately 300 U/kg) and hypothermia.
PAI activity initially fell after CPB, but not to a statistically significant extent. PAI activity is a functional assay that reflects the antifibrinolytic actions of PAI-1 and the fibrinolytic action of tissue plasminogen activator. The release of tissue plasminogen activator, following activation of endothelial cells during CPB, is therefore likely to be the cause of this initial fall. (34,35) Hemodilution is also likely to contribute to this fall. From 1 h after CPB, PAI activity increased and peaked from 3 h after CPB, threefold above baseline levels. All patients received 10 g of the antifibrinolytic agent EACA at the start of the operation. EACA was unlikely to be a factor in the increase in PAI activity. This assay does not reflect the actions of EACA (unpublished observations). The increase in PAI activity is therefore likely to reflect increased PAI-1 levels, indicating marked endogenous inhibition of fibrinolysis activation. This conclusion is consistent with previous studies that demonstrated increased PAI-1 levels after CPB. (34,35)
The magnitude and temporal changes in these hemostatic markers were similar to those found in other acute inflammatory conditions associated with microvascular thrombosis and organ injury, such as sepsis and the hemolytic uremic syndrome. (21,27,36-39) Levels of coagulation activation were also correlated with acute deteriorations, in the immediate postoperative period, in markers of organ function including the LVSWI, the Pa[O.sub.2]/FI[O.sub.2] ratio, and creatinine levels. These findings raise the possibility that microvascular thrombosis may play a role in organ dysfunction following cardiac surgery with CPB.
Previous studies suggest that ischemic tissue injury due to microvascular thrombosis may be an important mechanism through which the acute inflammatory response causes organ injury. Histologic studies (19,20,40,41) in patients with sepsis demonstrated microvascular thrombosis associated with significant isehemic organ injury. Angiographic studies (42,43) in patients with the ARDS demonstrated extensive microvascular obstruction, which improved following the administration of thrombolyties. Furthermore, as mentioned in the introduction, the administration of activated protein C (an anticoagulant) in patients with severe sepsis significantly reduced both organ failure and mortality. (31)
Myocardial and pulmonary ischemic-reperfusion injury is one of the major inflammatory triggers associated with cardiac surgery with CPB. (44,45) There is evidence that microvascular thrombosis may also contribute to organ injury associated with this aseptic inflammatory trigger. Previous studies (2,27,34,46-48) in humans demonstrated that isehemic-reperfusion injury was one of the major triggers of coagulation activation, whereas surgical trauma associated with sternotomy or thoracotomy had little impact. In animal models of myocardial ischemic-reperfusion injury, microsphere techniques demonstrated a progressive obstruction to microvascular blood flow over the first 2 h following reperfusion. (49) In these animal models, the administration of inhibitors of coagulation or thrombolytic agents reduced microvascular obstruction and myocardial dysfunction. (49-52) Similar findings were demonstrated in animal models of pulmonary ischemic-reperfusion injury. (53) In a rabbit model of CPB, extensive thrombus formation was found in small-sized pulmonary arteries at 4 h after CPB. In this study, animals treated with an infusion of a thrombin inhibitor had reductions in both thrombus formation and pulmonary vascular resistance. (54)
One human study (55) also supports a role for microvascular thrombosis. This study reported the autopsy findings in patients who had undergone thoracic aortic aneurysm repair with CPB and hypothermic arrest. Microvascular thrombi were found in a number of organs including the heart, lungs, adrenals, and kidneys. The thrombi in the renal cortical arterioles and the glomerular capillaries were associated with renal cortical infarction.
Our study has a number of limitations. It was relatively small. Consequently, although we found significant correlations between PTF levels and markers of organ dysfunction, the correlation coefficients were relatively weak. The [r.sup.2] values for these correlation coefficients indicate that PTF levels only explained approximately 16% of the variation in postoperative creatinine, Pa[O.sub.2]/FI[O.sub.2], and LVSWI levels. These relatively weak associations do not, however, necessarily indicate that organ injury due to microvascular thrombosis is not an important mechanism. PTF levels are a surrogate marker of microvascular thrombosis and therefore are unlikely to perfectly reflect levels of microvascular thrombosis. Furthermore, even if microvascular thrombosis only contributes to 16% of the deterioration in organ function, this is still a clinically important level, particularly because this mechanism is potentially preventable or reversible.
Finally, although we demonstrated correlations between coagulation activation and postoperative organ dysfunction, these correlations alone cannot prove causation. Other mechanisms may explain these associations. It is possible that organ injury results from other inflammatory mechanisms, and PTF levels merely reflect the magnitude of the underlying acute inflammatory response. These potential mechanisms include tissue edema and the release of reactive oxygen species and proteolytic enzymes by leukocytes.
CONCLUSION
We found marked increases in coagulation activation and inhibition of fibrinolysis following cardiac surgery with CPB. Levels of coagulation activation were associated with deteriorations in cardiac, pulmonary, and renal functions. Additional studies are warranted to investigate whether strategies that limit coagulation activation are associated with reductions in postoperative organ dysfunction.
REFERENCES
(1) Chandler WL, Velan T. Estimating the rate of thrombin and fibrin generation in vivo during cardiopulmonary bypass. Blood 2003; 101:4355-4362
(2) Mariani MA, Gu YJ, Boonstra PW, et al. Proeoagulant activity after off-pump coronary operation: is the current anticoagulation adequate? Ann Thorac Surg 1999; 67:1370-1375
(3) Ascione R, Lloyd CT, Underwood MJ, et al. On-pump versus off-pump coronary revascularization: evaluation of renal function. Ann Thorac Surg 1999; 68:493-498
(4) Cox CS, Allen sJ, Brennan M. Analysis of intestinal microvascular permeability associated with cardiopulmonary bypass. J Surg Res 1999; 83:19-26
(5) Raijmakers PG, Groeneveld AB, Schneider AJ, et al. Transvascular transport of 67Ga in the lungs after cardiopulmonary bypass surgery. Chest 1993; 104:1825-1832
(6) Dewanjee MK, Wu SM, Burke GW 3rd, et al. Tumor necrosis factor-[alpha] in plasma during cardiopulmonary bypass in a pig model: correlation with marginated neutrophils and cerebral edema by magnetic resonance imaging. ASAIO J 1998; 44:212-218
(7) Anderson RE, Li TQ, Hindmarsh T, et al. Increased extracellular brain water after coronary artery bypass grafting is avoided by off-pump surgery. J Cardiothorac Vasc Anesth 1999; 13:698-702
(8) Eberhardt F, Mehlhorn U, Larose K, et al. Structural myocardial changes after coronary artery surgery. Eur J Clin Invest 2000; 30:938-946
(9) Dreyer WJ, Burns AR, Phillips SC, et al. Intercellular adhesion molecule-1 regulation in the canine lung after cardiopulmonary bypass. J Thorac Cardiovasc Surg 1998; 115:689-698
(10) Massoudy P, Zalfler S, Becker BF, et al. Significant leukocyte and platelet retention during pulmonary passage after declamping of the aorta in CABG patients. Eur J Med Res 1999; 4:178-182
(11) Dreyer WJ, Michael LH, Millman EE, et al. Neutrophil sequestration and pulmonary dysfunction in a canine model of open heart surgery with cardiopulmonary bypass: evidence for a CD18-dependent mechanism. Circulation 1995; 92: 2276-2283
(12) Tassani P, Richter JA, Barankay A, et al. Does high-dose methylprednisolone in aprotinin-treated patients attenuate the systemic inflammatory response during coronary artery bypass grafting procedures? J Cardiothorac Vasc Anesth 1999; 13:165-172
(13) Kilger E, Weis F, Briegel J, et al. Stress doses of hydrocortisone reduce severe systemic inflammatory response syndrome and improve early outcome in a risk group of patients after cardiac surgery. Crit Care Med 2003; 31:1068-1074
(14) Fitch JC, Rollins S, Matis L, et al. Pharmacology and biological efficacy of a recombinant, humanized, single-chain antibody C5 complement inhibitor in patients undergoing coronary artery bypass graft surgery with cardiopulmonary bypass. Circulation 1999; 100:2499-2506
(15) Nawroth PP, Stern DM. Modulation of endothelial cell hemostatic properties by tumor necrosis factor. J Exp Med 1986; 163:740-745
(16) Schleef RR, Loskutoff DJ. Fibrinolytic system of vascular endothelial cells. Role of plasminogen activator inhibitors. Haemostasis 1988; 18:328-341
(17) Esmon CT. Inflammation and thrombosis. J Thromb Haemost 2003; 1:1343-1348
(18) Shibayama Y. Sinusoidal circulatory disturbance by microthrombosis as a cause of endotoxin-induced hepatic injury. J Pathol 1987; 151:315-321
(19) Ivanyi B, Thoenes W. Microvascular injury and repair in acute human bacterial pyelonephritis. Virchows Arch A Pathol Anat Histopathol 1987; 411:257-265
(20) Yoshikawa T, Tanaka KR, Guze LB. Infection and disseminated intravascular coagulation. Medicine 1971; 50:237-258
(21) Mesters RM, Mannucci PM, Coppola R, et al. Factor VIIa and antithrombin III activity during severe sepsis and septic shock in neutropenic patients. Blood 1996; 88:881-886
(22) Gando S, Kameue T, Nanzaki S, et al. Participation of tissue factor and thrombin in posttraumatic systemic inflammatory syndrome. Crit Care Med 1997; 25:1820-1826
(23) Menges T, Hermans PW, Little SG, et al. Plasminogen-activator-inhibitor-1 4G/5G promoter polynaorphism and prognosis of severely injured patients. Lancet 2001; 357: 1096-1097
(24) Gando S, Nakanishi Y, Tedo I. Cytokines and plasminogen activator inhibitor-1 in posttrauma disseminated intravascular coagulation: relationship to multiple organ dysfunction syndrome. Crit Care Med 1995; 23:1835-1842
(25) Geppert A, Zorn G, Delle-Karth G, et al. Plasminogen activator inhibitor type 1 and outcome after successful cardiopulmonary resuscitation. Crit Care Med 2001; 29:1670-1677
(26) Gando S, Kameue T, Nanzaki S, et al. Massive fibrin formation with consecutive impairment of fibrinolysis in patients with out-of-hospital cardiac arrest. Thromb Haemost 1997; 77:278-282
(27) Chandler WL, Jelacic S, Boster DR, et al. Prothrombotic coagulation abnormalities preceding the hemolytic-uremic syndrome. N Engl J Med 2002; 346:23-32
(28) Kaufman HH, Hui KS, Mattson JC, et al. Clinicopathological correlations of disseminated intravascular coagulation in patients with head injury. Neurosurgery 1984; 15:34-42
(29) Mehta B, Briggs DK, Sommers SC, et al. Disseminated intravascular coagulation following cardiac arrest: a study of 15 patients. Am J Med Sci 1972; 264:353-363
(30) Inward CD, Howie AJ, Fitzpatrick MM, et al. Renal histopathology in fatal cases of diarrhoea-associated haemolytic uraemic syndrome. British Association for Paediatric Nephrology. Pediatr Nephrol 1997; 11:556-559
(31) Bernard GR, Vincent JL, Laterre PF, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 2001; 344:699-709
(32) Roberts AJ, Spies SM, Sanders JH, et al. Serial assessment of left ventricular performance following coronary artery bypass grafting: early postoperative results with myocardial protection afforded by multidose hypothermic potassium crystalloid cardioplegia. J Thorac Cardiovasc Surg 1981; 81:69-84
(33) Chiu WC, Gann DS, Darlington DN. Measuring plasminogen activator inhibitor activity in plasma by two enzymatic assays. J Biochem Biophys Methods 2000; 45:127-140
(34) Grossmann R, Babin-Ebell J, Misoph M, et al. Changes in coagulation and fibrinolytic parameters caused by extracorporeal circulation. Heart Vessels 1996; 11:310-317
(35) Ray MJ, Marsh NA. Aprotinin reduces blood loss after cardiopulmonary bypass by direct inhibition of plasmin. Thromb Haemost 1997; 78:1021-1026
(36) van Deventer SJ, Buller HR, ten Cate JW, et al. Experimental endotoxemia in humans: analysis of cytokine release and coagulation, fibrinolytic, and complement pathways. Blood 1990; 76:2520-2526
(37) de Jonge E, Dekkers PE, Creasey AA, et al. Tissue factor pathway inhibitor dose-dependently inhibits coagulation activation without influencing the fibrinolytic and cytokine response during human endotoxemia. Blood 2000; 95:1124-1129
(38) Gando S, Nanzaki S, Sasaki S, et al. Activation of the extrinsic coagulation pathway in patients with severe sepsis and septic shock. Crit Care Med 1998; 26:2005-2009
(39) Mesters RM, Florke N, Ostermann H, et al. Increase of plasminogen activator inhibitor levels predicts outcome of leukocytopenic patients with sepsis. Thromb Haemost 1996; 75:902-907
(40) Kojima M, Shimamura K, Mori N, et al. A histological study on microthrombi in autopsy cases of DIC. Bibl Haematol 1983; 49:95-106
(41) Powell D. Non-suppurative lesions in staphylococcal septicaemia. J Path Bacteriol 1961; 82:141-149
(42) Greene R, Lind S, Jantsch H, et al. Pulmonary vascular obstruction in severe ARDS: angiographic alterations after i.v. fibrinolytic therapy. AJR Am J Roentgenol 1987; 148:501-508
(43) Jantsch H. Incidence and prognostic significance of pulmonary artery thromboses in patients with acute respiratory failure. Wien Klin Wochenschr Suppl 1989; 179:3-15
(44) Penttila HJ, Lepojarvi MV, Kiviluoma KT, et al. Myocardial preservation during coronary surgery with and without cardiopulmonary bypass. Ann Thorac Surg 2001; 71:565-571
(45) Chai PJ, Williamson JA, Lodge AJ, et al. Effects of ischemia on pulmonary dysfunction after cardiopulmonary bypass. Ann Thorac Surg 1999; 67:731-735
(46) Slaughter TF, LeBleu TH, Douglas JM Jr, et al. Characterization of prothrombin activation during cardiac surgery by hemostatic molecular markers. Anesthesiology 1994; 80:520-526
(47) Hunt BJ, Parratt RN, Segal HC, et al. Activation of coagulation and fibrinolysis during cardiothoracic operations. Ann Thorac Surg 1998; 65:712-718
(48) Casati V, Gerli C, Franco A, et al. Activation of coagulation and fibrinolysis during coronary surgery: on-pump versus off-pump techniques. Anesthesiology 2001; 95:1103-1109
(49) Longridge DJ, Follenfant MJ, Maxwell MP, et al. Enhanced myocardial salvage by maintenance of microvascular patency following initial thrombolysis with recombinant tissue plasminogen activator. Cardiovasc Ptes 1990; 24:697-706
(50) Bertuglia S, Colantuoni A. Protective effects of leukopenia and tissue plasminogen activator in microvascular ischemia-reperfusion injury. Am J Physiol Heart Circ Physiol 2000; 278:H755-H761
(51) Black SC, Gralinski MR, Friedrichs GS, et al. Cardioprotective effects of heparin or N-acetylheparin in an in vivo model of myocardial ischaemic and reperfusion injury. Cardiovasc Res 1995; 29:629-636
(52) Thourani VH, Brar SS, Kennedy TP, et al. Nonanticoagulant heparin inhibits NF-KB activation and attenuates myocardial reperfusion injury. Am J Physiol Heart Circ Physiol 2000; 278:H2084-H2093
(53) Lawson CA, Yan SD, Yah SF, et al. Monocytes and tissue factor promote thrombosis in a murine model of oxygen deprivation. J Clin Invest 1997; 99:1729-1738
(54) Tanaka K. Specific inhibition of thrombin activity during cardiopulmonary bypass reduces ischemia-reperfusion injury of the lung. Fukuoka Igaku Zasshi 2001; 92:7-20
(55) Saffitz JE, Stahl DJ, Sundt TM, et al. Disseminated intravascular coagulation after administration of aprotinin in combination with deep hypothermic circulatory arrest. Am J Cardiol 1993; 72:1080-1082
* From the St. Vincent's Hospital Intensive Care (Drs. Dixon and Santamaria) Melbourne; St. Vincent's Institute of Medical Research Melbourne, and Department of Medicine University of Melbourne (Dr. Campbell), Melbourne, Victoria, Australia. The study was supported by St. Vincent's Hospital Research Endowment Fund and a Medical Post-Graduate Research Award from the National Health and Medical Research Council of Australia.
Manuscript received August 5, 2004; revision accepted December 9, 2004.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Corresponaence to: Barry Dixon, MD, Intensive Care, St. Vincent's Hospital, 41 Victoria Parade Fitzroy Melbourne, Victoria 3065, Australia; e-mail: barry.dixon@svhm.org.au
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group