Abstract
Many medications have been reported to induce acneiform eruptions. A relatively new chemotherapy drug, gefitinib (Iressa), approved by the Food and Drug Administration in 2003 for the treatment of advanced-stage non-small cell lung cancer (NSCLC), has been reported to cause acne or an acne-like eruption. We report an Asian female who presented with hundreds of erythematous papules and pustules on her face, chest, and back, all of which appeared after starting gefitinib to treat non-small cell lung cancer.
**********
Introduction
The oral drug gefitinib is one of the many new anti-euplastic drugs that block epidermal growth factor receptor (EGFR) tyrosine kinases and prevents epidermal growth factor-induced proliferation in cell culture. It inhibits growth and causes regressions in human tumor xenografts with EGFR overexpression (1). Phase I trials identified diarrhea as dose-limiting at daily oral gefitinib doses of 700-1000 mg (2-5). An acne-like rash was also noted. Unlike conventional chemotherapy, gefitinib did not cause myelosuppression, neuropathy, or significant alopecia. In the same phase I trials, there was a rapid improvement and radiologic regressions were noted in patients with NSCLC who had previously received chemotherapy. In a randomized, double blind, phase II trial, subjects were divided into two groups; one group taking 250 mg and the other group taking 500 mg doses of gefitinib to determine whether there were important differences in the outcomes or adverse effects. The patients included in the study had stage IIIB or stage IV NSCLC and had progressed after at least two prior chemotherapy regimens including a platinum drug and docetaxel. Gefitinib is indicated as a monotherapy for the treatment of patients with advanced or metastatic non-small cell lung cancer after failure with both platinum-based and docetaxel chemotherapies.
Case Report
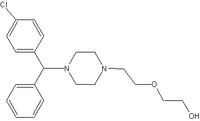
A 40-year-old Asian female presented with a history of non-small cell lung cancer with metastases involving T12 and a paraspinal mass. She began radiotherapy on February 2003 to T11, T12, and L1 and started on gefitinib 250mg qd in August 2003. She presented to the Dermatology Department at Texas Tech Health Science Center the following month with a sudden onset of a "rash" located on her face, back and chest. She had been treated initially with topical clindamycin and a topical steroid cream to her face without improvement. She denied any history of prior oral steroid usage. On physical examination, she had hundreds of erythematous papules and pustules across her face, chest, and back (Figure 1 and 2). She was started on Minocycline 100 mg twice daily, topical Klaron twice daily, and Atarax 25 mg once daily for itching. After consultation with her oncologist, the gefitinib was stopped for 2 weeks to monitor improvement. She did experience some improvement with discontinuation of the gefitinib but a mild acneiform eruption persisted. She is currently maintained with gefitinib 250mg qd. Oral and topical acne therapies have not provided any additional improvement and have been discontinued. Prior reports of patients with severe skin adverse drug reactions were success-fully managed by providing a brief (up to 14 days) therapy interruption followed by reinstatement of the 250 mg daily dose.
[FIGURE 1 OMITTED]
[FIGURE 2 OMITTED]
Discussion
While there is a great deal of information in the literature about gefitinib, there is little information about acne induced by gefitinib; however, in a multi-center clinical trial of 216 individuals there is evidence to support that acne can be a side effect of Iressa (6). The most common adverse effects reported at the recommended 250 mg dose were diarrhea, rash, acne, dry skin, nausea, and vomiting. In the multi-center clinically phase II trial, of the 102 individuals taking 250 mg/day, 25 individuals reported having acne and the 114 individuals taking 500 mg/day, 37 individuals reported having acne. In addition, those taking 250 mg/day, 44 individuals reported having a rash and 13 reported having dry skin, and those taking 500 mg/day, 61 individuals reported having a rash and 30 reported having dry skin. It is clearly evident that Iressa does affect the skin by causing acne, as well as other skin reactions, such as a skin rash or dry skin. The skin rash was not further described.
While gefitinib is approved for NSCLC, it has been tested for use in other forms of cancer, including metastatic colorectal cancer (7). That study also reported an acne-like skin rash. It was described as a sterile, suppurative eruption, starting on the face, scalp, chest, and upper back, and resolved without scarring, once the treatment was stopped. Interestingly, their studies indicated that the more severe acne-like eruptions were associated with higher treatment responses in patients with refractory colorectal cancer. Anecdotal evidence supports a similar finding of NSCLC remission with acne eruptions. Those patients whose NSCLS did not respond to gefitinib also did not develop acne.
Trojan et al reported a case of necrolytic migratory erythema-like eruption in a patient taking gefitinib for NSCLC with cerebral metastases (8). She took the drug for six weeks before the development of the necrolytic migratory erythema-like eruption. No evidence of an underlying glucagonoma could be found. Immunohistochemical studies demonstrated strong expression of epidermal growth factor tyrosinase inhibitor in the epidermal layer. Morphically, there were no changes in the sebaceous or eccrine glands.
The mechanism of gefitinib inducing acne or acne-like lesions is not known. However, epidermal growth factor, which is made by the monocytes, macrophages, and fibroblasts, is essential for normal skin development. The absence of epidermal growth factor receptors impairs epithelial development, including the skin (9). With the development of gefitinib and other chemotherapeutic agents in the EGFR class, clinicians need to be aware of the development of an acne or acne-like eruption. Prompt diagnosis and treatment of this side effect may allow the patient to continue with the drug if it is achieving its desired therapeutic effect.
References
1. Albanell J, et al. Pharmocodynamic studies of the epidermal growth factor receptor inhibitor ZD 1839 in skin from cancer patients: histopathologic and molecular consequences of receptor inhibition. J Clin Oncol 2001; 20:110-24.
2. Ranson M, et al. ZD 1839 a selective oral epidermal growth factor receptor-tyrosine kinase inhibitor, is well tolerated and active in patients with solid, malignant tumors: results of a phase I trial. J Clin Oncol 2002; 20:2240-50.
3. Herbst RS, et al. Selective oral epidermal growth factor receptor tyrosine kinase inhibitor ZD 1839 is generally well tolerated and has activity in non-small-cell lung cancer and other solid tumors: results of a phase I trial. J Clin Oncol 2002; 20:3815-25.
4. Baselga J, et al. Phase I safety, pharmacokinetic and pharmacodynamic trial of ZD 1839, a selective oral epidermal growth factor receptor tyrosine kinase inhibitor, in patients with five selected solid tumor types. J Clin Oncol 2002; 20: 4292-302.
5. Kusaba H, et al. A phase I intermittent dose-escalation trial of ZD1839 (Iressa) in Japanese patients with solid malignant tumors. Clin Cancer Res 2000; 6: 4543S.
6. Kris M, et al. Efficacy of Gefitinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in symptomatic patients with non-small cell lung cancer: a randomized trial. JAMA 2003; 290(16):2149-58.
7. H. Lee Moffitt Cancer Center and Research Institute. Inc Cancer Control 2003; 10(3):224-38.
8. Trojan A, et al. Necrolytic migratory erythema (Glucagonoma-like skin lesions induced by EGF-receptor inhibition. Swiss Med Wkly 2003; 133:22.
9. Burkhart CN. Clinical assessment of acne pathogenesis with treatment implications. International Pediatrics 3003; 18(1).
MOLLY M WARTHAN BA, CYNTHIA A JUMPER MD, JENNIFER L SMITH MD
TEXAS TECH UNIVERSITY HEALTH SCIENCES CENTER
LUBBOCK, TEXAS
ADDRESS FOR CORRESPONDENCE:
Jennifer L Smith MD
Texas Tech University Health Sciences Center
4911 7th Street
Lubbock, TX 79424
Phone: (806) 743-1842
E-mail: jen.smith@ttuhsc.edu
COPYRIGHT 2004 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2005 Gale Group