Background: This retrospective study compared the efficacy, tolerability, and cost of two dihydropyridine calcium channel blockers. Methods: Charts of patients who had been on continuous antihypertensive therapy with amlodipine or felodipine for at least 6 months were reviewed. Analyses include mean changes in blood pressure, percentage of patients achieving blood pressure (BP)
Introduction
Hypertension occurs in approximately 50 million Americans (1 in 5), and the total financial impact of this condition, with its associated morbidity and mortality, has been estimated at over $33 billion for 1999 alone. Direct costs, including drugs and medical care, account for $24.5 billion. Moreover, hypertension is the most common risk factor for cardiovascular disease, a leading cause of death and associated with a cost of $286.5 billion in 1999-more than eight times the cost of hypertension alone.1
Tight blood pressure (BP) control has been demonstrated to reduce morbidity and mortality substantially in a range of patient types.2-4 However, as the third National Health and Nutrition Examination Survey revealed,5 only one-quarter of individuals diagnosed with hypertension are undergoing treatment to achieve target levels of BP control. Even among those treated,
Direct costs associated with hypertension management include pharmacologic therapy, plus office visits, and laboratory monitoring.2,6 Drug costs comprise as much as 80% of the total cost of hypertension care.2 Therefore, managed care organizations and health care facilities must constantly evaluate the effectiveness of medical treatment in relation to the cost of providing it.7 Many health care institutions and the National Committee for Quality Assurance overseeing managed care organizations8 are adopting the health plan employer data and information set (HEDIS) BP guidelines as a benchmark to measure outcomes and monitor the quality of care in their hypertensive populations. Adequate BP control, defined by HEDIS and the Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of Hypertension (JNC VI), is systolic BP (SBP)
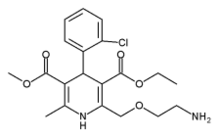
We initiated a study at the Naval Hospital (Jacksonville, Florida) specifically to address the most cost-effective way to make available on the formulary long-acting dihydropyridine calcium channel blockers (CCBs). Numerous well-controlled clinical trials have demonstrated the efficacy and tolerability of dihydropyridine CCBs for the treatment of hypertension,9-14 and these agents are considered among the most effective and versatile BP-lowering therapies currently available. Studies comparing different formulations of dihydropyridine CCBs demonstrate differences in pharmacokinetics, outcomes, and treatment costs.15
The Naval Hospital-Jacksonville conducted this study to determine whether either of two currently used dihydropyridine CCBs-amlodipine or felodipine-should be removed from their formulary based on efficacy, tolerability, and cost. Medical records were reviewed retrospectively and a cost analysis was conducted to compare BP control, defined by the JNC VI criteria, and cost per positive outcome (i.e., cost to achieve BP control) with amlodipine vs. felodipine.
Methods
Study Design
A systematic, retrospective chart review was conducted of patients who had been on continuous antihypertensive therapy with amlodipine or felodipine for at least 6 months as outpatients at the Naval Hospital-Jacksonville to compare the efficacy, tolerability, and cost of treatment with amlodipine vs. felodipine. Every fifth name from the entire list of patients on felodipine was selected for chart review. A random list of patients on amlodipine was generated and every fifth patient was reviewed, yielding a list of 800 patients. The medical records of 72 patients on amlodipine and 25 patients on felodipine seen at the facility were available for review. Of the 72 patients, 42 (30 patients on amlodipine and 12 on felodipine) met all the study criteria and were included in the outcome analysis.
Patient Population
An initial search of the hospital's computer database yielded a list of more than 4,000 patients who had received amlodipine and approximately 100 to 150 patients who had received felodipine during a 3-month period between January 1, 1999 and March 31, 1999. Patients had to have been on continuous antihypertensive therapy with amlodipine or felodipine for at least 6 months at the facility and have three pretherapy and three post-therapy BP measurements. Patients were excluded if they had been converted from another CCB. A data sheet was developed for this study prior to chart review. Only data for patients seen at the outpatient facility were included. Information extracted from patient records included demographics (age, sex, comorbid conditions), BP measurements at baseline and at the three most recent readings, average dose of amlodipine or felodipine and duration of the drug's use, concomitant cardiovascular (CV) medications at baseline and after 6 months of treatment, and side effects. Concomitant CV medications included diuretics, [beta] blockers, angiotensin-converting enzyme inhibitors, CCBs other than amlodipine or felodipine, a blockers, and other antihypertensive agents. These data were obtained from pharmacy profiles and confirmed by medical record review. All data were entered into a computer database for assessment.
BP Assessments
BP had to have been measured before and after administration of amlodipine or felodipine. For each patient, the mean of three BP measurements before drug therapy and the mean of BP measurements from the patient's last three outpatient visits on therapy at the Naval hospital were required to be available in the charts. The mean of the last three measurements was chosen to minimize unnecessary variation in BP readings and to provide a more accurate estimate of BP. This method is consistent with HEDIS methodology. Only one reading per visit was recorded. JNC VI guidelines were followed to determine whether adequate BP control (
Side Effects
Side effects were recorded if noted in the medical records. These data were then entered into the computer database but were not considered an end point in this study. The two specific side effects of headache and edema, which are among the most common side effects encountered with dihydropyridine CCBs, were specified in the data sheet, as were the categories "central nervous system" and "other."9,11
Cost Assessment
Antihypertensive medication costs derived from drug prices listed in the federal supply schedule at the time of analysis were used to calculate the total cost per day to treat each patient. The average dose of each of the two dihydropyridine CCBs, the cost per day of each, and the average cost of additional CV medication required for BP management as determined by the clinician were calculated to determine a total medication cost per day for patients in each group. A positive outcome was defined as good BP control as determined by JNC VI guidelines. The cost per positive outcome was calculated to account for the varying degrees of efficacy between the two agents. The cost per positive outcome was equal to the cost per day divided by efficacy rate x 100.
Statistical Analysis
The statistical test was determined by the type of data (categorical or continuous) and if the data were normally distributed. Categorical demographic characteristics were assessed using Fisher's exact test, except for the number of concomitant diagnoses, which were analyzed using the Row mean scores test. Continuous demographic data were assessed using analysis of variance (ANOVA) or the nonparametric Kruskal-Wallis test. Drug dose and duration were analyzed using the Kruskal-Wallis test. The number of concomitant medications was analyzed using Fisher's exact test; however, total concomitant medication use was analyzed categorically using the Row mean scores test and continuously using the nonparametric Kruskal-Wallis test. SBP and DBP data were assessed using ANOVA or the nonparametric Kruskal-Wallis test as appropriate. BP control was analyzed using Fischer's exact test. The use of ANOVA or Kruskal-Wallis was determined after testing the normality assumptions: if the normality assumption for either of the treatments was rejected (p > 0.10), then the Kruskal-Wallis nonparametric test was used; otherwise ANOVA was used. Side effects were analyzed using Fischer's exact test. The sample size of 12 in the felodipine group was managed statistically by using the non-parametric tests, Fischer's exact and Kruskal-Wallis, which minimize statistical error associated with smaller sample sizes (n
Results
Study Population
Among the 72 patients for whom data were collected (47 on amlodipine and 25 on felodipine), 42 patients met the criteria for outcome assessments (30 on amlodipine and 12 on felodipine). Demographic characteristics of the patients in each study group were similar, as shown in Table I. The mean age of patients on amlodipine was 55 years and among those on felodipine, 60 years. There were no statistical differences noted between study groups in gender, age, comorbid conditions, or number of concomitant diagnosis. Comorbidities identified in this patient population included angina, diabetes, and hypercholesterolemia. The average number of concomitant diagnoses was 1.9 with amlodipine and 1.8 with felodipine.
Dihydropyridine CCB Dosing
The average dose was 5.7 mg in the amlodipine group and 7.8 mg in the felodipine group. Patients had been taking amlodipine for an average of 26 months or felodipine for an average of 11 months (p = 0.00047).
BP Measures
A significantly greater percentage of amlodipine-treated patients achieved BP control compared with those on felodipine (p
Concomitant Medications
Concomitant antihypertensive medications prescribed to patients while on amlodipine or felodipine included diuretics, angiotensin-converting enzyme inhibitors, other CCBs, clonidine, [alpha] blockers, and [beta] blockers (Table III). Prior to treatment, 18 patients (72%) on amlodipine and 8 patients (67%) on felodipine were taking concomitant CV medications (Fig. 2). After treatment, the number of patients on concomitant antihypertensive drugs decreased to 15 patients (60%) on amlodipine and increased to 9 patients (75%) on felodipine. The mean number of concomitant antihypertensive medications after treatment decreased by 0.20 (19%) in the amlodipine group and increased by 0.167 (10%) in the felodipine group (p = 0.06). Notably, after treatment with felodipine, the percentage of patients prescribed an additional CV medication increased (from 67%-75%), and mean SBP decreased only slightly, whereas concomitant CV medication use in amlodipine-treated patients concomitant fell from 72% to 60%, whereas mean SBP decreased significantly.
Total Treatment Costs
Costs associated with BP control according to treatment are outlined in Table IV. The cost per positive outcome (cost to achieve BP control) per patient per day was lower by approximately one-half for patients on amlodipine ($0.87) compared with felodipine ($1.79). This occurred despite a higher average acquisition cost per patient per day for amlodipine ($0.683) compared with felodipine ($0.480), and higher total acquisition cost (dihydropyridine CCB plus concomitant CV medication). The average cost of concomitant antihypertensive medication was lower in the amlodipine group ($0.072/day) than in the felodipine group ($0.118/day) largely due to the greater number of concomitant medications used in the felodipine group. The number and type of concomitant medications used in each group are listed in Table III. Therefore, despite the higher acquisition cost, amlodipine is more cost-effective because of lower cost for additional CV medications and better BP control (positive outcome).
Adverse Events
Two of the 12 patients on felodipine (17%) experienced a headache (p = 0.076 vs. amlodipine) and 4 patients on felodipine (33%) had peripheral edema (p = 0.004 vs. amlodipine). None of the 30 patients on amlodipine were reported to have experienced side effects considered related to antihypertensive therapy. One potential explanation of the low incidence of side effects noted with amlodipine is that patients not tolerating the drug may have already discontinued the drug. Another factor in the overall low incidence of side effects noted for both drugs is that documentation of an adverse event in the medical record is often poor and inconsistent.
Discussion
The need to control escalating medical costs often drives formulary decisions at health care facilities. A recent economic evaluation of antihypertensive treatment suggests that decisions should be based on a broader focus than acquisition cost of medication alone, because the total cost of hypertension therapy is affected by the choice of first-line medication.6 This study demonstrates that formulary decisions about antihypertensive medications in settings such as that of the Naval Hospital-Jacksonville require analysis of the total medication costs per patient needed to achieve BP control, rather than simply cost per pill of a particular agent, if the total costs to the facility are to be assessed adequately.
Based on the cost per positive outcome in this study, amlodipine was superior to felodipine in controlling BP as defined by JNC VI and HEDIS guidelines in a cost-effective manner. Significantly more patients on amlodipine (87%) achieved BP control compared with
A lesser BP response, coupled with the need for additional CV medications to control BP, appeared to substantially increase the total cost of treatment for patients on felodipine, despite a lower acquisition cost per pill compared with amlodipine. Other drug conversion investigations support these findings.16,17 One study in a comparable outpatient setting demonstrated that patients converted from amlodipine to felodipine needed additional concomitant medications to control BP.16 In that study, instead of a projected cost savings of $18,000 annually across the institution, the switch resulted in an increased medication cost of nearly $4,900 for the 182 patients analyzed, which was extrapolated to project an expected total increase of more than $14,000 among all patients at the facility treated with CCBs. Other researchers have also found that the acquisition cost alone of antihypertensive therapy was a poor predictor of the total cost of treatment.17
Amlodipine and felodipine were well tolerated by patients included in our review, and this is consistent with CCBs in other clinical trials.18 For example, in the Treatment of Mild Hypertension Study, 83% of the 114 patients treated with amlodipine remained on this medication throughout the 4-year study, a percentage higher than that of the 483 patients randomized to an angiotensin-converting enzyme inhibitor, a-blocker, diuretic, or [beta]-blocker (p = 0.02 for differences).4
Second-generation dihydropyridine CCBs are well accepted as effective antihypertensive agents. However, agents in this category vary widely in terms of chemical structure and pharmacologic properties.9 Well-established differences in the pharmacokinetic profile of amlodipine and felodipine might account for some of the differences in BP control observed in this retrospective analysis. For example, amlodipine has a relatively higher bioavailability compared with felodipine10,15,19 and a longer duration of action.20 Amlodipine meets U.S. Food and Drug Administration antihypertensive drug guidelines of maintaining at least 50% of its peak BP-lowering effect at trough (the end of a 24-hour dosing period).21 A direct comparison of the peak-trough BP effects of amlodipine and felodipine revealed a more favorable ratio with amlodipine.22 Furthermore, plasma trough-to-peak concentration ratios were found to be significantly lower for felodipine (36%) than for amlodipine (67%) 24-hours postdose. Higher plasma concentrations 24-hours post-dose with amlodipine have been observed in another comparison with felodipine. In that study, amlodipine attained a smooth plasma concentration profile across a 24-hour period, whereas plasma concentrations of felodipine rapidly declined after 24 hours.23
Although it was expected that treating patients with felodipine would result in annual savings for the Naval Hospital-Jacksonville, in actuality the total cost to control BP with felodipine (dihydropyridine CCB plus concomitant CV medication) was more than double ($53.70/patient/month) the total cost to control BP with amlodipine ($26.10/patient/month). Extrapolated to the larger hypertension population of 4,000 treated with these agents at the facility, cost savings with amlodipine might be expected to exceed $1.3 million per year. As a result of this cost analysis study, the Pharmacy and Therapeutics Committee at the Naval Hospital-Jacksonville determined that amlodipine would remain on the formulary based on efficacy, tolerability, and cost per positive outcome, whereas felodipine would be removed from the formulary, because multiple concomitant drugs were generally required to control BP in a manner that was not cost-effective.
Conclusion
Several implications emerge from this study. First, containing costs without compromising patient care and outcomes remain an ongoing challenge for health care professionals treating patients with hypertension. Second, the acquisition cost of a drug can be misleading when evaluating the total cost of treatment. Third, conclusions drawn from this retrospective review reinforce the need for additional cost analysis studies that incorporate outcome data before making therapy choices.
In conclusion, amlodipine produced JNC VI-defined BP control in a substantially higher percentage of patients than did felodipine at a significantly lower total antihypertensive medication cost per positive outcome despite a higher initial acquisition cost. The lesser BP response and need for additional CV medications to control BP appeared to contribute to a higher overall cost per positive outcome of treatment for patients on felodipine. When evaluating the total cost of antihypertensive treatment, the acquisition cost of a drug alone can be misleading.
Acknowledgments
Synertact, Inc. (Encinitas, California) provided statistical support. AM Medica Communications Group (New York, New York) provided editorial assistance.
References
1. American Heart Association: 2000 Heart and Stroke Statistical Update. Dallas, TX, American Heart Association, 1999.
2. Odell TW, Gregory MC: Cost of hypertension treatment. J Gen Intern Med 1995; 10: 686-8.
3. Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure: The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med 1997; 157: 2413-46.
4. Neaton JD, Grimm Jr. RH, Prineas RJ, et al: Treatment of mild hypertension study. JAMA 1993; 270: 713-24.
5. Burt VL, Whelton P, Roccella EJ, et al: Prevalence of hypertension in the U.S. adult population: results from the Third National Health and Nutrition Examination Survey, 1988-1991. Hypertension 1995; 25: 305-13.
6. Ramsey SD, Nell N, Sullivan SD, Perfetto E: An economic evaluation of the JNC hypertension guidelines using data from a randomized controlled trial. J Am Board Fam Pract 1999; 12: 105-14.
7. Marwick C: Pharmacoeconomics: is a drug worth its cost? JAMA 1994; 272: 1395.
8. Alexander M, Tekawa I, Hunkeler E, et al: Evaluating hypertension control in a managed care setting. Arch Intern Med 1999; 159: 2673-7.
9. Palma-Gamiz JL: High blood pressure and calcium antagonism. Cardiology 1997; 88(Suppl 1): 39-46.
10. Van der Krogt JP, Brand R, Dawson EC, on behalf of the Amfortas Study Group: Amlodipine versus extended-release felodipine in general practice: a randomized, parallel-group study in patients with mild-to-moderate hypertension. CurrTher Res 1996; 57: 145-58.
11. Alexis G, Sessler NE, Conlin PR: Safety and efficacy of a mandatory formulary switch from nifedipine GITS to amlodipine. J Manag Care Pharm 1999; 5: 225-9.
12. Fagen TC, Haggert BE, Liss C: Efficacy and tolerability of extended-release felodipine and extended-release nifedipine in patients with mild-to-moderate essential hypertension. ClinTher 1994; 16: 634-46.
13. Kranz SR, Rase RS, Piepho RW: Retrospective analysis of formulary transition at large metropolitan HMO: nifedipine GITS to felodipine ER. J Manag Care Pharm 1996; 2: 642-6.
14. Burges RA, Dodd MG: Amlodipine. Cardiovasc Drug Rev 1990; 8: 25-44.
15. Videbaek LM, Jacobsen IA: Crossover comparison of the pharmacokinetics of amlodipine and felodipine ER in hypertensive patients. Int J Clin Pharmacol Ther 1997; 35: 514-8.
16. Oatis G, Stowers AD: A formulary conversion from amlodipine to felodipine ER: did the change fulfill expectations? Formulary 2000; 35: 435-42.
17. Hilleman DE, Mohiuddin SM, Lucas Jr. D, Stading JA, Stoysich AM, Ryschon K: Cost-minimization analysis of initial antihypertensive therapy in patients with mild-to-moderate essential diastolic hypertension. Clin Ther 1994; 16: 88-102.
18. Kloner RA, Vetrovec GW, Materson BJ, Levenstein M: Safety of long-acting dihy-dropyridine calcium channel blockers in hypertensive patients. Am J Cardiol 1998; 81: 163-9.
19. Abernethy DR, Gutkowska J, Winterboltom LM: Effects of amlodipine, a long-acting dihydropyridine calcium antagonist in aging hypertension: pharmacodynamics in relation to disposition. Clin Pharmacol Ther 1990; 48: 76-86.
20. Smilde JG: A comparison of amlodipine and felodipine extended release in the treatment of hypertension at steady state and after two missed doses. Curr Ther Res 1997; 58: 141-53.
21. Meredith PA. Elliott HL: FDA guidelines on trough: peak ratios in the evaluation of antihypertensive agents. J Cardiovasc Pharmacol 1994; 23(Suppl 5): S26-S30.
22. Bainbridge AD, Herlihy O, Meredith PA, Elliott HL: A comparative assessment of amlodipine and felodipine ER: pharmacokinetic and pharmacodynamic indices. Eur J Clin Pharmacol 1993; 45: 425-30.
23. Ostergren J, Isaksson H, Brodin U, Schwan A, Ohman KP: Effect of amlodipine versus felodipine extended release on 24-hour ambulatory blood pressure in hypertension. Am J Hypertens 1998; 11: 690-6.
Guarantor: LCDR Steven J. Blivin, MC USNR
Contributors: LCDR Steven J. Blivin, MC USNR*; Julie Pippins, PharmD[dagger]; Laura G. Annis, PharmD[double dagger]; Farris Lyons, BS[sec]
*Department of Primary Care, Naval Medical Clinic, Quantico, VA.
[dagger]Clinical Education, Pfizer Inc. New York, NY.
[double dagger]The University of Florida, Gainesville, FL.
[sec]The Pharmacy Department, Naval Hospital-Jacksonville, Jacksonville, FL.
Reprints: Dr. Steven J. Blivin, 5 Jamestown Court, Stafford, VA 22554; e-mail: blivin@dellnet.com.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Naval Medical Department or the Naval Service at large.
This manuscript was received for review in March 2002. The revised manuscript was accepted for publication in September 2002.
Reprint & Copyright (C) by Association of Military Surgeons of U.S., 2003.
Copyright Association of Military Surgeons of the United States Jul 2003
Provided by ProQuest Information and Learning Company. All rights Reserved