Abstract
Objective To examine the association between selective serotonin reuptake inhibitors and risk of upper gastrointestinal bleeding.
Design Population based case-control study.
Setting General practices included in the UK general practice research database.
Subjects 1651 incident cases of upper gastrointestinal bleeding and 248 cases of ulcer perforation among patients aged 40 to 79 years between April 1993 and September 1997, and 10 000 controls matched for age, sex, and year that the case was identified.
Interventions Review of computer profiles for all potential cases, and an internal validation study to confirm the accuracy of the diagnosis on the basis of the computerised information.
Main outcome measures Current use of selective serotonin reuptake inhibitors or other antidepressants within 30 days before the index date.
Results Current exposure to selective serotonin reuptake inhibitors was identified in 3.1% (52 of 1651) of patients with upper gastrointestinal bleeding but only 1.0% (95 of 10 000) of controls, giving an adjusted rate ratio of 3.0 (95% confidence interval 2.1 to 4.4). This effect measure was not modified by sex, age, dose, or treatment duration. A crude incidence of 1 case per 8000 prescriptions was estimated. A small association was found with non-selective serotonin reuptake inhibitors (relative risk 1.4, 1.1 to 1.9) but not with antidepressants lacking this inhibitory effect. None of the groups of antidepressants was associated with ulcer perforation. The concurrent use of selective serotonin reuptake inhibitors with non-steroidal anti-inflammatory drugs increased the risk of upper gastrointestinal bleeding beyond the sum of their independent effects (15.6, 6.6 to 36.6). A smaller interaction was also found between selective serotonin reuptake inhibitors and low dose aspirin (7.2, 3.1 to 17.1).
Conclusions Selective serotonin reuptake inhibitors increase the risk of upper gastrointestinal bleeding. The absolute effect is, however, moderate and about equivalent to low dose ibuprofen. The concurrent use of non-steroidal anti-inflammatory drugs or aspirin with selective serotonin reuptake inhibitors greatly increases the risk of upper gastrointestinal bleeding.
Introduction
In the past few years several case reports have shown an association between selective serotonin reuptake inhibitors such as fluoxetine and bleeding disorders.[1-7] Most of the patients had mild bleeding disorders, for example, ecchymoses, purpura, epistaxis, or prolonged bleeding time but several had more serious conditions such as gastrointestinal haemorrhage, genitourinary bleeding, and intracranial haemorrhage.[3 6]
The release of serotonin from platelets has an important role in regulating the haemostatic response to vascular injury.[8 9] Serotonin is not synthesised in platelets but is taken up from the circulation by serotonin transporters on the platelets, which are similar to those in the human brain.[10] At therapeutic doses fluoxetine and other selective serotonin reuptake inhibitors have consistently been shown to block this reuptake of serotonin by platelets leading to a depletion of serotonin after several weeks of treatment.[11 12] It is possible that these drugs impair haemostatic function, at least under certain conditions, and thereby increase the risk of bleeding. We tested this hypothesis with data from an ongoing case-control study, which was set up to estimate the risk of ulcer complications from non-steroidal anti-inflammatory drugs.[13]
Subjects and methods
We studied data from the general practice research database. This database has been described elsewhere.[14] It contains details of patients' demographics, medical diagnoses, referrals to consultants and hospitals, and prescriptions. The accuracy and completeness of these data have been validated in previous studies.[15 16]
Case definition and ascertainment
The source population was all patients aged 40 to 79 years between April 1993 and September 1997, with at least 2 years' enrolment with their general practitioner. Patients with cancer, oesophageal varices, Mallory-Weiss disease, alcoholism, liver disease, or coagulopathies were excluded. We identified incident cases of upper gastrointestinal bleeding or ulcer perforation, and we reviewed the computerised profiles of such patients. We used the same case ascertainment as in a previous study).[13] We excluded patients in whom the oesophagus was the source of bleeding. To confirm the classification of patients established from a review of their computerised profiles, we requested from the general practitioners a copy of the original records of 100 randomly sampled patients. We received records for 96 patients of which 95 were confirmed as cases. We therefore decided to study all patients classified as cases on the basis of the review of computerised information.
Controls
We randomly selected 10 000 controls matched for age, sex, and time from the source population. We applied the same exclusion criteria.
Exposure definition
We defined patients as "current users" if a prescription for antidepressants lasted until index date or ended within 30 days of the index date, "past users" if the prescription ended before the 30 days defined for "current users," and "non-users" if there was no prescription before the index date. Current users were subdivided in to "current single users" and "current multiple users" The latter category included patients who had prescriptions for several antidepressants, with their respective supply ending within 30 days of the index date.
We studied the effect of dose (most frequently used or less versus higher doses) and treatment duration (90 days or less versus longer periods) among current single users. Duration of use was the treatment period covering consecutive prescriptions. Prescriptions were considered consecutive when less than 2 months elapsed between them.
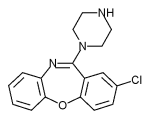
Antidepressants were classified in to three groups according to their inhibitory action on the serotonin reuptake mechanism: (a) selective serotonin reuptake inhibitors; (b) non-selective serotonin reuptake inhibitors; and (c) a miscellaneous group of "others." The first group comprised fluoxetine, fluvoxamine, paroxetine, sertraline, citalopram, clomipramine, and trazodone.[17 18] We decided to include clomipramine in this group because it is a potent and rather selective blocker of serotonin transport.[18] The second group comprised antidepressants that are thought to show a balanced inhibitory action on both serotonin and norepinephrine reuptake mechanisms. This group included amitriptyline, imipramine, lofepramine, doxepin, and dothiepin.[17-19] The third group comprised antidepressants that have either a selective inhibitory action on norepinephrine reuptake (nortriptyline, desipramine, trimipramine, maprotiline, and amoxapine)[17 18] or no action on any reuptake mechanism (mianserin)[17 18]
Potential confounders
Covariates studied as potential confounders were antecedents of upper gastrointestinal disorders, smoking status, and current use of non-steroidal anti-inflammatory drugs, anticoagulants, corticosteroids, or aspirin. Only prescription drugs are systematically recorded in the general practice research database. Most of the daily low dose aspirin used for cardioprotection in our study population was prescribed (unpublished results). To define the use of other drugs we used the same time windows as for antidepressants.
Analysis
We used unconditional logistic regression to determine the adjusted estimates of relative risk and 95% confidence intervals for current use of antidepressants compared with non-use of antidepressants. To study if these variables were modifiers of the effect measure associated with antidepressants we stratified the analysis by age and sex. Interaction was studied with standard epidemiological methods.[20] Relative excess risk due to interaction was used as a measure of interaction and was calculated as: Relative risk (A and B) - relative risk (A without B) - relative risk (B without A) + 1 where A and B are the factors whose interaction is being studied. Incidence rates of upper gastrointestinal bleeding associated with antidepressants were estimated with either users or prescriptions as denominator.
Results
Overall, 1651 patients had upper gastrointestinal bleeding and 248 had ulcer perforation. Fifty two (3.1%) patients with upper gastrointestinal bleeding were current users of selective serotonin reuptake inhibitors; among controls the proportion of current users was 1.0% (95 of 10 000) resulting in an adjusted rate ratio of 3.0 (2.1 to 4.4) (table 1). The effect measures were hardly modified by sex (relative risk 3.2 for men and 3.0 for women) or age group (2.9 for patients aged less than 70 years and 3.4 for patients aged 70 years or older).The rate ratio associated with non-selective serotonin reuptake inhibitors was 1.4 (1.1 to 1.9). No association was found with antidepressants that have no action on the serotonin reuptake mechanism (table 1). None of the three groups of antidepressants was associated with ulcer perforation (selective serotonin reuptake inhibitors: relative risk 1.3, 0.4 to 3.7; non-selective serotonin reuptake inhibitors: 0.4, 0.2 to 1.1; others: 1.3, 0.2 to 10.1).
Table 1 Risk of upper gastrointestinal bleeding associated with antidepressants
(*) Adjusted for sex, age, year, antecedents of upper gastrointestinal disorders, smoking status, and use of non-steroidal anti-inflammatory drugs, aspirin, anticoagulants, or steroids.
(dagger]) Fluoxetine, fluvoxamine, paroxetine, sertraline, citalopram, trazodone, clomipramine.
([double dagger]) Amitriptyline, dothiepin, imipramine, Iofepramine, doxepin.
([sections]) Nortriptyline, protriptyline, desipramine, trimipramine, maprotiline, amoxapine, mianserin. The 52 cases of upper gastrointestinal bleeding that occurred during current use of selective serotonin reuptake inhibitors arose from a cohort of 69 593 patients who received a total of 435 021 prescriptions for any of these drugs. The crude incidence rate of upper gastrointestinal bleeding for this population was estimated as 1 case per 8000 prescriptions or 1 case per 1300 users.
The risk of upper gastrointestinal bleeding was increased with all selective serotonin reuptake inhibitors although with clomipramine this was only marginal (table 2). After exclusion of trazodone--the drug with the greatest relative risk--the relative risk with selective serotonin reuptake inhibitors was 2.9 (2.0 to 4.2). The exclusion of clomipramine slightly increased the relative risk to 3.3 (2.2 to 4.9). Among non-selective serotonin reuptake inhibitors amitriptyline significantly increased the risk of upper gastrointestinal bleeding. A trend was noted with imipramine and lofepramine but dothiepin had no effect.
Table 2 Risk of upper gastrointestinal bleeding associated with current single use of antidepressants compared with non-use
(*) Adjusted for sex, age, year, antecedents of upper gastrointestinal disorders, smoking status, and use of non-steroidal anti-inflammatory drugs, aspirin, anticoagulants, or steroids.
Dose (equivalents of 20 mg fluoxetine for selective serotonin reuptake inhibitors or 75 mg amitriptyline for non-selective serotonin reuptake inhibitors or less versus higher doses) and duration of use (less than 91 days versus 91 days or longer) of either antidepressant group had little influence on the risk of upper gastrointestinal bleeding (data not shown). Most patients were prescribed medium or low doses of antidepressants, especially those receiving non-selective serotonin reuptake inhibitors where only 12% (30 of 242) of users among controls received equivalent amitriptyline doses greater than 75 mg.
The concurrent use of selective serotonin reuptake inhibitors with non-steroidal anti-inflammatory drugs greatly increased the risk of upper gastrointestinal bleeding (15.6, 6.6 to 36.6) (table 3) showing a more than multiplicative interaction (relative excess risk due to interaction 10.3). The relative risk of concurrent use of non-steroidal anti-inflammatory drugs with nonselective serotonin reuptake inhibitors compared with non-use was 4.6 (2.8 to 7.9), which roughly represents the sum of their respective effects (relative excess risk 0.2). An interaction was also observed between selective serotonin reuptake inhibitors and aspirin (7.2, 3.1 to 17.1; relative excess risk 3.5).
Table 3 Interaction between current use of selective serotonin reuptake inhibitors and current use of non-steroidal antiinflammatory drugs compared with non-use of either drug
(*) Adjusted for sex, age, year, antecedents of upper gastrointestinal disorders, smoking status, and use of aspirin, anticoagulants, or steroids. Discussion
Selective serotonin reuptake inhibitors increase the risk of upper gastrointestinal bleeding by threefold but they do not affect the risk of ulcer perforation. The absolute risk of upper gastrointestinal bleeding is estimated as 1 case per 8000 prescriptions, a risk similar to that of low dose ibuprofen.[13 21] The risk with all selective serotonin reuptake inhibitors is similar suggesting a class effect linked to their mechanism of action. Compatible with this hypothesis is the suggestion that some non-selective serotonin reuptake inhibitors may also increase the risk of upper gastrointestinal bleeding although to a lesser extent than selective serotonin reuptake inhibitors. This effect is not influenced by sex, age, dose, or duration of use but is greatly potentiated by the concurrent use of non-steroidal anti-inflammatory drugs and to a lesser extent low dose aspirin.
Causal relation
This is the first epidemiological study to support the hypothesis of an increased risk of gastrointestinal bleeding with selective serotonin reuptake inhibitors. Until now the only evidence was from anecdotal case reports. Although caution should be exercised in interpreting our results until confirmation by other studies a causal relation could be supported by the strength of the association found, the specificity shown by selective serotonin reuptake inhibitors for bleeding lesions compared with ulcer perforation, and the existence of a plausible biological mechanism. The release of serotonin from platelets seems to be an important step in platelet aggregation especially in the presence of collagen,[8] thrombin,[9] and ADP.[9] Therefore a depletion of serotonin from platelets would be expected to impair the haemostatic response to vascular injury.[22] The low frequency of this effect, however, indicates that only in certain circumstances would impaired aggregation be clinically patent, probably when alternative mechanisms are unable to compensate for the effect.
Antidepressants associated with upper gastrointestinal bleeding
With the exception of fluvoxamine all selective serotonin reuptake inhibitors were associated with upper gastrointestinal bleeding. Trazodone presented the greatest risk although its confidence interval overlapped with that of the other inhibitors. This finding is unexpected because trazodone is the inhibitor with the weakest effect on the serotonin reuptake mechanism. Interestingly, this drug is a potent blocker of [5-HT.sub.2] receptors,[23] the stimulation of which is thought to mediate the platelet aggregation induced by serotonin release.[8 9]
A trend to increase the risk of upper gastrointestinal bleeding was shown with all non-selective serotonin reuptake inhibitors, with the exception of dothiepin. This finding is compatible with the mechanistic hypothesis of an inhibitory action on serotonin uptake by platelets. The lack of effect of dothiepin contradicts this interpretation and merits comment. Dothiepin is chemically related to amitriptyline and is thought to mediate its antidepressant effect through inhibition of neuronal reuptake of norepinephrine and serotonin.[19] However, in some experimental models dothiepin has shown considerable selectivity for norepinephrine uptake with low or no action on serotonin uptake.[24]
Interaction with non-steroidal anti-inflammatory drugs
One of the most singular findings of our study was the interaction between selective serotonin reuptake inhibitors and non-steroidal anti-inflammatory drugs. This may have public health implications owing to the high prevalence of use of both groups of drugs in most countries.
Our study may have several limitations. A preferenrial prescription of selective serotonin reuptake inhibitors for patients with peptic ulcers that subsequently bleed can be ruled out with reasonable confidence because the risk seems to remain constant over treatment duration. A diagnosis or referral bias also seems improbable because the association between selective serotonin reuptake inhibition and gastrointestinal bleeding was uncertain for most general practitioners over the study period. Furthermore, we considered only severe cases requiring referral or admission to hospital. Prescription data in the general practice research database are considered complete, so misclassification of antidepressant use was unlikely. The review of patients was performed blinded to drug exposure. Finally, efforts were made to control for potential confounders but, as in any epidemiological study, the possibility still exists for residual confounding as a result of unmeasured or inaccurately measured risk factors.
What is already known on this topic
Case reports have suggested an association between selective serotonin reuptake inhibitors and bleeding disorders
More formal evidence from epidemiological studies has been lacking
What this paper adds
This population based case-control study shows that selective serotonin reuptake inhibitors increase the risk of upper gastrointestinal bleeding by threefold The risk is similar with all the inhibitors showing that the it is a class effect
Evidence exists for a clinically relevant interaction between these antidepressants and non-steroidal anti-inflammatory drugs
We thank the general practitioners.
Funding: The validation of cases was supported in part by a grant from Novartis. FJdeA was supported by a grant from Fondo de Investigaciones Sanitarias (98/5006).
Competing interests: For the past 5 years LAGR has received research grants from Novartis, manufacturer of several antidepressants.
[1] Yaryura-Tobias JA, Kirschen H, Ninan P, Mosberg HJ. Fluoxetine and bleeding in obsessive-compulsive disorder. Am J Psychiatry 1991;148:949.
[2] Alderman CP, Moritz CK, Ben-Tovim DL. Abnormal platelet aggregation associated with fluoxetine therapy. Ann Pharmacother 1992;26:1517-9.
[3] Evans TG, Buys SS, Rodgers GM. Acquired abnormalities of platelet function. N Engl J Med 1991;324:1671.
[4] Ottervanger JP, Stricker BHCH, Huls J, Weeda JN. Bleeding attributed to the intake of paroxetine. Am J Psychiatry 1994;151:781.
[5] Tielens JAE. Vitamin C for paroxetine and fluvoxamine-associated bleeding. Am J Psychiatry 1997;153:883.
[6] Montero D, Coulson R, De Abajo FJ, Martin Serrano G, Prieto M, Moore N. Selective serotonin reuptake inhibitors and bleeding disorders. Fourth annual meeting of the European Society of Pharmacovigilance. Lisbon: ESOP, 1996.
[7] Anon. Bruising and bleeding with SSRIs. WHO ADR Newsletter 1998;3:l.
[8] Sanders-Bush E, Mayer SE. 5-Hydroxytryptamine (serotonin) receptor agonists and antagonists. In: Hardman JG, Limbird LE, Milinoff PB, Ruddon RW, Goodman LS, Gilman AG, eds. Goodman and Gilman's the pharmacological basis of therapeutics, 9th ed. New York: McGraw-Hill, 1996:24963.
[9] Li N, Waller NF, Ladjervadi M, Hjemdahl P. Effects of serotonin on platelet activation in whole blood. Blood Coagul Fibrinolysis 1997;8:517-23.
[10] Lesch KP, Wolozin BL, Murphy DL, Reiderer R. Primary structure of the human platelet serotonin uptake site: identity with the brain serotonin transporter. J Neurochem 1993;60:2319-22.
[11] Wagner A, Montero D, Martensson B, Siwers B, Asberg M. Effects of fluoxetine treatment of platelet 3H-imipramine binding, 5-HT uptake and 5-HT content in major depressive disorder. J Affect Dis 1990;20: 101-13.
[12] Ross SB, Apenia B, Beck-Friis J, Jansa S, Wetteberg L, Aberg A. Inhibition of 5-hydroxytryptamine uptake in human platelets by antidepressants agents in vivo. Psychopharmacology 1980;67:1-7.
[13] Garcia Rodriguez LA, Jick H. Risk of upper gastrointestinal bleeding and perforation associated with individual nonsteroidal anti-inflammatory drugs. Lancet 1994;343:769-72.
[14] Garcia Rodriguez LA, Perez Gutthann S. Use of the UK general practice research database for pharmacoepidemiology. Br J Clin Pharmacol 1998;45:419-25.
[15] Jick H, Jick SS, Derby LE. Validation of information recorded on general practitioner based computerised data resource in the United Kingdom. BMJ 1991;302:766-8.
[16] Jick H, Terris BZ, Derby LE, Jick SS. Further validation of information recorded on a general practitioner based computerized data resource in the United Kingdom. Pharmacoepidemiol Drug Safety 1992;1:347-9.
[17] Potter WZ, Rudorfer MV, Manji H. The pharmacological treatment of depression. N Engl J Med 1991;325:633-42.
[18] Baldessarini R. Drugs and treatment of psychiatric disorders--depression and mania. In: Hardman JG, Limbird LE, Milinoff PB, Ruddon RW, Goodman LS, Gilman AG, eds, Goodman and Gilman's the pharmacological basis of therapeutics, 9th ed. New York: McGraw-Hill, 1996:431-59.
[19] Lancaster SG, Gonzalez JP. Dothiepin--a review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy in depressive illness. Drugs 1989;38:123-47.
[20] Rothman K. Modern epidemiology. Boston: Little, Brown, 1986. 21 Perez Gutthann, Garcia Rodriguez LA, Raford DS. Individual nonsteroidal antiinflammatory drugs and other risk factors for upper gastrointestinal bleeding and perforation. Epidemiology 1997;8:18-24.
[22] Skop BP, Brown TM. Potential vascular and bleeding complications of treatment with selective serotonin reuptake inhibitors. Psychosomatics 1996;37:12-6.
[23] Marek GJ, McDougle CJ, Price LH, Seiden LS. A comparison of trazodone and fluoxetine: implications for a serotoninergic mechanism of antidepressant action. Psychopharmacology 1992;109:2-11.
[24] Ishikawa K, Shibanoki S, Kubo T, Watabe S, Matsumoto A, Kogure M. Effects of various tricyclic antidepressants on amine uptake. Eur J Pharmacol 1986;120:63-8.
(Accepted 23 August 1999)
Editorial
by Li Wan Po
Division de Farmacoepidemiologia y Farmacovigilancia, Agencia Espanola del Medicamento, 28220
Majadahonda, Madrid, Spain Francisco J de Abajo head
Safety Evaluation Unit, Division de Farmacoepidemiologia y Farmacovigilancia, Agencia Espanola del Medicamento Dolores Montero head
Centro Espanol de Investigacion Farmacoepidemiologica, Madrid, Spain Luis A Garda Rodriguez director
Correspondence to: FJ de Abajo fabajo@agemed.es
BMJ 1999;319:1106-93
COPYRIGHT 1999 British Medical Association
COPYRIGHT 2000 Gale Group