Collagenous gastritis is a distinctive disorder characterized by thickening of the subepithelial collagen layer in the gastric mucosa. Although this entity was recognized in 1989, its etiology, pathogenesis, and clinicopathologic features remain poorly understood because of its rarity. An unusual case of collagenous gastritis was observed in a 37-year-old man who presented with profound weight loss, a feature that has not previously been emphasized.
Collagenous gastritis is a rare clinicopathologic entity of unknown etiology that is characterized by thickening of the subepithelial collagen layer (more than 10 µm in thickness) in the gastric mucosa associated with a mixed lamina propria inflammatory cell infiltrate. Since it was first described in 1989,1-3 only 18 cases have been reported worldwide.1-12 This lesion has not been widely recognized by pathologists and gastroenterologists. Although some of the reported cases are associated with other well-characterized diseases such as collagenous colitis,3,4,8-10 lymphocytic colitis," or celiac disease,5,12 the pathogenesis of collagenous gastritis remains obscure. No effective treatment regimens have been described.
To contribute to a better understanding of this disease, we report our experience with a patient that presented with profound weight loss. Collagenous gastritis was the sole abnormality found in the digestive system.
REPORT OF A CASE
The patient was a 37-year-old Hispanic man in excellent health until 2 years ago, when he presented with weight loss, weakness, and postprandial nonbloody diarrhea with 3 or 4 loose stools per day. He lost 14.8 kg during 1 year from a baseline of 60.7 kg. He had no fever, abdominal pain or distress, dysphagia, odynophagia, or sitophobia. Workup at another hospital revealed vitamin B12, deficiency, which was corrected with dietary supplements. Gastrointestinal biopsies at that time were reported as "chronic inflammation" in the colon, "lymphoid hyperplasia suggestive of immunoproliferative small intestinal disorder" in the small intestine, and "chronic gastritis" in the stomach. No Helicobacter pylori were identified in the gastric biopsies. A bone marrow biopsy done at that time showed "hypercellularity with changes consistent with megaloblastic anemia." A test for human immunodeficiency virus was negative. The patient was then started on tetracycline (presumably for empiric treatment of tropical sprue), which he continued for 1 year without symptomatic improvement. A trial course of Asacol was also given but was discontinued because of nausea and vomiting.
Upon presentation to our institution, the patient's symptoms were essentially unchanged, and he complained of some bloating. His social history was remarkable for heavy drinking in high school and 2 drinks per day thereafter. He was a nonsmoker. His family history was unremarkable. Physical examination revealed a cachectic man in no distress. he was afebrile with a pulse of 74 beats per minute, blood pressure 108/60 mm Hg, body weight 43.6 kg, and height 1.7 m. Notable findings were a scaphoid nontender abdomen without organomegaly, lymphadenopathy, or ascites. Perianal and rectal examinations were uninformative. Laboratory studies revealed a white cell count of 8.4 × 10^sup 3^/ µl with normal differential, hemoglobin 13.6 g/dL, hematocrit 40.7%, platelets 221 × 10^sup 3^/µl, mean corpuscular volume 78.4 fL, total serum protein 6.5 g/dL, albumin 3.6 g/dL, aspartate aminotransferase 25 U/L, alanine aminotransferase 18 U/L, lactate dehydrogenase 177 U/L, alkaline phosphatase 275 U/L, [gamma]-glutamyl transpeptidase 19 U/L, uric acid 7.5 mg/dL, total serum iron 100 µg/dL, total iron binding capacity 292 µg/dL, ferritin 56 ng/mL, vitamin B12 464 pg/mL (already on repletion), amylase 102 U/L, lipase 79 U/L, and Westergren sedimentation rate 15 mm/h. Serum anti-parietal-cell antibody screen was negative.
Computed tomography scan revealed unremarkable chest, abdomen, and pelvis. Mild nonspecific dilatation of the left colon was noted, but no evidence of bowel wall thickening was observed. No obstruction, lymphadenopathy, or evidence of malignancy was apparent.
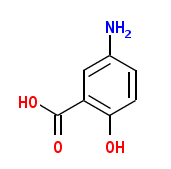
Esophagogastroduodenoscopy revealed normal esophagus, nodular and erythematous gastric mucosa, and granular duodenal mucosa. Colonoscopic findings were essentially normal except for the presence of small benign nodules in the ileum and colon consistent with lymphoid hyperplasia. Histologic examination of the endoscopic biopsies from the gastric antrum revealed a dense, diffuse, and superficial lamina propria lymphoplasmacytic infiltrate with occasional neutrophils. The number of intraepithelial lymphocytes appeared to be slightly increased in the foveolar surface, which also appeared to be mildly damaged (Figure 1). No lymphoid aggregates and no Helicobacter-Yike microorganisms were appreciated. The most striking finding in the gastric biopsies was patchy thickening of the subepithelial collagen layer, which varied from 20 to 120 µm in thickness (Figures 1 and 2). No significant fibrosis was evident in other areas of the lamina propria. These histologie features were consistent with previous description of collagenous gastritis.1-12 The biopsies from the duodenum, ileum, and colon were essentially unremarkable except for the presence of a few prominent lymphoid follicles without lymphoepithelial lesions. There was no histologic evidence of celiac disease, collagenous or lymphocytic enterocolitis, or inflammatory bowel disease. No microorganisms or viral inclusions were identified. However, because 1 of the clinical suspicions was immunoproliferative small intestinal disorder, immunohistochemical studies were performed on the duodenal biopsies. The lamina propria lymphocytes and plasma cells were polyclonal, composed of a mixed population of cells positive for immunoglobulin (Ig) M, IgG, IgA, and [kappa] and [lambda] light chains. Immunostaining for Bcl-2 further confirmed the benign nature of the lymphoid follicles. These findings thus did not support a diagnosis of lymphoproliferative disorder. Review of the prior endoscopic biopsies performed 2 years ago at the other hospital also showed collagenous gastritis with a similar degree of subepithelial collagen deposition. No evidence of lymphoproliferative disorder or other types of enterocolitis was found.
The patient was started on prednisone 40 mg per day and nutrition supplements. Four months later, his body weight had increased to 48.6 kg. A course of metronidazole and ciprofloxacin was also given empirically for bacterial overgrowth. His weight continued to increase and reached 55.3 kg 8 months later as prednisone was tapered by 10 mg per month. Unfortunately, the patient could not taper prednisone without relapse. Azathioprine treatment was then started but had also failed to allow for prednisone taper. Despite escalating doses of azathioprine, the patient's weight continued to fall to 48.1 kg, and prednisone was thus again increased to 30 mg per day by the 14th month along with 175 mg of azathioprine. By the 16th month, his weight improved to 52.2 kg, and his prednisone dose was back down to 20 mg per day. Because the patient had become steroid dependent, budesonide was introduced 20 months later to attempt to reduce the systemic adverse effects while providing effective steroid therapy. Currently, the patient's medications include daily doses of prednisone (20 mg), budesonide (9 mg), and azathioprine (200 mg) and calcium, magnesium, phosphate, iron, vitamins D, and vitamin B1, supplements. His body weight is relatively stable, and he has about 2 stools daily. His most recent biopsy from the gastric antrum still exhibited morphologic features of collagenous gastritis without a significant decrease in the thickness of the collagen band. A recent duodenal biopsy revealed no histopathologic abnormality and no lymphoid follicles.
COMMENT
This unusual case of collagenous gastritis was associated with profound weight loss, a feature that has not previously been emphasized. Although the initial clinical suspicions in this case included immunoproliferative small intestinal disorder and autoimmune enteropathy, extensive workup revealed collagenous gastritis as the only abnormality. The patient's disease was managed relatively successfully with steroid therapy, as indicated by body weight gain.
Collagenous gastritis is an extremely rare and poorly characterized disease that was recognized 10 years ago. The majority of descriptions in the literature are single case reports; one recent report included 6 cases diagnosed in France.4 The etiology and pathogenesis of this disorder are completely unknown. In an analysis of those 6 cases and a review of 8 cases previously reported, Lagorce-Pages et al4 divided the patients with collagenous gastritis into 3 subgroups, 2 of which appear to have distinct clinicopathologic patterns. The first subgroup mainly includes children and young adults with anemia but no evidence of extragastric involvement. The second subgroup mainly includes adults with watery diarrhea and collagenous colitis. The third subgroup does not seem to have any unique clinicopathologic characteristics, although an association with lymphocytic colitis11 or lymphocytic gastritis and celiac disease5,12 may occur. The cause of anemia seen in some of the patients with collagenous gastritis is unclear but may be associated with gastric bleeding secondary to damage of dilated capillaries entrapped in the subepithelial fibrous bands.13 Because collagenous colitis coexists in a subset of the patients with collagenous gastritis and because of the morphologic similarity between these two disorders, the pathogenic mechanisms proposed for collagenous colitis may also be applicable to collagenous gastritis to explain subepithelial collagen deposition. These proposed mechanisms include chronic inflammatory, reparative or autoimmune response to toxic or infectious agents, abnormal function of pericryptal fibroblasts, and collagenization of exudated plasma proteins.4,5,9
Weight loss was documented previously in 5 patients with collagenous gastritis.2,8-10,12 The clinicopathologic features of these cases are summarized with the present case in the Table 1. All 6 patients were adults, and no gender preference is apparent. In 3 of the cases,8-10 weight loss may also be attributed to coexistent collagenous colitis and duodenitis. Collagenous gastritis in those cases appears to be part of the spectrum of collagen deposition disease. In another case, collagenous gastritis may have been an incidental finding; the primary problems were celiac disease and ulcerative colitis.12 In 1 patient with marked weight loss, collagenous gastritis was the sole pathologic finding in the gastrointestinal tract.2 This case is similar to ours in its clinicopathologic features and its therapeutic response. Both patients were treated with prednisone and nutrition supplements and both showed significant improvement in weight gain, although the patient in the previous report eventually died of an unrelated disease.2 It remains unclear why and how collagenous gastritis alone results in such marked weight loss. Symptoms such as anorexia, nausea, vomiting, postprandial fullness, and diarrhea, all presumably secondary to gastric dysfunction, may be responsible. Alternatively, there might be a coexisting functional disorder in the gastrointestinal tract that is not detectable by histopathologic examination. This hypothesis appears to be supported by the fact that steroid therapy is relatively effective in promoting weight gain, but the thickness of the subepithelial collagen band in the stomach does not appear to be affected. However, a similar response (symptomatic improvement with persistent collagen band) has been well documented in patients with collagenous colitis treated with steroids.14
Two other possibilities have been clinically considered. One concerns the histologie findings from the duodenal biopsies. Although no evidence of immunoproliferative small intestine disorder was found and the patient did not show any signs of immunodeficiency, benign lymphoid follicles were noted in the duodenal biopsies on a couple of occasions. The significance of these findings remains unclear, although unusual. The second possibility concerns the coexistence of autoimmune gastritis given the initial observations of vitamin B,2 deficiency and megaloblastic change in the bone marrow 2 years ago at another hospital. Although a Schilling test was not performed and serum anti-intrinsic factor and blocking antibodies were not evaluated, pernicious anemia is unlikely because the patient responded very well to oral vitamin B12 supplement. There was no endoscopic evidence of atrophy in the gastric body, and the serum anti-parietal-cell antibody screen was negative. However, a biopsy from the gastric body has not been performed for histologic examination (all the gastric biopsies were from the antrum). Nevertheless, even if atrophie change were observed, it would not be surprising in a case of collagenous gastritis. In a 12-year follow-up study involving multiple gastric biopsies in one of the earliest reported cases,1 a gradual progression of glandular atrophy was observed and accompanied by endocrine cell hyperplasia, intestinal metaplasia, and epithelial changes indefinite for dysplasia, features similar to those seen in cases of atrophie gastritis.15 We suggest that the findings of mild lymphoid hyperplasia seen in the small intestine and the vitamin B12 deficiency were secondary to bacterial overgrowth, which was empirically treated.
The histopathologic diagnosis of collagenous gastritis is relatively straightforward. The diagnostic criteria are essentially identical to those for collagenous colitis.4 The thickening of the collagen band should be subepithelial in location and at least 10 p,m in thickness, and the band can be patchy or diffuse. This condition should not be confused with more diffuse lamina propria fibrosis, which can be associated with a variety of conditions including a healing ulcer, radiation gastritis, and toxicity caused by nonsteroid anti-inflammatory drugs. The observations of endocrine cell hyperplasia and epithelial dysplasia in patients with long-standing cases of collagenous gastris15 suggest an increased risk in these patients for gastric neuroendocrine tumor and adenocarcinoma.
References
1. Colletti RB, Trainer TD. Collagenous gastritis. Gastroenterology. 1989;97: 1552-1555.
2. Freeman HJ, Piercey JRA, Raine RJ. Collagenous gastritis. Can J Castroenterol. 1989;3:171-174.
3. Borchard F, Niederau C. Kollagene gastroduodenitis. Dtsch Med Wochenschr. 1989:114:1345.
4. Lagorce-Pages C, Fabiani B, Bouvier R, Scoazec JY, Durand L, Flejou JF. Collagenous gastritis: a report of six cases. Am J Surg Pathol. 2001:25:1174-1179.
5. Stancu M, De Petris G, Palumbo TP, Lev R. Collagenous gastritis associated with lymphocytic gastritis and celiac disease. Arch Pathol Lab Med. 2001:125: 1579-1584.
6. Freeman HJ. Topographic mapping of Collagenous gastritis. Can J Castroenterol. 2001:15:475-478.
7. Meunier S, Villard F, Bouvier R, Lachaux A, Bertrand Y. Collagen gastritis, an unusual cause of anemia in children: report of 2 cases. Arch Pediatr. 2001 ;8: 47-50.
8. Stolte M, Ritter M, Borchard F, Koch-Scherrer G. Collagenous gastroduodenitis on Collagenous colitis. Endoscopy. 1990;22:186-187.
9. Castellano VM, Munoz MT, Colina F, Nevado M, Casis B, Solis-Herruzo JA. Collagenous gastrobulbitis and collagenous colitis: case report and review of the literature. Scand J Castroenterol. 1999;34:632-638.
10. Pulimood AB, Ramakrishna BS, Mathan MM. Collagenous gastritis and collagenous colitis: a report with sequential histological and ultrastructural findings. Gut. 1999:44:881-885.
11. Groisman CM, Meyers S, Harpaz N. Collagenous gastritis associated with lymphocytic colitis. J Clin Gastroenterol. 1996;22:134-137.
12. Vesoulis Z, Lozanski G, Ravichandran P. Collagenous gastritis: a case report, morphologic evaluation, and review. Mod Pathol. 2000;13:591-596.
13. Cote JF, Hankard GF, Faure C, et al. Collagenous gastritis revealed by severe anemia in a child. Hum Pathol. 1998:29:883-886.
14. Fernandez-Banares F, Salas A, Esteve M, Espinos J, Forne M, Viver JM. Collagenous and lymphocytic colitis: evaluation of clinical and histological features, response to treatment, and long-term follow-up. Am J Gastroenterol. 2003; 98:340-347.
15. Winslow JL, Trainer TD, Colletti RB. Collagenous gastritis: a long-term follow-up with the development of endocrine cell hyperplasia, intestinal metaplasia, and epithelial changes indeterminate for dysplasia. Am J Clin Pathol. 2001 ;116: 753-758.
Hanlin L. Wang, MD, PhD; Amit G. Shah, MD; Lisa M. Yerian, MD; Russell D. Cohen, MD; John Hart, MD
Accepted for publication October 3, 2003.
From the Lauren V. Ackerman Laboratory of Surgical Pathology, Washington University School of Medicine, St Louis, Mo (Dr Wang); and the Departments of Pathology (Drs Yerian and Hart) and Medicine/ Gastroenterology (Drs Shah and Cohen), University of Chicago Hospitals, Chicago, III.
Reprints: Hanlin L. Wang, MD, PhD, Lauren V. Ackerman Laboratory of Surgical Pathology, Department of Pathology & Immunology, Washington University School of Medicine, Campus Box 8118, 660 South Euclid Ave, St Louis, MO 63110-1093 (e-mail: hwang@path.wustl.edu).
Copyright College of American Pathologists Feb 2004
Provided by ProQuest Information and Learning Company. All rights Reserved