Business Editors/Health/Medical Writers
SAN FRANCISCO--(BUSINESS WIRE)--May 20, 2003
Eli Lilly and Company (NYSE:LLY)
-- Naturalistic Study Provides Valuable Information About How
Antipsychotic Treatments May Affect Schizophrenia Patients'
Ability To Move Their Lives Forward
Six-month findings from the world's largest observational schizophrenia study show that although patients treated with atypical antipsychotics experienced marked improvement in their quality of life, various treatments differed in terms of effectiveness, sometimes significantly. People treated with olanzapine had greater symptom improvement and social functioning compared with patients on other leading schizophrenia medications, researchers reported today at the annual meeting of the American Psychiatric Association.
Unlike a traditional clinical trial, the Schizophrenia Outpatient Health Outcomes (SOHO) study will collect scientifically robust, long-term data in "real-world" settings. Eli Lilly and Company is sponsoring two three-year studies, one in Western Europe (SOHO EU) that includes 10 countries and approximately 10,000 patients. The second study is being conducted in Asia, Central and Eastern Europe, Latin America and the Middle East (SOHO IC) and includes 27 countries and 8,600 patients. With more than 18,600 patients enrolled from 37 countries, SOHO is unprecedented in size and scope.
Six Month Key Findings
-- In SOHO EU research, patients on olanzapine had significantly
greater improvement in positive (delusions and
hallucinations), negative (diminished emotion, lack of
interest), depressive, cognitive and overall symptoms and
social functioning compared with patients on risperidone,
quetiapine, oral typical and depot typical antipsychotics. No
significant differences were found between olanzapine and
clozapine.
-- Of the 10,204 patients included at the start of the SOHO EU
study, 9,028 (88.5%) were still in the trial six months later.
This is an exceptionally high retention rate for a study
evaluating treatments in people with schizophrenia, as this
population is prone to medication compliance problems.
-- Greater than 35 percent of patients in the SOHO EU study on
risperidone and typical antipsychotics were taking
anticholinergic agents (medication to control tremors or other
movement disorders) or experiencing movement disorders after
the first six months of treatment. This is compared with 20
percent or fewer patients treated with olanzapine or
clozapine.
-- Using a questionnaire specific to Germany, a subanalysis of
German outpatients with schizophrenia (n = 2,450) suggests
that after six months of treatment patients prescribed
atypical antipsychotics experienced strong improvements in
quality of life, including subscores reflecting self-control,
physical and mental functioning, emotional regulation and
social interaction.
-- Another analysis that specifically looked at SOHO IC patients
on either olanzapine or quetiapine (n = 7,655) found that
patients treated with olanzapine showed greater improvement in
clinical status and social functioning compared to those
treated with quetiapine.
-- In a SOHO IC analysis (n=501) of neuroleptic naive patients
with schizophrenia, 19 percent of patients treated with
risperidone and 30 percent of patients treated with
haloperidol developed impotence/sexual dysfunction compared to
three percent of olanzapine-treated patients.
-- Across treatment categories, results from measurements
collected by study investigators at six months are consistent
with results obtained from questionnaires completed directly
by the patients in the study.
"SOHO has yielded important information about the care we provide people with schizophrenia and the real-world outcomes of that care," said Dr. William M. Glazer, associate clinical professor of psychiatry, Massachusetts General Hospital, Harvard Medical School. "This kind of naturalistic study complements the data of more traditional clinical trials. Rigid exclusion criteria in conventional studies can limit our ability to reflect the patient population we see everyday."
Glazer continued, "Despite the vast differences in health care systems and cultures across the 10 European Union countries, there is marked consistency in the results. This validates the study's design and also reflects the clinical utility of agents such as olanzapine."
Study Design
Patients were enrolled in the study if, at the discretion of the treating psychiatrist, they started or changed antipsychotic medication in the outpatient setting. There are two study groups: patients who started the study with, or changed to, olanzapine and those who started the study with or changed to another antipsychotic such as amisulpride, quetiapine, risperidone, an oral typical, depot typical or a combination of these medications.
Mean change in positive, negative, depressive and overall symptoms from baseline to six months was measured using the Clinical Global Impressions-Schizophrenia scale (CGI-S).
The SOHO study will look at more than 30 areas over the course of three years to assess how treatment patterns affect patients' living conditions, clinical status, health-related quality of life, and ability to work and socialize. It will also assess treatment tolerability, compliance, victimization, violence and resource use.
About Schizophrenia
Schizophrenia is a severe and debilitating psychosis often characterized by acute episodes of delusions (false beliefs that cannot be corrected by reason), hallucinations (usually in the form of non-existent voices) and long-term impairments such as diminished emotion, lack of interest and depressive signs and symptoms. It is usually associated with a disruption in social and family relationships.
Schizophrenia is the most common severe mental illness. There are as many as 50 million people with schizophrenia worldwide, more than 33 million of them in developing countries. Symptoms of schizophrenia usually begin to appear in the teen-age years or early to mid-20s.
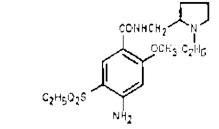
Olanzapine Background
Olanzapine is indicated in the United States for the treatment of schizophrenia, the short-term treatment of acute manic episodes associated with bipolar disorder and for the long-term therapy and maintenance of treatment response of schizophrenia. Olanzapine was the first atypical antipsychotic to prove its long-term effectiveness in patients with schizophrenia. Since olanzapine was introduced in 1996, it has been prescribed to 11 million people worldwide.
In the original schizophrenia registration trials, olanzapine was generally well tolerated. However, as with all medications, olanzapine was associated with some side effects. In the original six-week, acute-phase schizophrenia trials, the most common treatment-emergent adverse event associated with olanzapine was somnolence. Other common events were dizziness, weight gain, constipation, akathisia (inner and outer restlessness) and postural hypotension. Modest elevations of prolactin were also seen, although mean changes from baseline to endpoint were not statistically significantly different between olanzapine and placebo. A small number of patients experienced asymptomatic elevations of hepatic transaminase; none of these patients developed jaundice or drug-induced hepatitis.
In short-term (three- and four-week) acute bipolar mania trials, the most common treatment-emergent adverse event associated with olanzapine was somnolence. Other common events were dry mouth, dizziness, asthenia (muscle weakness), constipation, dyspepsia, increased appetite, and tremor.
About Eli Lilly and Company
Lilly, a leading innovation-driven corporation, is developing a growing portfolio of best-in-class pharmaceutical products by applying the latest research from its own worldwide laboratories and from collaborations with eminent scientific organizations. Headquartered in Indianapolis, Ind., Lilly provides answers -- through medicines and information -- for some of the world's most urgent medical needs. Additional information about Lilly is available at www.lilly.com.
COPYRIGHT 2003 Business Wire
COPYRIGHT 2003 Gale Group