Definition
Malaria is a serious, infectious disease spread by certain mosquitoes. It is most common in tropical climates. It is characterized by recurrent symptoms of chills, fever, and an enlarged spleen. The disease can be treated with medication, but it often recurs. Malaria is endemic (occurs frequently in a particular locality) in many third world countries. Isolated, small outbreaks sometimes occur within the boundaries of the United States.
Description
Malaria is not a serious problem in the United States. Within the last 10 years, only about 1200 cases have been reported each year in this country, mostly by people who were infected elsewhere. Locally transmitted malaria has occurred in California, Florida, Texas, Michigan, New Jersey, and New York City. While malaria can be transmitted in blood, the American blood supply is not screened for malaria. Widespread malarial epidemics are far less likely to occur in the United States, but small, localized epidemics could return to the western world.
The picture is far more bleak outside the territorial boundaries of the United States. A recent government panel warned that disaster looms over Africa from the disease. Malaria infects between 300 and 500 million people every year in Africa, India, southeast Asia, the Middle East, Oceania, and Central and South America. About 2 million of the infected die each year. Most of the cases and almost all of the deaths occur in sub-Saharan Africa. At the present time, malaria kills about twice as many people as does AIDS. As many as half a billion people worldwide are left with chronic anemia due to malaria infection. In some parts of Africa, people battle up to 40 or more separate episodes of malaria in their lifetimes. The spread of malaria is becoming even more serious as the parasites that cause malaria develop resistance to the drugs used to treat the condition.
Causes & symptoms
Human malaria is caused by four different species of a parasite called plasmodium: Plasmodium falciparum (the most deadly), P.vivax, P. malariae, and P. ovale. The last two are fairly uncommon. Many animals can get malaria but human malaria does not spread to animals. In turn, animal malaria does not spread to humans.
A person gets malaria when bitten by a female mosquito who is looking for a blood meal and is infected with the malaria parasite. The parasites enter the blood stream and travel to the liver, where they multiply. When they re-emerge into the blood, symptoms appear. By the time a patient shows symptoms, the parasites have reproduced very rapidly, clogging blood vessels and rupturing blood cells.
Malaria cannot be casually transmitted directly from one person to another. Instead, a mosquito bites an infected person and then passes the infection on to the next human it bites. It is also possible to spread malaria via contaminated needles or in blood transfusions. This is why all blood donors are carefully screened with questionnaires for possible exposure to malaria.
The amount of time between the mosquito bite and the appearance of symptoms varies, depending on the strain of parasite involved. The incubation period is usually between 8 and 12 days for falciparum malaria, but it can be as long as a month for the other types. Symptoms from some strains of P.vivax may not appear until 8-10 months after the mosquito bite occurred.
The primary symptom of all types of malaria is the "malaria ague" (chills and fever). In most cases, the fever has three stages, beginning with uncontrollable shivering for an hour or two, followed by a rapid spike in temperature (as high as 106°F), which lasts three to six hours. Then, just as suddenly, the patient begins to sweat profusely, which will quickly bring down the fever. Other symptoms may include fatigue, severe headache, or nausea and vomiting. As the sweating subsides, the patient typically feels exhausted and falls asleep. In many cases, this cycle of chills, fever, and sweating occurs every other day, or every third day, and may last for between a week and a month. Those with the chronic form of malaria may have a relapse as long as 50 years after the initial infection.
Falciparum malaria is far more severe than other types of malaria because the parasite attacks all red blood cells, not just the young or old cells, as do other types. It causes the red blood cells to become very "sticky." A patient with this type of malaria can die within hours of the first symptoms. The fever is prolonged. So many red blood cells are destroyed that they block the blood vessels in vital organs (especially the kidneys), and the spleen becomes enlarged. There may be brain damage, leading to coma and convulsions. The kidneys and liver may fail.
Malaria in pregnancy can lead to premature delivery, miscarriage, or stillbirth.
Certain kinds of mosquitoes (called anopheles) can pick up the parasite by biting an infected human. (The more common kinds of mosquitoes in the United States do not transmit the infection.) This is true for as long as that human has parasites in his/her blood. Since strains of malaria do not protect against each other, it is possible to be reinfected with the parasites again and again. It is also possible to develop a chronic infection without developing an effective immune response.
Diagnosis
Malaria is diagnosed by examining blood under a microscope. The parasite can be seen in the blood smears on a slide. These blood smears may need to be repeated over a 72-hour period in order to make a diagnosis. Antibody tests are not usually helpful because many people developed antibodies from past infections, and the tests may not be readily available.
Anyone who becomes ill with chills and fever after being in an area where malaria exists must see a doctor and mention their recent travel to endemic areas. A person with the above symptoms who has been in a high-risk area should insist on a blood test for malaria. The doctor may believe the symptoms are just the common flu virus. Malaria is often misdiagnosed by North American doctors who are not used to seeing the disease. Delaying treatment of falciparum malaria can be fatal.
Treatment
Falciparum malaria is a medical emergency that must be treated in the hospital. The type of drugs, the method of giving them, and the length of the treatment depend on where the malaria was contracted and how sick the patient is.
For all strains except falciparum, the treatment for malaria is usually chloroquine (Aralen) by mouth for three days. Those falciparum strains suspected to be resistant to chloroquine are usually treated with a combination of quinine and tetracycline. In countries where quinine resistance is developing, other treatments may include clindamycin (Cleocin), mefloquin (Lariam), or sulfadoxone/pyrimethamine (Fansidar). Most patients receive an antibiotic for seven days. Those who are very ill may need intensive care and intravenous (IV) malaria treatment for the first three days.
Anyone who acquired falciparum malaria in the Dominican Republic, Haiti, Central America west of the Panama Canal, the Middle East, or Egypt can still be cured with chloroquine. Almost all strains of falciparum malaria in Africa, South Africa, India, and southeast Asia are now resistant to chloroquine. In Thailand and Cambodia, there are strains of falciparum malaria that have some resistance to almost all known drugs.
A patient with falciparum malaria needs to be hospitalized and given antimalarial drugs in different combinations and doses depending on the resistance of the strain. The patient may need IV fluids, red blood cell transfusions, kidney dialysis, and assistance breathing.
A drug called primaquine may prevent relapses after recovery from P. vivax or P. ovale. These relapses are caused by a form of the parasite that remains in the liver and can reactivate months or years later.
Another new drug, halofantrine, is available abroad. While it is licensed in the United States, it is not marketed in this country and it is not recommended by the Centers for Disease Control and Prevention in Atlanta.
Alternative treatment
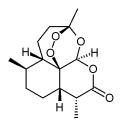
The Chinese herb qiinghaosu (the western name is artemisinin) has been used in China and southeast Asia to fight severe malaria, and became available in Europe in 1994. Because this treatment often fails, it is usually combined with another antimalarial drug (mefloquine) to boost its effectiveness. It is not available in the United States and other parts of the developed world due to fears of its toxicity, in addition to licensing and other issues.
A western herb called wormwood (Artemesia annua) that is taken as a daily dose can be effective against malaria. Protecting the liver with herbs like goldenseal (Hydrastis canadensis), Chinese goldenthread (Coptis chinensis), and milk thistle (Silybum marianum) can be used as preventive treatment. Preventing mosquitoes from biting you while in the tropics is another possible way to avoid malaria.
Prognosis
If treated in the early stages, malaria can be cured. Those who live in areas where malaria is epidemic, however, can contract the disease repeatedly, never fully recovering between bouts of acute infection.
Prevention
Several researchers are currently working on a malarial vaccine, but the complex life cycle of the malaria parasite makes it difficult. A parasite has much more genetic material than a virus or bacterium. For this reason, a successful vaccine has not yet been developed.
Malaria is an especially difficult disease to vaccinate against because the parasite goes through several separate stages. One recent, promising vaccine appears to have protected up to 60% of people exposed to maleria. This was evident during field trials for the drug that were conducted in South America and Africa. It is not yet commercially available.
The World Health Association (WHO) has been trying to eliminate malaria for the past 30 years by controlling mosquitoes. Their efforts were successful as long as the pesticide DDT killed mosquitoes and antimalarial drugs cured those who were infected. Today, however, the problem has returned a hundredfold, especially in Africa. Because both the mosquito and parasite are now extremely resistant to the insecticides designed to kill them, governments are now trying to teach people to take antimalarial drugs as a preventive medicine and avoid getting bitten by mosquitoes.
Travelers to high-risk areas should use insect repellant containing DEET for exposed skin. Because DEET is toxic in large amounts, children should not use a concentration higher than 35%. DEET should not be inhaled. It should not be rubbed onto the eye area, on any broken or irritated skin, or on children's hands. It should be thoroughly washed off after coming indoors.
Those who use the following preventive measures get fewer infections than those who do not:
- Between dusk and dawn, remain indoors in well-screened areas.
- Sleep inside pyrethrin or permethrin repellent-soaked mosquito nets.
- Wear clothes over the entire body.
Anyone visiting endemic areas should take antimalarial drugs starting a day or two before they leave the United States. The drugs used are usually chloroquine or mefloquine. This treatment is continued through at least four weeks after leaving the endemic area. However, even those who take antimalarial drugs and are careful to avoid mosquito bites can still contract malaria.
International travelers are at risk for becoming infected. Most Americans who have acquired falciparum malaria were visiting sub-Saharan Africa; travelers in Asia and South America are less at risk. Travelers who stay in air conditioned hotels on tourist itineraries in urban or resort areas are at lower risk than backpackers, missionaries, and Peace Corps volunteers. Some people in western cities where malaria does not usually exist may acquire the infection from a mosquito carried onto a jet. This is called airport or runway malaria.
Key Terms
- Arteminisinins
- An antimalarial family of products derived from an ancient Chinese herbal remedy. Two of the most popular varieties are artemether and artesunate, used mainly in southeast Asia in combination with mefloquine.
- Chloroquine
- This antimalarial drug was first used in the 1940s, until the first evidence of quinine resistance appeared in the 1960s. It is now ineffective against falciparum malaria almost everywhere. However, because it is inexpensive, it is still the antimalarial drug most widely used in Africa. Native individuals with partial immunity may have better results with chloroquine than a traveler with no previous exposure.
- Mefloquine
- An antimalarial drug that was developed by the United States Army in the early 1980s. Today, malaria resistance to this drug has become a problem in some parts of Asia (especially Thailand and Cambodia).
- Quinine
- One of the first treatments for malaria, quinine is a natural product made from the bark of the Cinchona tree. It was popular until being superseded by the development of chloroquine in the 1940s. In the wake of widespread chloroquine resistance, however, it has become popular again. It or its close relative quinidine can be given intravenously to treat severe falciparum malaria.
- Sulfadoxone/pyrimethamine (Fansidar)
- This antimalarial drug developed in the 1960s is the first drug tried in some parts of the world where chloroquine resistance is widespread. It has been associated with severe allergic reactions due to its sulfa component.
Further Reading
For Your Information
Books
- Desowitz, Robert S. The Malaria Capers: More Tales of Parasites and People, Research and Reality. New York: W.W. Norton, 1993.
- Stoffman, Phyllis. The Family Guide to Preventing and Treating 100 Infectious Illnesses. New York: John Wiley & Sons, 1995.
Periodicals
- Kristof, Nicholas D. "Malaria Makes a Comeback, Deadlier Than Ever." The New York Times (Jan. 8, 1997).
- Mack, Alison. "Collaborative Efforts Under Way to Combat Malaria." The Scientist 10 (May 12, 1997): 1, 6.
- Shell, Ellen Ruppel. "Resurgence of a Deadly Disease." The Atlantic Monthly 280 (August 1997).
Organizations
- Centers for Disease Control Malaria Hotline. (770) 332-4555.
- Centers for Disease Control Travelers Hotline. (770) 332-4559.
Other
- Malaria Foundation. http://www.malaria.org.
Gale Encyclopedia of Medicine. Gale Research, 1999.