Monday
"My hands bleed," Julie proclaimed. "I don't know whether I need to see a doctor or a priest." She smiled weakly and asked, "Do the stigmata itch?" The 34-year-old woman looked worn out. I knew she had her hands full juggling a job and raising two young children. Someone had suggested to Julie that she might possess the stigmata. The palms of her hands were dry and rough, and in some areas the skin was cracked. I could understand how skin like this might weep or bleed on occasion. Although I was sure that Julie's problem was merely a case of mundane bilateral palmar dermatitis, I carefully inspected the rest of her skin and paid special attention to the feet, brow, and trunk. I encouraged Julie to apply moisturizer to her hands during the day and avoid excessively exposing them to water. I gave her a prescription for a potent topical steroid ointment to apply at night and recommended hydroxyzine (Atarax) at bedtime if the pruritus interrupted her sleep. A couple of weeks later, I saw Julie at the gas station. She walked over and held out her hands, palms up. "They're doing great--no more bleeding or itching." My gaze shifted from Julie's hands to her sports utility vehicle (SUV) next to the gas pump. Inside the SUV, a rowdy boy was sticking a piece of chewed bubble gum into his little sister's hair. Julie doesn't have the stigmata, but in my opinion, that doesn't make her any less of a saint.
Tuesday
"I'm curious, doctor. Is it ever normal to urinate blood?" Ivan was an elderly man who seldom came to see me at the office, but he always had plenty of questions. What prompted this query was the development of painless, gross hematuria beginning more than one month ago. "Could it be something I'm eating? Do you think I've been taking too many vitamins?" He exited the office restroom holding a specimen container that we both knew was a urine sample but looked instead like 100 mL of blood. His complete blood count and his glucose, BUN, and creatinine levels were normal. An intravenous pyelogram was obtained and revealed a 5-cm radiolucent filling defect of the bladder. Cystourethroscopy showed a large bladder tumor completely occluding the right ureteric orifice. Transurethral resection of the tumor was performed along with placement of a right ureteral stent. The pathology report described a high-grade transitional cell carcinoma invading the bladder muscle. The urologist recommended a radical cystectomy and ileal conduit as the best chance for a possible cure. Ivan wanted to think it over. After all, he still had lots of questions: "How likely are complications from this type of surgery? Where's the best place to have it done? If I no longer notice any blood in my urine, do I still need such a major operation?" Curiosity is a good thing. When patients ask the right questions, they and their doctors are likely to learn a great deal.
Wednesday
Mrs. Ludwig is a remarkable woman. The 92-year-old widow lives independently and stays active. She has never required any surgical procedures or fractured any bones. The problem list in her chart contains only three items: isolated systolic hypertension, osteoarthritis, and hearing loss. She seems unflappable. I wonder if she lets anything bother her. Today, I ask her a question that I'm certain many others have posed, "What's the secret behind your longevity?" Although I hope to hear about a mysterious tonic or special diet, frankly I expect a response of "clean living" or "just lucky." Her answer is accurate and somehow disappointing. "Genetics," she replies. Her mother lived to be 100 years old. Two sisters are in their 90s. Mrs. Ludwig's mood abruptly changed. "There's nothing wrong with being old as long as your mind doesn't go." She paused and then added, "One of my sisters has Alzheimer's." The thought of dementia scared Mrs. Ludwig more than any other illness. "I know I'm forgetful," she continued, "but I can still think ... can't I?" Her eyes now betrayed her age--full of sorrow and worry. I administered the Mini-Mental State Examination. She scored a 30. "Perfect," I complimented her. "No sign of Alzheimer's disease." Was she convinced? Maybe the only thing worse than losing your mind is living in fear that one day it will likely happen.
Thursday
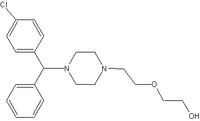
Big, pouty lips are considered stylish by many young women these days. But not everyone desires that large-lip look. "Do something about this," 26-year-old Lynn commanded as she pointed to her lips. They appeared to be about three times larger than usual. She had no difficulty breathing or any trouble swallowing. With the exception of her unusually puffy lips, Lynn's examination was unrevealing--no urticaria, no wheezing, and no swelling of the eyelids, tongue, hands, or feet. She had never experienced this problem before. The swelling had began about one hour earlier without any warning. Lynn had no known allergies and was taking no prescription or over-the-counter (OTC) medications. She had not applied any new lipsticks or cosmetics, and she had not changed the brand of her toothpaste or eaten any different kinds of food recently. I gave her some oral diphenhydramine (Benadryl) and had my nurse keep an eye on her. Within 30 minutes, Lynn's lips had dramatically "deflated." I recommended she take OTC loratadine (Claritin) once every 24 hours for the next few days and apply cool compresses to her lips for the remainder of today. Lynn was delighted by the rapid downsizing of her lips. "I could just kiss you," she said. Naturally, I settled for a "thank you" instead.
Friday
In the course of his high school football career, Tyler has taken more than his share of lumps for the team. There is no telling how many yards of elastic bandages and how many feet of medical tape have helped patch him up. Toward the end of today's game, Tyler was tackled hard and his left shoulder was driven into the ground. He had localized swelling and tenderness over the left acromioclavicular (AC) joint, but no obvious bony deformity. X-rays of his shoulder (with and without the use of weights) displayed slight widening of the AC joint. For his Type II AC joint sprain, I recommended the use of a sling for a few weeks, application of ice, and the use of ibuprofen for pain. When Tyler's pain lessened, I would have him begin range-of-motion and strengthening exercises. "No football for a while," I decreed. On hearing that command, the boy's parents appeared as heartbroken as their son. They requested a second opinion so I arranged an appointment with an orthopedist. He gave them the same advice I did. In my experience, the vast majority of Type I and II AC sprains heal well with only conservative treatment--time and avoidance of additional trauma. Such a simple remedy is not always easily accepted. If Tyler ends up returning to football competition prematurely, then somebody else must've been willing to shoulder the responsibility that I was not.
Saturday/Sunday
Florence hasn't changed much over the years. Before retiring, she was one of those "Renaissance" nurses who could do it all--take care of medical and surgical patients, help out in the emergency department, and assist with obstetric cases--and do it well. Seeing Florence recently made me recall an incident that happened 18 years ago. The telephone rang at approximately 1 a.m. on a Saturday. An elderly patient with chest pain needed to be admitted to the hospital. My wife was out-of-town for the weekend. It was just me and my four-year-old son at home. I bundled him up, secured him in his car seat, and headed to the hospital. I walked into the small intensive care unit (ICU) holding the dozing child. Three of the four rooms were unoccupied. Florence immediately intercepted me. "You look at your patient," she directed me, "and I'll look after your son." She carefully removed his coat, placed him in an empty ICU bed, and covered him with a blanket. When I left the hospital more than two hours later, I realized that my son had slept through all the commotion. We were never billed for his "ICU admission." Nurses do a wonderful job of taking care of patients. There are occasions when they look after doctors and their families in special ways too. Practicing medicine in a small town has its perks.
Dr. Tony Miksanek has been a family physician for more than 20 years. Most of that time has been in solo private practice in Benton, a town of about 7,000 people in rural southern Illinois.
Address correspondence to Tony Miksanek, M.D., 712 Old Orchard Dr., Benton, IL 62812.
In order to preserve patient confidentiality, the patients' names and identifying characteristics have been changed in each scenario.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group