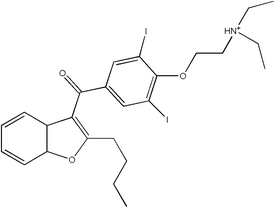
INTRODUCTION: Amiodarone pulmonary toxicity most commonly takes the form of interstitial pneumontitis (1). Here we report a case of amiodarone-induced lung injury presenting as a pulmonary mass.
CASE PRESENTATION: A 66 year old woman presented to hospital with dyspnea secondary to congestive heart failure and high grade atrioventricular block. She underwent insertion of a biventricular pacemaker without complication. A routine post-procedure chest radiograph revealed a right upper lobe mass. She was referred for further pulmonary assessment. She has a 50 pack year smoking history. Her past medical history is significant for severe left ventricular dysfunction, supraventricular tachycardia (SVT), recently diagnosed hypothyroidism, hyperlipidemia and remote pulmonary embolism. SVT had been treated with amiodarone 200mg daily for four years (total cumulative dose approximately 300g). Her dyspnea had resolved following pacemaker insertion and medical management of heart failure. She denied any other respiratory or constitutional symptoms. Physical examination was unremarkable. ALT was mildly elevated (67 U/L). A nonenhanced chest computed tomography (CT) scan showed an irregular right upper lobe mass measuring 3.0 x 2.3 cm (Figure 1). A smaller (1.8 x 1.2 cm) right lower lobe peripheral wedge shaped lesion was also noted. There was increased density of both lesions (80 Hounsfield units) as well as hyperdensity of the liver. Percutaneous fine needle aspirate of the right upper lobe mass was performed. Pathology revealed chronic interstitial inflammation, organizing pneumonia, intra-alveolar aggregates of foamy macrophages and type 2 pneumocyte hyperplasia. There was no evidence of malignancy. These results are consistent with pulmonary changes due to amiodarone therapy (1). Repeat imaging three months after discontinuation of amiodarone showed complete resolution of radiologic abnormalities (Figure 2).
[FIGURE OMITTED]
DISCUSSIONS: This case represents an unusual presentation of amiodarone pulmonary toxicity. There have been isolated case reports of similar presentations over the last 20 years, but none of these have correlated radiographic and CT imaging with light and electron microscopy (24). Previous reports have postulated that these solitary depositions are due to increased localized accumulation of the drug in an area of previous inflammation (5). Interestingly, all previous reported cases describe masses in the upper lobes, particularly right upper lobe. Our case highlights the fact that primary lung cancer needs to be excluded in a long standing smoker with a lung mass. Also, one needs to consider amiodarone toxicity as a potential, usually reversible, etiology. With an increasing population at risk for both lung cancer and cardiovascular disease, the need for this distinction will become increasingly important. It also demonstrates that amiodarone toxicity can occur alter many years of low dose therapy. Previous studies support that toxicity correlates more closely with total cumulative dose and duration than with serum drug levels (1). This case is in keeping with previous reports who had concomitant thyroid disease and/or liver toxicity. Abnormalities in other organ systems should prompt physicians to look for pulmonary amiodarone toxicity in asymptomatic patients. Diagnosis can be made by combination of clinical, radiologic and/or pathologic findings with improvement after discontinuation of the drug.
CONCLUSION: Amiodarone-induced toxicity should be included in the differential diagnosis of pulmonary mass lesions in patients receiving amiodarone.
REFERENCES:
(1) Camus P et al. Amiodarone pulmonary toxicity. Clin Chest Med 2004;25:65-75.
(2) Arnon R et al. Amiodarone pulmonary toxicity presenting as a solitary lung mass. Chest 1988;93:425-427.
(3) Piccione W Jr et al. Amiodarone-induced pulmonary mass. Ann Thorac Surg 1989;47:918-919.
(4) Rodriguez-Garcia JL et al. Pulmonary mass and multiple pulmonary nodules mimicking a lung neoplasm as amiodarone-induced pulmonary toxicity. Eur J Intern Med 2001;12:372-376.
(5) Kuhlman JE et al. Amiodarone Pulmonary Toxicity: CT findings in symptomatic patients. Radiol 1990;177:121-125.
DISCLOSURE: Julie Jarand, None.
Julie Jarand MD * Jessi Minion MD Andrew Lee MD Francis Green MD Richard Leigh MD University of Calgary, Calgary, AB, Canada
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group