Diabetes is a chronic disease affecting carbohydrate, protein, and fat metabolism. Hyperglycemia is caused by a defect in insulin regulation affecting either insulin production or insulin action. The diagnosis and management of diabetes has changed significantly over the last 5 years. Diagnostic criteria have become more refined with lower glucose values indicating clinical diabetes. Much of the change in diagnostic criteria is based on research indicating increased risk for macrovascular complications at these lower glucose values (American Diabetes Association [ADA], 2004a). The change in diagnostic criteria is expected to identify individuals early in the course of the disease, thereby decreasing the impact of chronic complications such as macrovascular disease.
The prevalence of diabetes continues to increase, with 1997 estimates at 10.4 million Americans with diabetes, and about 5.4 million Americans with undiagnosed diabetes (ADA, 2001). It is well known that the prevalence of diabetes increases with age; however, additional factors include obesity, life style, and changing demographic factors (ADA, 2001; Boyle, Honeycutt, Venkat Narayan, Hoerger, Geiss, et al, 2001). Type 2 diabetes is an emerging epidemic, particularly among children and young adults (Kaufman, 2002). The increase in Type 2 diabetes parallels the rise in obesity and physical inactivity seen worldwide, and it is estimated that another 16 million Americans have impaired glucose tolerance or impaired fasting glucose tolerance, also called prediabetes (ADA, 2001).
The Diagnosis and Classification of Diabetes Mellitus (ADA, 2004a) updated the classifications of diabetes in 1997. These new classifications use terms based on the pathophysiology of diabetes versus defining diabetes with terms based on pharmacology. There are four clinical classes of diabetes: Type 1, Type 2, gestational diabetes, and other specific types of diabetes (ADA, 1998, 2004a). Hyperglycemia that does not meet the specific criteria for clinical diabetes is classified as either impaired fasting glucose or impaired glucose tolerance, also called pre-diabetes (ADA, 2004c). Table 1 outlines the classifications of diabetes with the appropriate clinical characteristics. Screening and diagnostic criteria for the non-pregnant adult have also changed. Table 2 summarizes the ADA's screening and diagnostic recommendations for clinical diabetes.
As the ability to diagnose diabetes has improved, so have treatment tools, which include better glucose monitoring, better medication options, and a better understanding of the role of meal planning and exercise. The primary goal of diabetes management is to maintain blood glucose as close to normal as possible. Management of diabetes is a team approach that includes the dietician, diabetes nurse educator, pharmacist, psychologist, the physician or nurse practitioner, and most importantly, the patient. Diabetes management requires a lifestyle change and active participation from the patient. If nurses neglect to understand the patient's lifestyle needs, all the best efforts to affect change will fail.
The Diabetes Control and Complications Trial was the first large, prospective study to show that improved glucose control can affect the development of long-term complications (ADA, 2003a). In this study, "there was a 60% reduction in risk between the intensive treatment group and the standard treatment group in diabetic retinopathy, nephropathy, and neuropathy" (ADA, 2003a, p. S25). The United Kingdom Prospective Diabetes Study documented similar results for patients with Type 2 diabetes (ADA, 2002). Daily glucose monitoring is the outcomes measure for the success of meal planning, exercise, and medications. Management goals need to address both pre-prandial and post prandial glucose values. Laboratory tests such as the hemoglobin A1C are also useful measures of glycemic control but do not replace daily glucose monitoring. Goals of glucose management, as published by the ADA (2004d) include fasting values of 70 to 120 mg/dl, postprandial values of 100 to 140 mg/dl, and hemoglobin A1C values of
Management of Diabetes
Medical nutrition therapy is the cornerstone for management of clinical diabetes and impaired glucose tolerance (pre-diabetes). The standard calorie "ADA diets" are no longer recognized as appropriate therapy (Hirsch, 2002). Preprinted calorie-based "diets" do not offer the opportunity to determine the patient's individual needs or food preferences. Nurses should give more attention to the patient's understanding of the nutrient effect of foods on blood glucose levels, and specific recommendations should then be tailored to the patient's nutrition requirements and medication plan. The ADA (2002a) has published a position statement detailing current nutrition recommendations (see Table 3).
Exercise has long been recognized as an adjunct to meal planning. The Diabetes Prevention Program randomized individuals into one of three groups. These are "the intensive nutrition and exercise counseling ('lifestyle') group, or either of two masked medication treatment groups: the biguanide metformin group or the placebo group" (ADA, 2002b, p. 743). The lifestyle group averaged "a 58% relative reduction in the progression to diabetes" (ADA, 2002b, p. 743). This data further support the importance of exercise with meal planning as part of the lifestyle prescription for treating hyperglycemia. Participants in this study exercised an average of 150 minutes per week at a moderate intensity. Additional exercise benefits include assisted weight loss, decreased cardiovascular risk factors (such as hypertension and hyperlipidemia), improved insulin sensitivity and glucose tolerance, decreased anxiety and depression, and improved overall sense of well-being (ADA, 1998). As with all aspects of diabetes management, exercise needs to be individualized.
Medications become part of the treatment plan for individuals with Type 2 diabetes when meal planning and exercise are no longer effective in achieving glucose goals. In the U.S., over 60% of patients with diabetes are on some form of pharmacology intervention to achieve target blood glucose goals. Pharmacology support can be achieved through a variety of oral antidiabetic medications, insulin, or a combination of oral medications and insulin. In Type 1 diabetes, an absolute insulin deficiency is the primary defect; therefore, insulin is the only appropriate choice and is part of the management plan from the time of diagnosis. The pathophysiology of Type 2 diabetes is complicated by increased hepatic glucose output, insulin resistance at the cellular level, and a relative insulin deficiency. Understanding the pathophysiology for Type 2 diabetes is important when considering the appropriate form of drug therapy. In the patient with Type 2 diabetes, the selection of medications (oral antidiabetic agents or insulin) is based on several criteria including the degree of hyperglycemia, presence of concurrent disease, age, weight, patient motivation, and the patient's ability to manage self-care regimes (ADA, 1998).
There are now 5 separate classes of oral medications. Not all of these medications have hypoglycemia as a side effect; therefore, they are no longer referred to as oral hypoglycemic agents, but rather as oral antidiabetic agents. Oral medications can be prescribed as monotherapy or used as combination therapy. Table 4 lists the class of medication along with the generic name, brand name, and dosages for some of the more common oral medications. Insulin is the treatment of choice for the following:
* Patients with Type 1 diabetes.
* Patients with Type 2 diabetes who no longer respond to oral antidiabetic agents.
* Patients with stress hyperglycemia, steroid-induced hyperglycemia, or cystic fibrosis-related diabetes.
* Patients with Type 2 diabetes with comorbidity such as liver or kidney disease.
* Patients with diabetes who are pregnant.
Insulin is available as rapid-acting, short-acting, intermediate-acting, long-acting, and premixed preparations. Animal insulin is no longer in use, having been replaced by synthetic preparations that are structurally identical to human insulin. In the last 5 years, insulin analogs have been developed. These differ from human insulin by changes in the amino acid chains. Three rapid-acting preparations are lispro (Humalog®), aspart (Novolog®), and glulisine (Apidra®). Glargine (Lantus®) is a long-acting analog, with a second long-acting analog scheduled for release later this year.
There are several premixed analog and human insulin preparations available in the U.S. While these preparations do not allow for the flexibility needed to manage Type 1 diabetes, these preparations can be useful for some patients with Type 2 diabetes who may not have the ability to manage multiple types of insulin. Finding the insulin combination that works most efficiently with the patient's lifestyle has been the greatest challenge of managing diabetes.
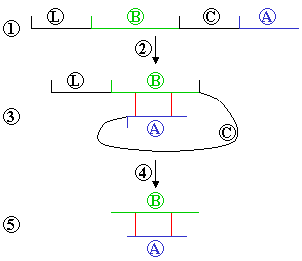
Endogenous insulin is released directly into the portal circulation as a "basal/bolus" combination (ADA, 2004b & c). The "basal" insulin is the 50% continuous insulin release necessary for maintaining normal glucose levels, with the "bolus" insulin carefully timed to match meal-related increases in blood glucose levels (ADA, 2004b & c). Much of diabetes management is attempting to replicate this pattern with the additional challenges of altered insulin absorption and fluctuating patient lifestyles.
Traditionally, exogenous insulin was administered approximately 30 minutes before a meal to overcome some of the issues with insulin absorption and slower onset of action. However, many patients find this "lag time" difficult to achieve on a consistent basis. The introduction of rapid-acting insulin (such as lispro and aspart) has given the practitioner another alternative for a faster preprandial insulin response. Insulin schedules are determined based on the patient's lifestyle, meal patterns, and blood glucose levels. Any number of combinations of insulin are possible. Table 5 lists some of the available insulin preparations including onset, peak, and duration times.
Future Management Options
The future of diabetes holds much promise. Research has introduced new information on the prevention or delay of Type 2 diabetes. In addition, new research on islet cell transplants and pancreas transplants holds promise for a possible cure for Type 1 diabetes. Glucose sensor technology promises to provide better methods for measuring blood glucose. New products are being developed, such as the GlucoWatch® Biographer by Cygnus and the Continuous Glucose Monitoring Sensor® by Medtronic/MiniMed. These devices are new and have not yet found a place in daily management; however, they provide some interesting options for the future.
More insulin formulations and additional changes in oral antidiabetic medications continue to offer expanding options for medication management. Insulin delivery systems have improved to help make intensive insulin management easier to incorporate into daily management. Insulin pumps offer new options, including the ability to communicate with a blood glucose meter and to calculate "insulin on board." New insulin delivery options, such as inhaled insulin, continue to show promise in research trials. The role of health care providers is to continue to strive for tight glycemic control in patient management and to keep patients motivated and engaged in their health care. Nurses need to continue to follow the changing trends in diabetes management to offer patients the best tools and information available.
This article, co-provided by AAACN and Anthony J. Jannetti, Inc., provides 1.0 contact hour. Anthony J. Jannetti, Inc. (AJJ) is accredited as a provider of continuing nursing education by the American Nurses' Credentialing Center's Commission on Accreditation (ANCC-COA). AAACN is a provider approved by the California Board of Registered Nursing Provider Number CEP 5336, for 1.0 contact hour.
This article was reviewed and formatted for contact hour credit by Sally S. Russell, MN, CMSRN, AAACN Education Director, and Rebecca Linn Pyle, MS, RN, Editor.
References
American Diabetes Association. (2004a). Diagnosis and classifications of diabetes mellitus. Diabetes Care, 27(Suppl. 1), S5-S10.
American Diabetes Association. (2004b). Intensive diabetes management (3rd ed.). Alexandria, VA: Author.
American Diabetes Association. (2004c). Medical management of Type 1 diabetes (4th ed.). Alexandria, VA: Author.
American Diabetes Association. (2004d). Standards of medical care in diabetes. Diabetes Care, 27(Suppl. 1), S15-S35.
American Diabetes Association. (2003a). Implications of the diabetes control and complications trial. Diabetes Care, 26(Suppl, 1), S25-S27.
American Diabetes Association. (2003b). Implications of the United Kingdom Prospective Diabetes Study. Diabetes Care, 26(Suppl. 1), S28-S32.
American Diabetes Association. (2002a). Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes-related complications. Diabetes Care, 25(Suppl. 1). S50-S60.
American Diabetes Association. (2002b). The prevention or delay of Type 2 diabetes. Diabetes Care, 25, 742-749.
American Diabetes Association. (1998). Medical management of Type 2 diabetes (4th ed.). Alexandria, VA: Author.
Boyle, J.P., Honeycutt, A.A., Venkat Narayan, K.M., Hoerger, T.J., Geiss, LS., Chen, H., Thompson, T.J. (2001). Projection of Diabetes Burden through 2050. Diabetes Care, 24, 1936-1940.
Hirsch, I.B. (2002). The death of the "1800-calorie ADA diet." Clinical Diabetes, 20, 51-52.
Kaufman, F.R. (2002). Type diabetes in children and young adults: A "new epidemic." Clinical Diabetes, 20, 217-218.
Lewis, G. (1998). Drug therapy in diabetes management. Nurse Practitioner Forum, 9, 58-65.
Murphy, J.L. (Ed.). (2004). Monthly prescribing reference. New York: Prescribing Reference, Inc.
Ginny Lewis, MN, ARNP CDE
Ginny Lewis, MN, ARNP, CDE, is a Nurse Practitioner, Diabetes Care Center, University of Washington Medical Center, Seattle, WA. She may be reached at ginlewis@u.washington.edu
Copyright American Academy of Ambulatory Care Nursing Jul/Aug 2004
Provided by ProQuest Information and Learning Company. All rights Reserved

![The structure of insulin Red: carbon; green: oxygen; blue: nitrogen; pink: sulfur. The blue/purple ribbons denote the skeleton [-N-C-C-]n in the protein's amino acid sequence H-[-NH-CHR-CO-]n-OH where R is the part protruding from the skeleton in each amino acid. The structure of insulin Red: carbon; green: oxygen; blue: nitrogen; pink: sulfur. The blue/purple ribbons denote the skeleton [-N-C-C-]n in the protein's amino acid sequence H-[-NH-CHR-CO-]n-OH where R is the part protruding from the skeleton in each amino acid.](pics/Apidra_1.jpg)