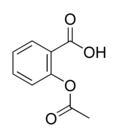
Testing for fecal occult blood can reduce the incidence and mortality from colorectal cancer. An annual screening is recommended for every person 50 years and older. Eating red meat, poultry, fish, certain raw vegetables, or taking some medications can cause false-positive test results. In addition, intake of vitamin C can cause false-negative test results. Few data address the advisability of restricting the use of aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) during the stool specimen collection process for fecal occult blood testing. Various studies have attempted to define this issue but have had different limitations. Clinical guidelines state that it is unclear if low-dose aspirin can cause false-positive test results, and higher doses may cause problems. Kahi and Imperiale evaluated whether the regular use of aspirin or NSAIDs has any effect on the risk of false-positive fecal occult blood tests in patients that are likely to present to family physicians.
The trial design was a prospective cohort study of patients referred to a Veterans Affairs medical center for evaluation of positive fecal occult blood tests over 22 months. All were scheduled for colonoscopy to follow up on the abnormal test. Before the procedure, patients were provided fecal occult blood serial test cards to collect three separate specimens, and the cards were processed in a hospital laboratory. Patients who had significant risk for other gastrointestinal bleeding or were on warfarin (Coumadin) or antiplatelet regimens were excluded from the study.
After the colonoscopy was scheduled, patients were contacted by phone and asked about the use of prescribed medications, medical conditions, their recall of the specimen collection instructions, and their use of over-the-counter NSAIDs. The definition of regular use of aspirin or NSAIDs was at least once daily for at least three days per week at the time of the specimen collection. This was determined by the interview process and by a medical record review. Patients had to have been taking aspirin or NSAIDs for at least one month before the fecal occult blood testing. Aspirin use was divided into three groups, 81 to 324 mg per day, 325 to 649 mg per day, and 650 to 1,250 mg per day. The type of colorectal lesion that could explain a positive fecal occult blood test was the primary outcome measure.
There were 193 participants (98 percent men) in the study, with a mean age of 66 years. In 79 percent of patients there were no colonoscopy findings that could account for the positive fecal occult blood test results. Seventy percent of the participants were defined as regular users of aspirin or NSAIDs. Of these regular users, 21 percent had findings that explained the positive fecal occult blood test, compared with 19 percent of those who were not regular users. When analyzed, there was no association between the dose of aspirin and colonoscopic findings unlikely to explain the positive fecal occult blood test. There was no association between regular aspirin or NSAID use and false-positive fecal occult blood test after multivariate analysis.
The authors conclude that aspirin and NSAID use does not increase the risk for false-positive fecal occult blood tests. They add that their study suggests that these two classes of medications do not need to be restricted when patients are collecting stool samples for fecal occult blood tests.
KARL E. MILLER, M.D.
Kahi CJ, Imperiale TF. Do aspirin and nonsteroidal anti-inflammatory drugs cause false-positive fecal occult blood test results? A prospective study in a cohort of veterans. Am J Med December 1, 2004;117:837-41.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group