After a 4-year hiatus, this column returns as a regular fixture of Perspectives. As before, the emphasis will be on biological aspects of understanding and/or treating mental disorders. It is an interesting time to reintroduce this column, because now we can look back on the "decade of the brain" in its entirety and begin assessing its impact on psychiatric care.
While the congressional pronouncement heartened many of us concerned with psychiatric nursing's pre1990s reluctance to embrace biological constructs, it will be up to those with a greater breadth of vision to distill the decade's overall impact. It seems fair to say, even this early in the decade's review, that psychiatric nursing took the clarion call seriously and made substantial inroads into addressing the specialty's brain-related knowledge deficits. For example, in 1990 some psychiatric nursing textbooks still were alienating families with the suggestion that bad mothering (e.g., the schizophrenogenic mother) caused schizophrenia. You will not see such concepts in textbooks today. Further, all textbooks and journals now pay closer attention to psychotropic drugs and psychobiology than before the decade of the brain. Whether the overall field of psychiatric care evolved as hoped will be debated, but it is clear that important changes occurred in psychiatric nursing during those 10 years. This relaunching of Biological Perspectives aims at continuing a contribution to this momentum. In that vein, we address an area of psychiatric care undergoing significant change during the decade of the brain-antidepressant therapy.
During the 1990s and just before, a number of new antidepressant drugs were introduced: sertraline (Zoloft), paroxetine (Paxil), fluvoxamine (Luvox), bupropion (Wellbutrin), venlafaxine (Effexor), nefazodone (Serzone), mirtazapine (Remeron), and citalopram (Celexa). As new antidepressants, they empowered clinicians because they were, in Preskorn's (1994) words, "rationally developed." This rational development, or molecular targeting, starkly contrasted the serendipitous "discovery" of monoamine oxidase inhibitors (MAOIs) in 1952 (a better antituberculosis drug was sought) and tricyclic antidepressants (TCAs) in 1956 (a better antipsychotic was the goal). Prior to the selective serotonin reuptake inhibitors (SSRIs) and other "new" drugs mentioned above, clinicians had limited choices-for instance, when a TCA failed, the clinician was forced to stay "within class" or switch to the multiproblemed MAOIs. Since the numerous antidepressants available today provide improvement over the limited options of just a few years ago, it seems prudent to review just what makes them different from each other.
As it turns out, the array of antidepressant medications available today can be distinguished by at least seven distinct mechanisms of action; see BezchlibnykButler & Jeffries (199 and Stahl (1998).
1. Blocking enzymatic breakdown. The MAOIs were the first antidepressants "discovered," and the only antidepressants inhibiting neurotransmitter breakdown as a primary mechanism of action. Monoamine oxidase can be found in the liver, intestines, and terminals) of monoamine-- producing neurons. This enzyme can be further differentiated into type A (metabolizes nor-epinephrine and serotonin) and type B (metabolizes dopamine). MAOIs inactivate monoamine oxidase, resulting in increased levels of monoamines (dopamine, norepinephrine, serotonin). The older, nonselective drugs (e.g., phenelzine, tranylcypromine) inhibit both types A and B, while newer agents such as moclobemide (inhibits type A) and selegiline (inhibits type B) are more selective. MAOIs are known to cause serious interactions with tyramine-containing foods and with a number of drugs, particularly indirect-acting sympathomimetics and serotonin-enhancing agents. MAOIs have a narrow therapeutic index.
2. Nonselective inhibition of norepinephrine and serotonin uptake. The TCAs block uptake of both norepinephrine and serotonin. Some TCAs are more potent norepinephrine-uptake inhibitors (e.g. [in descending order], desipramine, protriptyline, amoxapine, nortriptyline) and others more potent serotonin-uptake inhibitors (e.g. [in descending order], clomipramine, amitriptyline, impramine), but all share the ability to block uptake of both neurotransmitters to some degree. Due to their nonselectivity, TCAs cause many side effects. TCAs have a narrow therapeutic index and can be lethal at doses only 10 times the therapeutic daily dose.
3. Selective serotonin uptake inhibition. SSRIs selectively block uptake of serotonin. These drugs, beginning with fluoxetine (Prozac) and continuing through citalopram (the singular psychotropic drug approved in 1998), significantly affected treatment of depression and are now first-line agents. SSRIs offer a good side effect profile but cause significant sexual dysfunction (+/-50%) and considerable gastrointestinal (GI) disturbances. It is thought serotonin 5HT^sub 2^ receptors modulate sexual activity and, when stimulated, result in anxiety and insomnia. Therefore 5HT^sub 2^ agonists (including SSRIs) contribute to sexual dysfunction, anxiety, and insomnia. Additionally, 5HT3 receptors are located in the gut and, when stimulated, cause GI symptoms. SSRIs are responsible for a number of GI complaints. SSRIs also interact with many other drugs, causing significant reactions. A major source of these drug-drug interactions is the inhibiting effect SSRIs exert on the cytochrome P-450 (P450) enzyme system. For example, fluoxetine inhibits the P450 isoenzymes 2C19, 2D6, and 3A3/4. Substrates of these enzymes will have slowed metabolism in the presence of fluoxetine. SSRIs have a wide therapeutic index.
4. Selective dopamine uptake inhibition. Bupropion is unique in two ways. It is the only antidepressant with dopamine-uptake inhibition as a major mechanism of action and it does not affect serotonin systems. Bupropion also inhibits norepinephrine uptake. This drug has a good side effect profile but significantly lowers the seizure threshold at higher dosages (>450 mg/day). Side effects (e.g., overstimulation, agitation, insomnia), as might be expected, are often related to increased catecholamine levels. Hence, bupropion is classified as an activating antidepressant. Bupropion's dopamineenhancing property accounts for its use in smoking-cessation programs (under the trade name Zyban). It is thought dopamine counters the craving associated with nicotine withdrawal. Further, in a general sense, it can be said dopamine tends to enhance sexual functioning and serotonin tends to inhibit sexual functioning. Since bupropion increases dopamine intrasynaptically, it countern SSRI-mediated sexual inhibition and is prescribed in low doses in conjunction with SSRIs for that very purpose. Buproprion has a narrow therapeutic index, though with considerably less lethal effects than those associated with MAOIs and TCAs.
5. Variable inhibition of serotonin, norepinephrine, and dopamine uptake. Venlafaxine inhibits the uptake of serotonin at lower doses, norepinephrine at medium doses, and dopamine at higher doses. At higher doses (>300 mg/day), elevations in blood pressure occur in 10% to 15% of patients. Venlafaxine provides a good side-effect profile overall but shares some problems assodated with SSRI-use related to sexual and GI function. It is metabolized by P450 2D6 and 3A3/4 enzymes and can be affected by drugs inhibiting those isoenzymes. Venlafaxine has a wide therapeutic index.
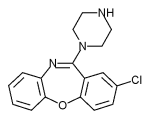
6. Serotonin uptake inhibition with 5HT^sub 2^ antagonism. Nefazodone is similar to SSRIs in that it selectively inhibits the uptake of serotonin into presynaptic terminals but has the added advantage of antagonizing 5HT^sub 2^ receptors--the receptors thought to mediate sexual-dysfunction, anxiety, and insomnia effects associated with SSRIs. This mechanism of action provides the benefits of serotonergic enhancement without inducing these troubling side effects. Further, 5HT^sub 2^ antagonism probably provides an antimigraine effect and, due to the efficacy of atypical antipsychotics (by definition 5HT^sub 2^ antagonists), may play a significant role in treatment of mixed psychotic/depressive symptoms. Nefazodone also antagonizes alpha-1 receptors, accounting for some cardiovascular side effects. Serious drug interactions occur with nefazodone due to inhibition of P450 3A4 enzymes. Nefazadone has a relatively wide therapeutic index.
7. Alpha^sub 2^ antagonism with 5HT^sub 2^and 5HT^sub 3^ antagonism. Mirtazapine increases availability of both serotonin and norepinephrine by its antagonism of alpha^sub 2^ autoreceptors. This antagonism triggers the feedback system to increase norepinephrine and serotonin activ ity. Mirtazapine's uniqueness is attributable to its antagonism of both 5HT^sub 2^ (i.e., reducing sexual dysfunction, anxiety, insomnia) and 5HT^sub 3^ (i.e., reducing GI distress). Mirtazapine does cause weight gain and sedation related to histamine receptor blockade. Mirtazapine is a substrate of P450 1A2, 2D6, and 3A3/4 enzymes. Drugs inhibiting these enzymes increase serum levels of mirtazapine. Mirtazapine has a wide therapeutic index.
Antidepressant therapy changed significantly during the decade of the brain. As we look forward to the years just ahead and to our collective efforts to stay abreast of antidepressants and other biological considerations, this column seeks to join in that effort by offering concise and informative articles for your review.
References
Bezchlibnyk-Butler, K.Z., & Jeffries, J.J. (1997). Clinical handbook of psychotropic drugs. Seattle: Hogrefe & Huber.
Preskorn, S.H. (1994). Antidepressant drug selection: Criteria and options. Journal of Clinical Psychiatry, 55(Suppl.A), 6-22.
Stahl, S.M. (1998). Basic psychopharmacology of antidepressants, Part I: Antidepressants have seven distinct mechanisms of action. Journal of Clinical Psychiatry, 59(Suppl.4), 5-14.
Annotated Bibliography
Bezchlibnyk-Butler, K.Z., & Jeffries, J.J. (1997). Clinical handbook of psychotropic drugs. Seattle: Hogrefe & Huber. This clinical manual has become a much-referenced classic for clinicians. The authors' antidepressant section groups these agents by mechanism of action into 7 to 11 different categories, depending on the categorizing scheme.
Keltner, N.L., & Folks, D.G. (199. Psychotropic drugs. St. Louis: MosbyYearbook She read: "This book provides a complete reference for psychotropic drugs and issues and developmental considerations related to drug therapy."
Lieberman, J.A., & Tasman, A. (2000). Psychiatric drugs. Philadelphia: Saunders. This is an excellent book that is comprehensive in scope yet fits easily into a pocket for ready reference in the clinical setting.
Preskorn, S.H., (1994). Antidepressant drug selection: Criteria and options. journal of Clinical Psychiatry, 55(Suppl.A), -22. "Paradigm shift" is an overworked phrase, but Preskorn takes most of us out of our comfort zone and enables us to "think bigger"; a very informative article.
Stahl, S.M. (1998). Basic psychopharmacology of antidepressants, Part 1: Antidepressants have seven distinct mechanisms of action. Journal of Clinical Psychiatry, 59(Supp1.4), 5-14. This article addresses the mechanisms of action for antidepressants and helps differentiate efficacy and side effect profile considerations. Excellent for those working with the depressed and critical to those prescribing antidepressants. A true classic.
Key words: Pharmacodynamics, pharmacokinetics, therapeutic usage
Norman L. Keltner, EdD, RN Associate Professor, University of Alabama, Birmingham, AL
Author contact: Keltnern@son.uab.edu, with a copy to the Editor: mary77@concentric.net
Copyright Nursecom, Inc. Apr-Jun 2000
Provided by ProQuest Information and Learning Company. All rights Reserved