Previous studies have reported conflicting reports concerning the effects of anticholinergic agents during the treatment of acute asthma attacks. Rebuck et al [1] showed that ipratropium bromide produced a significant increase in bronchodilation when given with fenoterol, a [beta]-adrenergic agent. Karpel and associates, [2] however, found that atropine sulfate, given as a nebulized solution, did not increase bronchodilation when given 80 minutes after treatment with inhaled metaproterenol. The latter study used a randomized crossover design, with patients initially treated with either metaproterenol or atropine sulfate alone and later with the other compound. The effects of giving atropine sulfate after metaproterenol were monitored for only 40 minutes. Since the peak effect of atropine sulfate on bronchodilation occurs approximately 60 minutes after administration, [3] it is possible that a beneficial effect might have been shown by following the patients for a longer observation period. The present study was designed to determine whether atropine sulfate increases bronchodilation when added to an inhaled [beta]-adrenergic agonist during the initial treatment (first 2 hours) of an acute asthma attack.
METHODS
Patients presenting to the LSU Hospital Emergency Department with acute exacerbations of asthma were studied. They were required to have a history of asthma as defined by the American Thoracic Society Committee on Standards for Diagnosis and Care of Patients with Chronic Obstructive Pulmonary Disease (COPD) and Asthma, [4] and to have an [FEV.sub.1] less than 2 L prior to beginning the study. Patients were excluded if they were older than 65 years of age or younger than 18 years of age, had ever smoked cigarettes, or had heart disease, glaucoma, bladder dysfunction, prostatism, chronic bronchitis, emphysema, or hypertension. Written informed consent was obtained from each patient; the consent form was approved by the Institutional Review Board for Human Studies.
Patients who met the admission criteria were randomized in a double-blinded fashion to receive either one dose of nebulized metaproterenol (5 percent solution, 0.3 ml) alone, or combined with atropine sulfate (2.5 mg) in 3 ml normal saline solution. All medications were administered in a hand-held nebulizer (Medi-Mist, Mountain Medical Equipment, Inc, Lindenhurst, NY) attached to an aerosol mask (Hudson Co, Temecula, CA). Nebulization was continued until the face mask was dry. To ensure double-blind treatment, packages were prepared in advance and coded. These were then selected randomly by the treating physician, but neither this physician nor the patient knew which medications were administered. Patients were dropped from the study if they required additional therapy during the 2-hour observation period.
Prior to beginning the study, venous blood was obtained from all patients taking theophylline to determine plasma theophylline levels. Spirometry was performed prior to nebulization of bronchodilators and again 30, 60, and 120 minutes after therapy. Spirograms were performed with a portable wedge bellows spirometer (Vitalograph, Inc, Lenexa, KS) that was calibrated daily using a test syringe. The subject's pulse rate, respiratory rate, blood pressure, and the presence of any side effects were recorded at each time interval.
Data were expressed both as the mean percent change in [FEV.sub.1] or FVC ([FEV.sub.1] or FVC [time]-[FEV.sub.1] or FVC [baseline] x 100/[FEV.sub.1] or FVC [baseline]) and as the actual mean change in milliliters for each treatment group. Results were compared using Student's t test for unpaired data. Differences were considered significant when p[is less than or equal to]0.05.
RESULTS
Forty patients satisfied all entry criteria and were
[TABULAR DATA OMITTED]
randomized to one of the two treatment groups. Three of these patients were withdrawn from the study during the 2-hour observation period because they were too ill and needed additional therapy. Only data from the 37 patients who completed the study are reported. The clinical characteristics of these patients are presented in Table 1. The group treated with metaproterenol alone (n=20) was similar to the group treated with the combination of metaproterenol and atropine sulfate (n=17) in regard to sex, age, duration of asthma, theophylline level, [FEV.sub.1], FVC, and [FEV.sub.1]/FVC at time zero. The mean age of the group receiving combination therapy was 8 years older, although this difference was not statistically significant (p=0.10).
The percent change in [FEV.sub.1] and FVC from baseline (percent [FEV.sub.1] and percent FVC) in the two groups is shown in Table 2. Both groups had a significant increase in [FEV.sub.1] and FVC at all times tested compared with their initial measurement. However, there was no statistically significant difference between the two groups at any time point. This was true whether results were expressed as the mean [FEV.sub.1] percent and FVC percent or the actual change in milliliters (Table 2).
Since it has been proposed [5] that older patients might have an element of chronic bronchitis and therefore might respond better to cholinergic agents, we determined whether age affected the response of patients to the addition of atropine sulfate. We divided
[TABULAR DATA OMITTED]
[TABULAR DATA OMITTED]
the patients receiving combination therapy into those younger than 40 years of age and those aged 40 years or older (Table 3). Patients aged 40 years or older did not respond to the addition of aropine sulfate any more than patients younger than 40 years. This was true for both [FEV.sub.1] and FVC at all time points during the 2-hour observation period.
There was no significant correlation between bronchodilatory response and the duration of asthma in patients receiving atropine sulfate. Additionally, the degree of ventilatory dysfunction ([FEV.sub.1]) prior to treatment did not correlate with bronchodilatory response in patients receiving atropine sulfate.
The number of patients with side effects (tremor, dry mouth, nausea, increase in heart rate > 10 beats) in both groups is shown in Table 4. Six patients had one side effect each; two patients in the metaproterenol group and four patients in the combination group. While the difference in the number of patients with side effects was not statistically significant, those receiving combination therapy tended to have more side effects (24 percent vs 10 percent, p=0.38).
The disposition of patients after 2 hours was not different in the two groups. The percent of patients discharged to home vs the percent admitted to the hospital or requiring continued emergency department treatment was similar (Table 5).
DISCUSSION
Our data show that nebulized atropine sulfate yields no additional bronchodilation during a 2-hour observation period when added initially to metaproterenol in patients with acute exacerbations of asthma. These
Table 4--Reported Side Effects During 120-Minute Observation Period
(*) M = metaproterenol sulfate; M + A = metaproterenol sulfate + atropine sulfate.
Table 5--Disposition 2 Hours after Bronchodilator Aerosol Treatment
(*) M = metaproterenol sulfate; M + A = metaproterenol sulfate + atropine sulfate.
results agree with those of Karpel and associates [2] who showed that 6.4 mg of atropine sulfate provided no clinically significant bronchodilation when given after therapeutic doses of metaproterenol aerosol. Karpel et al used a crossover study design, with half the patients receiving metaproterenol first and then atropine sulfate 80 minutes later. They followed [FEV.sub.1] after administration of atropine sulfate for only 40 minutes, and concluded that it did not augment the bronchodilatory effect of metaproterenol. Since the peak effect of atropine sulfate is approximately 60 minutes after inhalation, [3] it is possible that an additional bronchodilator effect might have occurred later. Our results, with a 120-minute observation period, provide additional evidence that atropine sulfate does not augment the bronchodilatory effects of a nebulized [beta]-adrenergic agonist in the early treatment of asthma attacks.
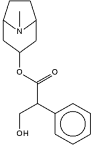
The dose of 2.5 mg used in the study is a conventional dose that is frequently recommended for emergency department use in adults. Doses greater than this may be associated with side effects such as slurred speech, difficulty with swallowing and micturation, and mental changes. [6] We did not choose a higher dose for this study because of these potential side effects, which would limit the clinical usefulness of atropine sulfate even if it were found to augment bronchodilation.
While atropine appears to be ineffective in most patients with asthma, it has been suggested that certain subsets of patients may be more responsive. Previous investigators have stated that anticholinergic agents are more effective in patients older than 40 years, those with a long history of asthma, and those with milder exacerbations of their obstructive airway disease. [5,7,8] Our results provide evidence that the response to atropine sulfate is not related to age, since patients older than 40 years did not show more bronchodilation than patients younger than 40 years. Additionally, when the response of the combination therapy group was looked at in reference to duration of asthma, there was no significant correlation between bronchodilatory response and duration of their disease.
Altounyan [8] has suggested that patients with more severe airways obstruction respond poorly to atropine sulfate. While the pretreatment [FEV.sub.1] was lower in the group that received combination therapy (0.98 L) compared with the group that received metaproterenol alone (1.26 L), this difference was not statistically significant (p=0.29). We found no correlation between the level of the initial [FEV.sub.1] and response (change in [FEV.sub.1] in milliliters or as a percent of baseline) to the addition of atropine sulfate. In other words, there was no improved bronchodilation in those with milder obstruction. It has been suggested that while atropine sulfate may not increase the overall degree of bronchodilation, it may prolong the bronchodilatory effect. [9] Our study did not determine responses beyond 120 minutes.
Several studies have shown that the quartenary ammonium derivative of atropine, ipratropium bromide, is effective in the treatment of acute asthmatic attacks. [10,11] Rebuck et al [1] demonstrated that it is additive to a [beta]-agonist in this setting, whereas in the treatment of an acute exacerbation of COPD, it is equally effective, but not additive. Atropine sulfate, on the other hand, has not been shown to have a beneficial role in the treatment of acute asthma in the present study or in previous studies, and has significantly more side effects. [2,12] While the two anticholinergic agents have similar mechanisms of action, ipratropium bromide may be more effective at recommended doses because of a slower local metabolism and less absorption, and thus a longer half-life in the airway. Furthermore, ipratropium bromide has few or no side effects, whereas the dose of atropine sulfate is limited by systemic side effects secondary to its rapid absorption. These are possible reasons for the conflicting reports regarding the beneficial effects of the two agents.
It is possible that because of the relatively small numbers of patients in our two treatment groups, we may have failed to detect small but distinct differences between bronchodilator effects in the two groups. However, the number of patients entered in this study is similar to that of previous studies that have addressed the use of atropine sulfate in the treatment of obstructive airways disease. [2,12] Because of the difficulty of enrolling patients into a highly regimented study protocol like this, we were unable to increase the study population further without a prolonged study period that might entail changes in personnel, equipment, etc.
The results of this study extend the findings of Karpel et al [2] and indicate that when the observation time is prolonged to 120 minutes to cover the period of peak effect of atropine sulfate, it has no significant additive effect when given with a nebulized [beta]-adrenergic agent to patients with acute asthma. We were unable to identify a subset of patients (older, longer duration of disease, or less severe obstruction) who received additional benefit from atropine sulfate. Based on our results, as well as those of other investigators, [2,12] there is no evidence that atropine sulfate is a useful adjunct in the initial treatment of acute asthma attacks in the emergency department.
REFERENCES
[1] Rebuck AS, Chapman KR, Abboud R, Pare PD, Kreisinan H, Wolkove N. et al. Nebulized anticholinergic and sympathomimetic treatment of asthma and chronic obstructive airways disease in the emergency room. Am J Med 1987; 82:59-64
[2] Karpel JP, Appel D, Breidbart D, Fusco MJ. A comparison of atropine sulfate and metaproterenol sulfate in the emergency treatment of asthma. Am Rev Respir Dis 1986; 133:727-29
[3] Cavanaugh MJ, Cooper DM. Inhaled atropine sulfate: dose response characteristics. Am Rev Respir Dis 1976; 114:517-24
[4] Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD) and asthma. Am Rev Respir Dis 1987; 136:225-44
[5] Ulah MI, Newman GB, Saunders KB. Influence of age on response to ipratropium and salbutamol in asthma. Thorax 1981; 36:523-29
[6] Weiner N. Atropine, scopalamine and related antimuscarinic drus. In: Gilman AG, Goodman LS, Gilman A, eds. The pharmacologic basis of therapeutics. 6th ed. New York: Macmillan; 1980:-135
[7] Partridge MR, Saunders KB. Site of action of ipratropium bromide and clinical and physiological determinants of response in patients with asthma. Thorax 1981; 36:530-33
[8] Altounyan REC. Variation of drug action on airways obstruction in man. Thorax 1964; 19:406-15
[9] Shenfield GM. Combination bronchodilator therapy. Drugs 1982; 24:414-39
[10] Ward MJ, Fentem PH, Smith WHR, Davies D. Ipratropium bromide in acute asthma. Br Med J 1981; 282:598-600
[11] Bryant DH. Nebulized ipratropium bromide in the treatment of acute asthma. Chest 1985; 88:24-8
[12] Karpel JP, Briedbart D, Appel D, Fusco MJ. A comparison of atropine sulfate and metaproterenol sulfate in the emergency treatment of asthma. Am Rev Respir Dir 1985; 131:A49
COPYRIGHT 1991 American College of Chest Physicians
COPYRIGHT 2004 Gale Group