ROCHESTER, MINN. -- Medicine may be on the verge of an explosion in new synthetic antifungal agents comparable to that seen in the antiviral arena in recent years.
A rich pharmaceutical pipeline makes this "a pretty exciting time in antifungal therapy. I think we're going to see some big changes," Dr. Michael R. Keating predicted at a dermatology meeting sponsored by the Mayo Foundation.
A boom in antifungal options is long overdue. "This is an area where we have a desperate need, a critical need, for new agents," stressed Dr. Keating, an infectious disease specialist at the Mayo Clinic.
That's because over the last few decades the population at risk for systemic mycoses has ballooned. The explanation is multifaceted, including greater use of organ transplantation, cancer chemotherapy immunomodulatory therapy for inflammatory disorders, and implanted prosthetic devices. And then there's the AIDS epidemic.
Meanwhile, significant resistance has emerged to the limited repertoire of existing agents, and important new systemic fungal pathogens have emerged in the last 10 years. For example, at many tertiary care centers, cases of candidiasis due to Candida albicans are now outnumbered by cases of fluconazole-resistant C. glabrata and C. krusei, he continued.
So what's on the horizon? Third-generation triazoles are, for one thing.
Furthest along in clinical trials is voriconazole; both oral and intravenous preparations are under intensive investigation. Voriconazole is a broad-spectrum agent that is very active against Aspergillus, Candida species, and important emerging pathogens such as Acreinonium, Scedosporium, and Fusarium. It is quite well tolerated, although 15% of treated patients experience a transient "flashing light" phenomenon, Dr. Keating said at the meeting, which was also sponsored by the Minnesota Dermatologic Society.
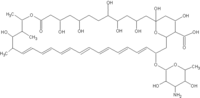
Nystatin is a drug that has managed to retain its antifungal activity despite decades of use. What's new here is the development of a liposomal form that is under investigation for systemic use.
Nikkomycin is an investigational chitin synthase inhibitor with "some real potential," in Dr. Keating's view Chitin is an essential component of the cell wall of yeasts and molds and therefore a great target for a novel agent. Yet nikkomycin appears to have only a limited spectrum of activity: It is active against Candida, Coccidioides, Blastomyces, and Histoplasma species. Combined with an azole, however, nikkomycin exhibits impressive synergy against these pathogens as well as against Aspergillus species.
Echinocandins and pneumocandins work by inhibiting glucan synthase, which produces glucan, another essential cell wall component of yeasts and molds. Merck, Eli Lilly, and other companies are now shepherding echinocandins and pneumocandins through phase II and III trials in the treatment of esophageal candidiasis, invasive candidiasis, and aspergillosis, Dr. Keating noted.
Echinocandins are active against Aspergillus and Canidida species; pneumocandins have a similar spectrum but in addition are active against Pneumocystis. Neither, however, is active against Cryptococcus--a real drawback, he said.
Allylamines and thiocarbamates inhibit the enzyme squalence epoxidase. This action interferes with production of ergosterol, an essential fungal cell wall component that's also the target of amphotericin. Terbinafine, the first allylamine on the market, has recently been shown to be effective against Sporothrix. "We may see expanded labeling for this drug," according to Dr. Keating.
But again, the exciting new finding for terbinafine is its apparent potent synergy in combination with other agents, including fluconazole and itraconazole, he added.
Pradimicins and benanomicins are broadspectrum antifungal agents with a unique action. They work by binding cell wall mannoproteins in a calcium-dependent manner. They appear safe thus far but are in a very early stage of development.
Three different lipid preparations of amphotericin B are now commercially available: Abelcet, AmBisome, and Amphotec. There's no question that the liposomal preparations are less nephrotoxic, generally safer, and better tolerated than conventional amphotericin B, Dr. Keating said. The big unanswered question is: Are they truly more effective?
The lack of data on relative efficacy makes it difficult to use these agents intelligently, particularly in light of their high cost. For example, the average wholesale price of AmBisome at a dose of 3 mg/kg is $506/day, or $7,084 for a 2-week course. At 5 mg/kg, a 2-week course costs $12,250. "And if we're treating aspergillosis we're talking 4-6 weeks of therapy," Dr. Keating noted.
Amphotec has only one labeled indication: treatment of invasive aspergillosis. But there are clinical data to suggest the agent also has efficacy against invasive candidiasis, cryptococcal infection, and neutropenic fever.
AmBisome is FDA approved for empiric therapy of presumed fungal infection in patients with neutropenic fever, as well as for aspergillosis, candidiasis, or cryptococcal infection refractory to or intolerant of conventional amphotericin B deoxycholate.
Abelcet is indicated for the treatment of invasive fungal infections where conventional amphotericin B is ineffective or not tolerated.
Look for greater use of combinations of existing and novel antifungal drugs as multidrug therapy comes under increasing formal scrutiny in clinical trials. For example, there are good data to show enhanced survival when patients with invasive aspergillosis receive a combination of amphotericin B and the nucleoside analog 5-flucytosine, compared with amphotericin B alone.
The same combination was earlier shown to be the treatment of choice for cryptococcal meningitis and other serious cryptococcal infections, he commented.
But the story of combination therapy is a complex one. Within infectious disease circles, there is a hotly debated theoretic concern about antagonism, which appears to be borne out by animal studies involving certain drug combinations.
For example, itraconazole and amphotericin B were antagonistic in animal models of aspergillosis, while fluconazole and amphotericin were synergistic in models of cryptococcal and candidal infection.
"I think this is a very confusing area that's probably going to have to be worked out agent by agent and organism by organism," Dr. Keating said.
COPYRIGHT 2000 International Medical News Group
COPYRIGHT 2001 Gale Group