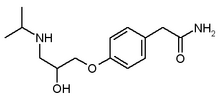
Atenolol
Atenolol is a drug belonging to the group of beta blockers, a class of drugs used primarily in cardiovascular diseases. Introduced in 1976, Atenolol was developed as a replacement for propanolol in the treatment of hypertension. Hypertension is a clinical condition in which the arterial blood pressure in rest exceeds constantly 140/90 mm Hg (as defined by the World Health Organization). Hypertension is a risk factor for stroke, myocardial infarction (heart attack), and serious renal damage. more...
Propranolol is known to readily cross the blood-brain barrier (BBB) and can pass into the brain, causing side-effects such as depression and nightmares; atenolol was specifically developed to be unable to pass through the blood-brain barrier in order to prevent this effect.
Pharmacology and Indications
Atenolol can be used to treat cardiovascular diseases such as hypertension, coronary heart disease, arrhythmias, and treatment of myocardial infarction after the acute event. Patients with compensated congestive heart failure may be treated with Atenolol as a comedication (usually together with an ACE inhibitor, a diuretic and a digitalis-glycosid, if indicated). In patients with congestive heart failure, it reduces the need for and the consumption of oxygen of the heart muscle. It is very important to start with low doses, as atenolol reduces also the muscular power of the heart, which is an undesired effect in congestive heart failure.
The drug is also used to treat other conditions, including dysautonomia, anxiety and hyperthyroidism (overfunction of the thyroid gland).
Due to its hydrophilic properties, the drug is less suitable in migraine prophylaxis compared to Propranolol, because for this indication, atenolol would have to reach the brain in high concentrations, which is not the case (see below).
Atenolol is a so-called beta1-selective (or 'cardioselective') drug. That means that it exerts greater blocking activity on myocardial beta1-receptors than on beta2 ones in the lung. The beta2 receptors are responsible to keep the bronichal system open. If these receptors are blocked, bronchospasm with serious lack of oxygen in the body can result. However, due to its cardioselective properties, the risk of bronchospastic reactions if using atenolol is reduced compared to nonselective drugs as propranolol. Nonetheless, this reaction may also be encountered with atenolol, particularly with high doses. Extreme caution should be exerted if Atenolol is given to asthma patients, who are particularly at risk; the dose should be as low as possible. If an asthma attack occurs, the inhalation of an beta2-mimetic antiasthmatic, such as hexoprenalin or salbutamol, will usually suppress the symptoms.
Provisonal data suggests that antihypertensive therapy with Atenolol provides weaker protective action against cardiovascular complications (e.g. myocardial infarction and stroke) compared to other antihypertensive drugs. In particular, diuretics are superior. Propranolol and metoprolol might also be better alternatives. However, controlled studies are lacking (CARLBERG, B. et al.: Lancet 2004; 364: 1684-9).
Unlike most other commonly-used beta blockers, atenolol is excreted almost exclusively by the kidneys. This makes it attractive for use in individuals with end-stage liver disease.
Read more at Wikipedia.org