Background & objectives: Tumour necrosis factor-alpha (TNF-α) has been suggested to play a key role in insulin resistance (IR) in obesity and may contribute to the development of type 2 diabetes mellitus. Recently, studies are focused on the effect of antihypertensive drugs on insulin sensitivity and cytokines. We undertook this study to evaluate the effect of amlodipine, a long-acting dihydropyridine calcium channel blocker treatment on TNF-α, homeostasis model assessment (HOMA) IR and leptin levels in obese hypertensive type 2 diabetic patients.
Methods: Amlodipine 5-10 mg for 12 wk was given to type 2 diabetic patients in the amlodipine group. Pre- and post-treatment values of laboratory parameters in the amlodipine group were compared with those of normotensive nondiabetic obese controls. At baseline blood pressures (BP) and metabolic parameters were measured in all patients and repeated after 12 wk in the amlodipine group.
Results: Basal waist-to-hip ratio, systolic and diastolic BPs, fasting glucose, TNF-α and HOMA-IR values of the amlodipine group were higher than the control group. No difference was detected in body mass index, fasting insulin, hemoglobin A^sub 1c^ and leptin values between groups. The systolic and diastolic BPs, fasting glucose, HOMA-IR and TNF-α values decreased significantly after the treatment. But, there was no correlation between percentage change in TNF-α and HOMA-IR.
Interpretation & conclusion: Besides reducing BP, amlodipine seemed to improve IR and decrease TNF-α levels. In this context, these properties may provide additional benefits of antihypertensive drug regimens chosen for this population, but larger group interventions are needed.
Key words Amlodipine * insulin resistance * leptin * tumor necrosis factor-alpha
Insulin resistance (IR) with consequent hyperinsulinaemia has a central role in the pathogenesis of many diseases including diabetes mellitus (DM), hypertension, obesity and dyslipidaemia and is generally accepted as an independent risk factor for atherosclerosis1. Though genetic and environmental factors are known to be causing IR, its etiology is still obscure1,2. A cytokine tumour necrosis factor-alpha (TNF-α) is thought to be participating in the IR in obese subjects by inhibiting tyrosine kinase activity at the insulin receptor. Phosphorylation of the insulin receptor by tyrosine kinase is critical for the binding of insulin to its receptor3. It also decreases expression of glucose transporters4. Adipocytes secrete another cytokine leptin as well as TNF-α. Weight reduction with dietary control decreases both TNF-α expression and serum leptin levels. This leads to improvement in insulin sensitivity and lipid metabolism5. There is evidence to show that TNF-α and leptin might influence each other in the development of IR6. Besides, TNF-α levels in obese subjects are supposed to be related to the regulation of plasma leptin concentrations7.
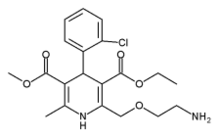
It is important to control hypertension in type 2 diabetic patients as it increases both morbidity and mortality, if uncontrolled8. The effects of antihypertensive drugs on insulin sensitivity in diabetic patients have been studied, and it was found that angiotensin-converting enzyme (ACE) inhibitors, alpha-blockers and long-acting calcium channel blockers (CCB) ameliorate9-11, whereas beta-blockers, short-acting CCBs, and thiazide diuretics impair insulin sensitivity12,13. Though the relationship between CCBs and IR has been evaluated in different studies, the effects of CCBs on IR and glucose metabolism are not yet fully understood. A study conducted by utilizing mice and a human peripheral blood mononuclear cell culture indicated that amlodipine decreased TNF-α both in vivo and in vilro conditions14. In human studies conducted in essential hypertensive nondiabetic patients with or without obesity, amlodipine was found to improve insulin sensitivity although the relation between this improvement and TNF-α was not investigated 11,15. In type 2 diabetic patients, the effect of amlodipine on TNF-α, leptin and IR has not been reported yet. Therefore, in the present study we aimed to evaluate the effect of amlodipine, a long-acting dihydropyridine CCB, on IR, TNF-α, leptin, glucose and lipid metabolisms in type 2 diabetic patients.
Material & Methods
A prospective study was conducted in obese hypertensive type 2 diabetic outpatients. Inclusion criteria were as follows: age between 18-70 yr, having mild (systolic blood pressure-SBP: 140-159 mm Hg and/or diastolic BP-DBP: 90-99 mmHg) or moderate (SBP: 160-179 mm Hg and/or DBP: 100-109 mmHg) hypertension according to World Health Organisation (WHO) criteria16, body mass index (BMI) above 25 kg/m^sup 2^, being on diabetic diet with or without gliclazide treatment. Patients having drugs other than gliclazide, other illness that may influence lipid and carbohydrate metabolism, illness or condition that may effect TNF-α level, pregnancy, diabetic nephropathy, renal artery stenosis, coronary artery disease, and hypersensitivity against amlodipine were excluded from the study. The study protocol was approved by the ethics committee of the institution and informed written consent was taken from all patients before participation.
Between January and November 2001, 24 consecutive patients (amlodipine group) satisfying the inclusion criteria were recruited in the study. During the study there were 4 withdrawals, 2 of them due to amlodipine's side effect and 2 on their own willingness. The rest 20 subjects completed the study. To compare the basal values of the amlodipine group, age, gender and BMI matched 20 obese nondiabetic normotensive subjects were selected as controls (control group) from our hospital staff to evaluate the possible additive effect of hypertension and DM on IR and TNF-α in the amlodipine group.
All subjects in the control and amlodipine groups underwent a complete physical examination, electrocardiographic, biochemical and haematologic investigations. Patients in the amlodipine group were receiving either diabetic diet or diabetic diet and gliclazide treatment besides a regular exercise programme at least over one year. Diabetic diet was prepared for each patient by the same dietitian according to American Diabetes Association (ADA) criteria17. After enrollment, no change was done in gliclazide dosage, diet and exercise modalities throughout the study. Eleven patients were using different antihypertensive agents including 1 thiazide diuretic, 2 angiotensin receptor blockers (ARB), 2 ACE inhibitors, 1 cardioselective beta blocker, and 5 nondihydropyridine CCBs. Before including in the study, the patients had a washout period of 4 wk for their previous antihypertensive medications. Then all the patients with or without antihypertensive medication before admission were given daily 5 mg of amlodipine orally (Monovas tablet, Mustafa Nevzat Drug Industry Company, Turkey) for 12 wk. If blood pressure control could not be achieved during visits, daily dose was increased up to 10 mg as was the case in five patients. Possible side effects of the drug were recorded during visits.
SBP and DBP, and heart rates were measured at the beginning of the study in the control group and at the beginning, 6th and 12th wk of the treatment in the amlodipine group. SBP and DBPs were measured after 10 min of resting from patient's right arm with sphygmomanometer twice with 2 min intervals in sitting position and the arithmetical mean was calculated. BMIs and waist to hip ratios (WHR) were also calculated.
Laboratory tests'. At the beginning of the study serum glucose and insulin levels were measured 3 times with 5 min intervals after 12 h of fasting in both of the groups and a second measurement was done in the amlodipine group after 12 wk of amlodipine treatment. The arithmetical means of the three values were obtained and used in the calculation of insulin sensitivity by using the homeostasis model assessment-insulin resistance (HOMA-IR) index [fasting glucose (mmol/l) x fasting insulin (µu/ml)/ 22.5]18. The following measurements were also done in both groups in the beginning after 12 h of fasting: serum glucose, total cholesterol (T-Chol), triglyceride (TG) (enzymatic assay, with Technicon Omnipak Glucose, T-Chol and TG reagents according to manufacturer's instructions, Technicon Dax System Methods Manual Technicon Instruments Corp. New York, USA) and high density lipoprotein cholesterol (HDL) (enzymatic assay, Randox Direct HDL-Cholesterol, Randox Laboratories Ltd., Belfast, Northern Ireland) with enzymatic methods by autoanalyzer (Technicon Dax System, Technicon Instruments Corp., New York, USA); lipoprotein (a) [Lp(a)], apolipoprotein A1 (Apo A1) and apolipoprotein B (Apo B) (N Latex Lp(a), N antisera to human apolipoprotein A-I and apolipoprotein B, Behring Diagnostics Inc. Westwood, USA) by Behring nephelometer;-haemoglobin A1c (HbA^sub 1c^) (high performance liquid chromotography, BIO RAD Diagnostics Group, California, USA) and insulin levels (radioimmunassay, Medical System DPC, Los Angeles, CA, USA). These measurements were repeated in the amlodipine group after 12 wk of treatment. Glucose and HbA levels of the patients were also measured 4 wk before recruitment in the study. Very low density lipoprotein (VLDL) and low density lipoprotein (LDL) cholesterol levels were calculated according to Freidewald formula19. TNF-α (Human TNF-alpha ELISA Version 2 BMS223/2, enzyme-linked immunosorbent assay, Bender MedSystems, Vienna-Austria) and leptin (Quantikine Human Leptin Immunoassay DLPOO, R&D Systems, United Kingdom) levels were measured in all subjects of the control group once and in patients of the amlodipine group before and after 12 wk of amlodipine treatment according to manufacturers' instruction. Standard curves and detection of quantitative values were obtained with Cricket graph programme.
Statistical analysis: The data were expressed as mean ± SEM. The sample size was small in both groups. By taking variability skewness (α3) and curtosis (α4) values into account the non-parametric and parametric test options were evaluated. The data in the sample did not show normal distribution except age variable. Statistical analysis was performed with non-parametric Wilcoxon signed rank test in intragroup comparisons in the amlodipine group. Since before and after treatment values of the amlodipine group were dependent and the values of the control group was independent, non-parametric Mann-Whitney U test was used in intergroup comparisons between control group and before treatment, between control group and after treatment and between before and after treatment values. Parametric unpaired t test was used for the comparison of ages of both groups. Comparisons of gender ratios in both groups were performed with Fischers' exact test. To evaluate the correlation between percent changes, Pearson correlation test was used. Value of P
Results
Two female patients in the amlodipine group developed oedema of the lower extremities as a side effect of amlodipine and dropped out. Two male patients did not continue the study because of social problems. In the amlodipine group the results of 20 patients were evaluated.
There was no significant difference between gender ratios and mean ages of the subjects in the amlodipine (F/M: 12/8, 53.8 ± 1.9 yr, range 36-69 yr) and control groups (F/M: 13/7, 49.0 ± 1.7 yr, range 37-66 yr). The duration of diabetes in the amlodipine group was 3.7 ± 0.5 yr and that of hypertension was 4.9 ±1.3 yr. Five patients in the amlodipine group needed only diabetic diet for glucose regulation and others needed daily 92 ± 9.5 mg of gliclazide treatment besides diabetic diet. The pre- and post-treatment BMl values of the amlodipine group did not differ from that of control group, while WHR was significantly lower in the control group compared to pre-treatment value of the amlodipine group (P
Mean glucose and HbA^sub 1c^ levels of the patients in the amlodipine group obtained 4 wk before recruitment were 7.9 ± 0.7 mmol/l and 7.1 ± 0.4 per cent and did not differ from the pre-treatment values. Pre-treatment mean HOMA-IR (P
Both basal HDL (P
When correlations between percentage changes in parameters like TNF-α, HOMA-IR, serum fasting glucose, BP and Apo Al that had statistically significant alteration after amlodipine treatment were investigated, the percentage changes in TNF-α levels correlated with changes in BMI values. There was a positive correlation between percentage changes in fasting glucose and insulin levels with percentage changes in HOMA-IR (Table III). The changes in SBP were also correlated with changes in DBP (r: 0.530, P
Discussion
In the present study, amlodipine was found to improve IR and decrease TNF-α levels as well as lower BP effectively in hypertensive obese type 2 diabetic patients. Studies have shown that TNF-α is associated with IR syndrome in certain conditions14,20. TNF-α levels in essential hypertensive subjects were found to be higher than or similar to normotensive controls21,22. TNF-α levels were also reported to be higher in obese type 2 diabetic patients with IR compared to those without IR and controls23. A two year follow up study conducted in elderly patients revealed that TNF-α levels continuously increased and led to deterioration in glycaemic control24. Hyperinsulinaemia and leptin secretion from adipocytes might be important in the development of hypertension and IR in obese patients25,26. TNF-α affects BP by causing IR and hyperinsulinaemia, as well.
It is known that antihypertensive agents that affect IR might also affect TNF-α. The effects of CCBs on IR are generally reported to be neutral or positive. In a rat study, amlodipine and nifedipine were found to increase insulin sensitivity, but not ACE inhibitors and nitrendipine27. Amlodipine also improved insulin sensitivity in non diabetic obese or non obese hypertensives11 CCBs are thought to be inhibiting TNF-α production with different mechanisms. Among them, amlodipine is known to be a free radical scavenger increasing vascular prostocycline production and inhibiting TNF-α production and/or its effect28. In a study conducted in mice, CCBs including amlodipine inhibited TNF-α production in 1-10 times higher doses than clinically effective doses14. The in vivo effects of these drugs may not be similar with in vitro effects but these suprapharmacological doses in mice might be similar to clinical doses in humans despite absence of clinical evidence. In clinical studies the effect of amlodipine in improving IR was studied but not on TNF-α11,15. After 12 wk of amlodipine treatment TNF-α, HOMA-IR, SBP and DBP of amlodipine group decreased while BMI and leptin levels were unchanged. Lack of correlation between TNF-α and other parameters may be due to small number of subjects, which is a limitation of our study. In two previous studies29,30 conducted in obese type 2 diabetic subjects no correlation could be detected between HOMA-IR and TNF-α levels. Lack of correlation was explained with the presence of hyperglycaemia, hyperinsulinaemia or other factors which have a stronger impact on peripheral insulin sensitivity in type 2 DM29,30.
Many factors like BMI, BP and glycaemic control might affect IR in an obese hypertensive diabetic patient population like our amlodipine group. BMI was unchanged during amlodipine treatment possibly explaining unchanged leptin levels, although leptin release was shown to be an energy and calcium dependent procedure in in vitro studies31. In our patients changes in BP did not correlate with changes in HOMA-IR, possibly excluding the direct effect of decrease in BP over IR.
Although different CCBs might inhibit insulin release in in vitro conditions, glucose-dependent insulin secretion was found to be unchanged in in vivo studies32. Clinical studies conducted in hypertensive nondiabetic subjects indicated neutral effect of CCBs used in clinical doses as far as the glycaemic control was concerned13,33. Glucose and HbA^sub 1c^ levels of the patients in the amlodipine group at 4 wk and just before the treatment did not differ. We observed a decrease in fasting glucose and a stability in HbA^sub 1c^ level after 12 wk of amlodipine treatment. The stability of HbA^sub 1c^c during treatment with CCBs is in agreement with these results13. Although decrease in fasting glucose levels might be as the result of gliclazide treatment, it is important to notice that HbA^sub 1c^ which is a better predictor of glucose metabolism, was unchanged. Though gliclazide administration per se was shown to have an inhibitory effect on TNF-α production14, this factor was neutralized in our study with unchanged gliclazide dosages throughout the study. In an in vitro study gliclazide was shown to enhance insulin signaling in skeletal muscle but not restore glucose uptake34.
In conclusion, the findings of our study showed that amlodipine caused an improvement in IR and decrease in TNF-α levels. We also observed positive effect of amlodipine on glucose and lipid metabolisms besides its well known antihypertensive effects. It is difficult to draw any firm conclusions about the association between TNF-α, leptin, hypertension and amlodipine treatment because of small sample size. Another study with larger numbers of subjects is needed to draw definitive conclusions to verify the relationship between cytokines and antihypertensive treatment modalities.
References
1. Reaven GM. Banting Lecture 1998. Role of insulin resistance in human disease. Diabetes 1988; 37 : 1595-607.
2. DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care 1991; 14 : 173-94.
3. Hotamisligil GS, Budavari A, Murray D, Spiegelman BM. Reduced tyrosine kinase activity of the insulin receptor in obesity-diabetes. Central role of tumor necrosis factor-α. J Clin Invest 1994; 94 : 1543-9.
4. Stephens JM, Lee J, Pilch PF. Tumor necrosis factor-a-induced insulin resistance in 3T3-Lladipocytes is accompanied by a loss of insulin receptor substrate-1 and GLUT4 expression without a loss of insulin receptor- mediated signal transduction. JBiol Chem 1997; 272 : 971-6.
5. Halle M, Berg A, Northoff H, Keul J. Importance of TNF-alpha and leptin in obesity and insulin resistance: a hypothesis on the impact of physical exercise. Exerc Immunol Rev 1998; 4 : 77-94.
6. Kirchgessner TG, Uysal KT, Wiesbrock SM, Marino MW, hotamisligil GS. Tumor necrosis factor-alpha contributes to obesity-related heperleptinemia by regulating leptin release from adipocytes. J Clin Invest 1997; 700 : 2777-82.
7 Corica F, Allegra A, Corsonello A, Buemi M, Calapai G, Ruello A, et al. Relationship between plasma leptin levels and the tumor necrosis factor-alpha system in obese subjects. Int J Obes Relat Metab Disord 1999; 23 : 355-60.
8 Bakris GL. Pathogenesis of hypertension in diabetes. Diabetes Rev 1995; 3 : 460-76.
9 Paolisso G, Gambardella A, Verza M, D'Amore A, Sgambato S, Varricchio M. ACE inhibitors improves insulin sensitivity in aged insulin-resistant hypertensive patients. J Hum Hypertens 1992; 6 : 175-9.
10. I luupponen R, Lehtonen A, Vahalalo M. Effect of doxazosin on insulin sensitivity in hypertensive non-insulin dependent diabetic patients. Eur J Clin Pharmacol 1992; 43 : 365-8.
11. Harano Y, Kageyama A, Hirose J, Asakura Y, Yokota T, Ikebuchi M, et al. Improvement of insulin sensitivity for glucose metabolism with the long-acting Ca-channel blocker amlodipine in essential hypertensive subjects. Metabolism 1995; 44 : 315-9.
12. Lithell HO, Pollare T, Berne C. Insulin sensitivity in newly detected hypertensive patients: influence of captopril and other antihypertensive agents on insulin sensitivity and related biological parameters. J Cardiovasc Pharmacol 1990; 15 (SupplS) : S46-52.
13. Hedner T, Samuelsson O, Lindholm L. Effects of antihypertensive therapy on glucose tolerance; focus on calcium antagonists. J Intern Med Suppl 1991; 735 : 101-11.
14. Fukuzawa M, Satoh J, Ohta S, Takahashi K, Miyaguchi S, Qiang X, et al. Modulation of tumor necrosis factor-α production with anti-hypertensive drugs. Immunopharmacology 2000; 48 : 65-74.
15. Ueshiba H, Tsuboi K, Miyachi Y. Effects of amlodipine on serum levels of adrenal androgens and insulin in hypertensive men with obesity. Harm Metab Res 2001; 33: 167-9.
16. World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension.Guidelines Subcommittee. J Hypertens 1999; 17 : 151-83.
17. Bloomgarden ZT. American Diabetes Association 60lh Scientific Sessions, 2000: nutrition, lipids, and alternative medicine. Diabetes Care 2000; 23 : 1847-51.
18. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and B-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28 : 412-9.
19. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972; 18 : 499-502.
20. Hotamisligil GS, Spiegelman BM. TNF-α, and the insulin resistance of obesity. In: LeRoith D, Taylor SI, Olefsky JM, editors. Diabetes mellitus: a fundamental and clinical text. Philadelphia: Lippincott-Raven; 1996 p. 554-60.
21. Sheu WUH, Lee WJ, Chang RL, Chen YT. Plasma tumor necrosis factor alpha levels and insulin sensitivity in hypertensive subjects. Clin Exp Hypertens 2000; 22 : 595-606.
22. Demirbas B, Giiler S, Cakir B, Culha C, Aral Y. Plasma tumor necrosis factor-alpha levels and insulin resistance in nondiabetic hypertensive subjects. Horm Res 2002; 58 : 283-6.
23. Mishima Y, Kuyama A, Tada A, Takahashi K, Ishioka T, Kibata M. Relationship between serum tumor necrosis factor-alpha and insulin resistance in obese men with type 2 diabetes mellitus. Diabetes Res Clin Pract 2001; 52 : 119-23.
24. Lechleitner M, Herold M, Dzien-Bischinger C, Hoppichler F, Dzien A.Tumour necrosis factor-alpha plasma levels in elderly patients with type 2 diabetes mellitus - observations over 2 years. Diabetes Med 2002; 19 : 949-53.
25. Levy JR, Gyarmati J, Lesko JM, Adler RA, Stevens W. Dual regulation of leptin secretion: intracellular energy and calcium dependence of regulated pathway. Am J Physiol Endocrinol Metab 2000; 278 : E892-901.
26. Shimomura I, Hammer RE, Ikemoto S, Brown MS, Goldstein JL. Leptin reverses insulin resistance and diabetes mellitus in mice with congenital lipodystrophy. Nature 1999; 401 : 73-6.
27. Goyal RK. Hyperinsulinemia and insulin resistance in hypertension: differential effects of antihypertensive agents. Clin Exp Hypertens 1999; 21 : 167-79.
28. Chou TC, Yang SP, Pei D. Amlodipine inhibits proinflammatory cytokines and. free radical production and inducible nitric oxide synthase expression in lipopolysaccharide/interferon-gamma-stimulated cultured vascular smooth muscle cells. Jpn J Pharmacol 2002; 89 : 157-63.
29. Miyazaki Y, Pipek R, Mandarine LJ, DeFronzo RA.Tumor necrosis factor alpha and insulin resistance in obese type 2 diabetic patients. Int J Obes Relat Metab Disord 2003; 27 : 88-94.
30. Katsuki A, Sumida Y, Murashima S, Murata K, Takarada Y, Ito K, et al. Serum levels of tumor necrosis factor-alpha are increased in obese patients with noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 1998; 83 : 859-62.
31. Zheng D, Jones JP, Usala SJ, Dohm GL. Differential expression of ob mRNA in rat adipose tissues in response to insulin. Biochem Biophys Res Commun 1996; 218 : 434-7.
32. Wollheim CB, Sharp GW. Regulation of insulin release by calcium. Physio! Rev 1981; 61 : 914-73.
33. Trost BN, Weidmann P. Effects of calcium antagonists on glucose homeostasis and serum lipids in non-diabetic and diabetic subjects: a review. J Hypertens 1987; 5 (Suppl): S81-104.
34. Kumar N, Dey CS.Gliclazide increases insulin receptor tyrosine phosphorylation but not p38 phosphorylation in insulin-resistant skeletal muscle cells. J.Exp Biol 2002; 205: 3739-46.
Canan Ersoy, Sazi Imamoglu, Ferah Budak*, Ercan Tuncel, Erdinç Ertürk & Barbares Oral**
Departments of Endocrinology & Metabolism, * Immunology Laboratory of Microbiology & ** Immunology Microbiology, Uludag University Medical School, Bursa, Turkey
Received November 28, 2003
Reprint requests: Dr Canan Ersoy, Uludag University Medical School, Department of Endocrinology
16059, Görükle, Bursa, Turkey
e-mail: ecanan@uludag.edu.tr
Copyright Indian Council of Medical Research Nov 2004
Provided by ProQuest Information and Learning Company. All rights Reserved