Women's Health
Oxytrol
A transdermal oxybutymn, the FDA approved Oxytrol in February 2003, for control of urinary incontinence due to overactive bladder ( OAB ). Approval was based on clinical trials.1'2 Anticholinergic therapy has been the standard pharmacologie treatment, however these medications produce increased bladder capacity and a delayed desire to void. . Oral oxybutynin (Ditropan) has been the anticholinergic pharmacologie treatment of choice for OAB albeit not without significant side effects. The transdermal oxybutynin patch appears to be as effective with fewer side effects than the oral forms.
Oxybutynin chloride is a potent muscarinic receptor antagonist that acts predominantly in the parotid glands and bladder. The drug is a synthetic tertiary amine, well-absorbed through gastrointestinal processes and undergoes extensive first-pass liver metabolism.3 The drug exerts a spasmolytic action and antimuscarinic action on smooth muscle, although with little to no effect on blood vessel smooth muscle. Metabolism is predominantly in the liver and excretion is through the urine. Oxybutynin is classified as a pregnancy class B medication and it is unknown if the drug is distributed into human milk.
Patients in over 50 United States centers were involved in these two clinical trials to compare the efficacy and side effects of oral versus transdermal oxybutynin.1,2 Results indicated a significant and similar reduction of daily incontinence episodes with both oral and transdermal groups. Dry mouth, the most commonly reported side effect, was less severe and occurred in significantly fewer patients in the transdermal group (38%) as compared to the oral group (94%). Erythema at the patch application site was assessed and reported to be mild (30%), moderate (7%), and severe (1%) by those receiving transdermal treatment.
Although efficacy is comparable, the transdermal patch has reduced undesirable side effects and minimal adverse reactions, suggesting an overall favorable profile for prescribing transdermal oxybutynin. Medication compliance may improve with use of the transdermal route as the twice-weekly dosing reduces the need for the daily administration of the oral form.
Oxytrol, produced by Watson Pharmaceuticals, Inc., is a thin, flexible, clear patch that delivers 3.9 milligrams per day of oxybutynin when applied to the abdomen, hip, or buttock twice a week. The patch adheres well with minimal skin irritation. Each patch provides symptom relief for up to four days. Patients with a history of urinary retention, gastric retention, and uncontrolled narrow-angle glaucoma should avoid the use of this medication.
Nonpharmacologic interventions should also be encouraged. Bladder training and pelvic muscle rehabilitation to relieve urinary incontinence are noninvasive techniques with proven efficacy and minimal risk.
Valtrex
The FDA revised the labeling for valacyclovir (Valtrex) to include its use in the reduction of risk of heterosexual transmission of genital herpes to susceptible partners. This decision was based on international, double-blind, placebocontrolled research among 1,500 monogamous, heterosexual couples over an 8-month period conducted by GlaxoSmithKline (GSK).4 This study showed reductions of 75% symptomatic HSV-2 acquisition, 50% HSV-2 seroconversion, and 48% overall HSV-2 acquisition.5
Valacyclovir hydrochloride is rapidly absorbed from the gastrointestinal tract, converted to acyclovir, then encoded by herpes simplex virus (HSV) and varicella-zoster virus (VZV) into a nucleotide analogue.5 This means the inhibitory activity of the medication is highly selective to HSV and VZV; however, it is not a cure for genital herpes. Patients must continue to avoid contact with lesions and be aware that herpes can be transmitted in the absence of symptoms through asymptomatic viral shed. all patients need to be aware of the necessity for safe sex practices in combination with the suppressive therapy.
The plasma elimination half-life averaged 2.5 to 3.3 hours and renal clearance is increased with impaired renal function. Dose reduction may be required for clients with decreased renal function.
Oral valacyclovir hydrochloride is indicated for the treatment of herpes zoster (1 gram TID × 7 days), genital herpes (1 gram BID × 10 days), recurrent episodes (500 mg BID × 3 days), and herpes labialis (2 grams BID × 1 day).5Sunscreen is also effective in reducing ultraviolet light exposure as a trigger for cold sores. all therapy should begin at the first sign or symptom of an episode. Valacyclovir hydrochloride is also indicated for suppressive therapy in immunocompetent individuals with genital herpes.5 No data are available for safety and efficacy of therapy with Valtrex beyond 1 year. Suppressive therapy for IIIV-infected patients with CD4 cell count greater than or equal to 100 cells/mm3 is 500 mg daily.
A serious adverse event of thrombotic thrombocytopenic purpura/hemolytic uremie syndrome has occurred in patients with advanced HIV disease, in allogeneic bone marrow transplant and renal transplant recipients in clinical trials of Valtrex at doses of 8 grams per day.3 Additional adverse effects include nausea, headache, vomiting, dizziness, abdominal pain, dysmenorrhea, arthralgias, and depression.
Research has not yet addressed the use of Valtrex in pregnant women, nursing mothers, or pediatrie use. Patient information sheets are available from GiaxoSmithKline. The cost for thirty 500 mg tablets is approximately $170.6
Femring
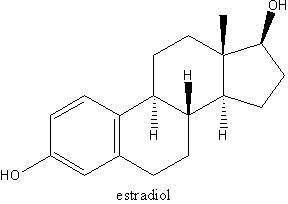
The PDA approved a vaginal ring for hormone therapy in March 2003. The estradiol acetate vaginal ring (Femring), manufactured by Galen Hodings, was approved to treat hot flashes and vaginal symptoms of menopause. It is a flexible ring a woman inserts herself. Side effects, precautions and warnings are similar to other topical, vaginal estrogen products. The ring does not include progestin and therefore standard protocols for women with intact uterus on estrogen should be followed.7
Men's Health
Uroxatral
Alfuzosin (Uroxatral) extended-release tablets were approved by the PDA in june 2003 for the treatment of benign prostatic hypertrophy (BPH). This medication is an alphaj-adrenergic antagonist exerting its effects on the prostate, bladder neck, and posterior urethra. Smooth muscle blockade in these structures improve urine flow and BPH symptom reduction. The extended-release 10 mg tablets are taken each day immediately after the same meal.
Adverse events associated with alfuzosin are related to its cardiovascular effects. Dizziness, headache, and fatigue are the most common. Alfuzosin is hepatically metabolized and other drugs (e.g., ketoconazole, itraconazole, and ritonavir) using the CYP3A4 enzyme systerns may increase the bioavailability of alfuzosin. Co-administration of vardenafil (Levitra) or sildenafil (Viagra) may cause symptomatic hypotension.
Patients taking CYP3A4 inhibitors or with moderate to severe liver dysfunction are contraindicated from using alfuzosin. Alpha^sub 1^-blockers are antihypertensive agents and patients using alfusozin should be cautioned about this potential effect; especially if using other blood pressure lowering medications. The appearance of or increase in angina symptoms require discontinuation of alfuzosin. Alfuzosin should be cautiously used in patients who have a history of QT interval prolongation or are taking medications with this effect. Prescribers are also advised to carefully consider the use of this medication in patients with severe renal insufficiency.
Alfuzosin has been available in countries outside the United States for many years. One double-blind, placebo controlled study demonstrated effective relief from BPH symptoms at a dose of 10 mg.8 Other alphat adrenergic antagonists have a similar dose-related side-effect profile, and seem to have comparable efficacy.9 No comparative studies of these medications has been conducted.
Alfusozin (UroXatral), manufactured by Sanofi-Synthelabo, is considered an effective medication in the treatment of patients with moderate to severe BPH symptoms.
Levitra
Vardenafil (Levitra) was approved by the PDA in August 2003 to treat erectile dysfunction.10 Penile erection occurs with increased blood flow to the corpus cavernosum. This process involves sexual stimulation that initiates nerve endings and endothelial cells to release nitric oxide. Nitric oxide stimulates increased synthesis of cyclic guanosine monophosphate (cGMP). It is the cGMP that stimulates smooth muscle relaxation allowing increased blood flow into the penis and resulting in erection. Cyclic GMP is degraded via phosphodiesterases (PDEs). Inhibition of PDE5, the most abundant PDE in the corpus cavenosum, slows down the rate of degradation of cGMP. The increased amount of available cGMP provides enhanced erectile function.11 The medication has no effect if nitric oxide is not released due to sexual stimulation.
Vardenafil is eliminated by hepatic metabolism (mainly CYP3 A4 and CYP2C) and use with strong CYP3A4 inhibitors (ritonavir, indinavir, ketoconzaole) and even mild CYP3A4 inhibitors (erythromycin) may result in significant increases of plasma levels of vardenafil. The half-life of the drug is about 4 to 5 hours and it is excreted primarily in the feces.11
Vardenafil is absorbed rapidly after oral dosing in a fasting state, is highly bound to plasma proteins, and has an extensive tissue distribution. Maximum plasma concentrations after a single 20 mg dose are reached between 30 minutes and 2 hours with a median of 60 minutes. High-fat meals cause an 18% to 50% reduction in maximum concentration."
When combined with nitrates, it may cause an additional time-related decrease in blood pressure and increase in heart rate. The use of vardenafil is contraindicated for patients on nitrate therapy, on nitric oxide donors, using "poppers" such as amyulnitrate or butylnitrate and/or on alpha-blockers.12 Concurrent use increases the risk of hypotension that could result in dizziness, syncope, myocardial infarction (MI) or cerebral vascular accident (CVA). Clients currently taking quinidine, procainamide, amiodarone, sotalol, ritonavir, indinavir sulfate, ketoconazole, itraconazole, erythromcycin, or other treatments for erectile dysfunction should be carefully evaluated for dose and use of Levitra. A time interval for multiple doses has not been determined.11
Clients with left ventricular outflow obstruction may be sensitive to the action of vasodilators. Client history gathered prior to prescribing vardenafil should include history of heart problems, low blood pressure, CVA, family members with a prolonged QT interval, liver problems, kidney problems, retinitis pigmentosa, stomach ulcers, bleeding problems, deformed penis shape (Peyronie's disease), history of an erection that lasted more than 4 hours, sickle cell anemia, multiple myeloma, or leukemia.11
Sustained erections and priapism (painful erection greater than 6 hours) have rarely occurred but, because of the serious consequences of untreated priapism, clients should be aware of the possibility and cautioned to seek immediate medical care if they experience priapism. They should also be aware that Levitra does not increase sexual desire, function as birth control, or protect the man or his partner from sexually transmitted diseases. It is recommended clients with moderate hepatic impairment begin with 5 mg and not exceed a dose of 10 mg. Elderly males (> or =65 years) showed a higher plasma concentration than younger males and clinicians should consider a starting dose of 5 mg for their older patients.11
Additional adverse reactions included reports of headache (15%), flushing (11%), rhinitis (9%), dsyspepsia (4%), sinusitis (3%), flu syndrome (3%), dizziness (2%), increased creatine kinase (2%), and nausea (2%)."
The recommended starting dose is 10 mg orally about 60 minutes before sexual activity and may be increased to a maximum dose of 20 mg or decreased to 5 mg. Levitra should not be taken more than once a day and starting doses should be reduced to 5 mg for clients over 65 and/or those with moderate hepatic impairment.
* Immunologic
FluMist
Influenza Virus Vaccine Live, Intranasal (FluMist) is the first live virus vaccine and the first influenza vaccine that is administered nasally. The PDA approved the use of this new medication in june 2003. FluMist is a live trivalent vaccine intended for active immunization for the prevention of influenza. The vaccine viruses replicate in the nasopharynx but are attenuated so as not to cause an influenza-like illness. The Type A and B strains in FluMist are antigenically representative of influenza viruses that may circulate in humans during the 2003-2004 influenza season according to the United States Public Health Service. The vaccine is for use in children and adolescents (5 to 17 years) and adults (18 to 49 years), and is especially suited for patients reluctant or unwilling to get an IM vaccine injection. FluMist is manufactured by Medlmmune, Inc.
The mechanism of action for FluMist is to induce influenza serum antibodies to the strains selected each year. Clinical studies with this product evaluated 20,228 subjects including more than 10,000 children and adolescents. Multi-center, randomized, double-blind, placebo-controlled studies were reviewed. In children, the nasal vaccine was effective in preventing influenza in approximately 85% of the clinical subjects.13 The results were less dramatic in adults, with small, but significant reductions noted in febrile illnesses and upper respiratory illnesses.14
FluMist should not be administered to immunocompromised or immunosuppressed patients, patients with a history of asthma, children under 5 years, and adults over 65 years. Patients with severe medical conditions that may predispose them to influenza should not receive FluMist. The production of the vaccine utilizes chicken eggs, so patients with a history of allergic reaction to eggs should avoid this medication.
Adverse events for FluMist are mild and typically include nasal congestion, runny nose, sore throat, and cough. The medication is listed as a Pregnancy Category C and it is unknown if the live vaccine is excreted in human milk. However, due to the close proximity of nursing mothers to their breast-feeding infants, caution is advised when considering using this vaccine in nursing mothers. Children or adolescents on aspirin therapy are contraindicated from receiving FluMist. Patients on antivirals should wait 48 hours after last dose before using FluMist.
FluMist comes in a single dose, single use sprayer that needs to be kept frozen and then thawed within 24 hours prior to use. Half the dose is sprayed into each nostril. Children 5 to 8 years old that have not previously been vaccinated with a live influenza vaccine should receive two doses approximately 60 days apart. Previously vaccinated children or patients 9 to 49 years should receive one dose. The vaccination should occur in the fall before the expected influenza season.
* Asthma Update
Xolair
The FDA approved a new biologic in june 2003 for allergyrelated asthma called omalizumab (Xolair).15 Xolair is a recombinant DNA monoclonal antibody and is designed to selectively bind to human immunoglobulin E (IgE). Bound IgE decreases the surface-bound IgE on mast cells and basophils and therefore somewhat limits degranulation of the mast cells when they are exposed to their antigens. This decrease in release of mediators reduces the severity and frequency of asthma symptoms, but like all nonselective biologic medications, side effects can be problematic.
The effectiveness of Xolair was assessed in two placebo-controlled studies that lasted only 6 months but did include over 1,000 adolescents and adults.15 With Xolair, 80% to 85% of the clients had no exacerbations of their asthma compared to about 70% to 75% of placebo-treated patients. However, treated clients had a 0.5% increase of new or recurrent cancer compared to a 0.2% increase in the control group. Additional studies are being conducted to determine if this is a true relationship or an aberrant finding.15
Another major concern is the potential for severe allergic reactions including anaphylaxis associated with this recombinant DNA monoclonal antibody. During the clinical trials, anaphylaxis occurred in three patients. all three patients recovered from the episode.
Only IgE mediated asthma events are affected by Xolair. It is not a rescue medication nor is it considered a first line therapy. It should be used only with clients that are not controlled with inhaled steroids and have documented allergenassociated symptoms.15,16 Prior to initiated therapy with Xolair, clinicians should follow the guidelines set in 1997 by the National Institutes of Health's National Heart, Lung and Blood Institute in their published Guidelines for the Diagnosis and Management of Asthma. This document cautions clinicians to initially rule out nonallergic symptoms that present as allergy such as rhinitis, sinusitis, and gastrointestinal reflux, and treat these conditions as indicated. In addition, these guidelines specifically state that clinicians treating clients with persistent asthma on daily medications should identify allergen exposures, use the patient's history to assess sensitivity to seasonal allergens, use skin testing or in vitro testing to assess sensitivity to perennial indoor allergens, and assess the significance of positive tests in the context of the patient's medical history.16
Xolair is manufactured by Genentech. The dose is 150 to 375 mg given as a subcutaneous injection every 2 to 4 weeks. Doses and dosing frequency are based on serum total IgE level measured before the start of treatment, and on body weight. Dose determination charts are available at the Genentech Web site.
Mean serum free IgE decrease was greater than 96% using recommended doses. The drug's half-life averaged 26 days. Since current analyses were limited to 12 to 76 years, Xolair is currently only indicated for adults and adolescents 12 years of age or above.17
It is recommended that oral corticosteroid reduction be continued initially and decreased only under direct clinician supervision. Clients placed on Xolair should be told not to decrease their inhaled steroid dose or stop taking any other asthma medications unless instructed to do so by their health care provider. They should also understand that this is not a rescue medication, and they may not see immediate improvement in their asthma after beginning Xolair therapy.
No formal drug interaction studies have been performed. Malignancies and anaphylaxis are the most serious adverse reactions and are currently under additional study. Other reactions reported include injection site reactions (45%), viral infections (23%), upper respiratory tract infection (20%), sinusitis (16%), headache (15%) and pharyngitis (11%)."
* Dermatology
Raptiva
Treatment regimens for psoriasis have had limited options, especially due to the compliance and safety concerns of chronic treatment using traditional therapies. However, in October 2003, the PDA approved efalizumab (Raptiva); the first biologic therapy that is designed for continuous control of chronic moderate to severe plaque psoriasis.
Psoriasis, a chronic condition that affects approximately 4.5 million people in the United States is due to rapid skin cell growth that produces thick, red, scaly, inflamed patches on the skin surface. The most common form of this incurable disease is plaque psoriasis, which presents with the typical plaque lesions topped with silvery white scales. Scalp, knees, elbows, and trunk are the most common sites. The disease is noncontagious.
Raptiva is a humanized monoclonal antibody that acts as an immunosuppressant by modulating targeted T cell activity. The mechanism of action of Raptiva decreases the lymphocytic activation involved in plaque psoriasis. This mechanism of action inhibits T-cell activation, T-cell trafficking to the dermis and epidermis, and T-cell reactivation. However, this action is not specific to the skin lesions and the medication has a potential to reactivate latent, chronic infections, or increase the risk of new infections.
Four randomized, double-blind, placebo-controlled phase III studies demonstrated patients (n=2,762) treated with Raptiva had at least a 75% reduction in the extent and severity of the psoriasis after 12 weeks.18 Continuing treatment with an every-other-week dosing schedule maintained the improvements in psoriasis symptoms. Raptiva is also reversible, with a return of psoriasis in 60 to 80 days after discontinuation of treatment.
Common adverse events in the study subjects included nonspecific infection (e.g. common cold), psoriasis, headache, pain, rhinitis, pharyngitis, and cough.18 Serious adverse events during the clinical studies included serious infections, malignancy, and thrombocytopenia although these were not significantly greater than in the placebo group.19 It is recommended that patients have a baseline and every 1 to 3 month platelet count to monitor for thrombocytopenia.
The safety and efficacy of concurrent Raptiva and other immunosupressants and immunizations has not been studied, nor has Raptiva had formal drug interaction studies.20 Raptiva is a Pregnancy Category C; it is unknown whether it is excreted in human milk, and it has not been studied or approved for use in pediatrie patients. Eight percent of the clinical trial patients were > or = 65 years and no significant differences in efficacy or safety were noted.20
The initial dose of Raptiva is 0.7 mg/kg, followed by weekly doses of 1 mg/kg (maximum dose not to exceed 200 mg). The subcutaneous injections are administered in the thigh, abdomen, buttocks, or upper arm, and injection sites should be rotated. Initial trials lasted 12 weeks, but ongoing clinical trials are assessing the continuous use of Raptiva therapy. Investigators are also evaluating the efficacy of evcry-otlicr-week dosing. Rapliva offers the convenience of self-administered injections, the rapid onset of clinical benefits, and a favorable impact on disease severity and patient outcomes.18 For people with moderate to severe psoriasis, this medication offers practitioners an important addition to the pharmacological management of these patients.
Cubicin
Daptomycin (Cubicin) for injection was approved for the treatment of complicated skin and skin structure infections in September 2003.21 As a new class of antibiotic called cyclic lipopeptide antibacterial agents, daptomycin offers a unique mechanism of action for treating serious infections including major abscesses, post-surgical skin wound infections, and infected ulcers. It is most effective against susceptible strains of gram-positive microorganisms including Staphylococcus aureus (including methicillin-resistant strains), Streptococcus pyogenes, Streptococcus agalactiae, Streptococcus dysgalactiae subspecies equisimilis and Enterococcus faecalis (vancomycin-susceptible strains only). It is not indicated for the treatment of pneumonia.21 Combination therapy may be needed if pathogens include gram-negative or anaerobic organisms.22
Clinical studies involving over 1,400 adults demonstrated efficacy and safety in treating complicated skin and skin structure infections when compared to equivalent standard treatments such as vancomycin or semisynthetic penicillin.21
Mild to moderate common adverse events were reported including gastrointestinal disorders, injection site reactions, fever, headache, insomnia, dizziness, and rash. Muscle injury was found rarely and most of these patients had no symptoms with normal blood tests after therapy. However, it is recommended that creatine phosphokinase (CPK) levels be monitored weekly in patients who receive Cubicin and more frequently in those who develop unexplained CPK elevations.21 all patients receiving Cubicin should be monitored for the development of muscle pain or weakness; especially weakness in the distal extremities.
Drug warnings listed in the package insert include danger of Pseudomembranous colitis. As with other antibacterial agents, overgrowth of G difficile may occur with altered normal flora of the gastrointestinal track. Therefore, it is important to consider this diagnosis in clients with diarrhea subsequent to the administration of any antibacterial agent including Cubicin.
Drug interactions were explored with warfarin and no significant effect on either drug was found. Studies of interaction of Cubicin with HMG-COA Reductase Inhibitors (statins) showed no reported skeletal myopathy in a placebocontrolled phase 1 trial but the study was limited (10 subjects). Consider temporarily suspending use of any statin in patients receiving Cubicin.22
Safety in pediatrie use, nursing mothers, and pregnancy has not been established. For clients over 65, lower clinical success rates were seen but with more adverse events.
Cubicin (4 mg/kg) is administered over a 30 minute period by intravenous infusion in 0.9% sodium chloride injection once every 24 hours for 7 to 14 days. It is primarily eliminated by the kidney and therefore, dosage modification is recommended for clients with creatinine clearance
Cardiovascular:
Crestor
Rosuvastatin (Crestor) is the newest HMG-CoA reductase inhibitor (statin) approved by the FDA in August 2003 for the treatment of hypercholesterolemia. Initially developed in Japan, it is licensed to AstraZeneca (United Kingdom) and initial evaluations seem to indicate this new statin exhibits many desirable characteristics and superior efficacy compared to other agents in the category.23'24 Data from many clinical trials have established the effectiveness of statins in the primary and secondary treatment of coronary heart disease.
Rosuvastatin's mechanism of action is similar to other statins and is a competitive inhibitor of HMG-CoA reductase, the enzyme involved in the synthesis of cholesterol in the liver. These agents reduce low-density lipoproteins (LDL) and triglycerides, and increase high-density lipoproteins (HDL). In numerous clinical studies, Crestor demonstrated superior cholesterol reduction when compared to placebo and other statins. Crestor had a dose-dependent reduction in LDL between 34% and 65% and a mean HDL increase between 7.7% and 9.6%.23 Investigators suggest that "rosuvastatin can achieve most of these lipid-modifying benefits at a dose of 10 mg/day".25
Crestor is available in 5-, 10-, 20-, and 40-mg tablets. Most patients achieved their cholesterol goals using a daily dose of 10 mg. The 20 mg is started on patients with very high cholesterol levels and the 40 mg dose is reserved for those inadequately treated with the 20 mg dose. In clinical trials, the 80 mg dose was found to increase the risk of renal impairment and rhabdomyolosis and was discontinued. The lower doses did not exhibit the adverse effect of rhabdomyolosis, however significant proteinuria was noted in patients using the 40 mg dose. Rosuvastatin does not appear to be metabolized by the cytochrome P450 3A4 enzymes, so the potential for interactions with other drugs using this enzyme are reduced in comparison with other statins.23 Crestor's long half-life of about 20 hours allow for a versatile dosing schedule. Additionally, the medication may be taken with or without food.
Adverse events that were reported in clinical trials with rosuvastatin included muscle aches, stomach pain, constipation, nausea, and weakness. Baseline liver function tests (LFT) should be acquired before initiating treatment with rosuvastatin, and repeated at 12 weeks or with any increase in dose. Periodic LFT monitoring is recommended for patients on long-term therapy. Crestor is a Pregnancy Category X and is therefore contraindicated in pregnant women. Geriatric populations did not exhibit any significant differences in adverse effects as compared to younger clinical study participants.
Stalins represent a significant agent in the practitioner's armamentarium for cholesterol control and treatment of heart disease. Crestor appears to offer some significant advantages over the other statins. In addition, the practitioner should encourage risk reduction in patients with coronary heart disease through lifestyle changes related to diet and exercise.
Coreg
Carvedilol (Coreg), a nonselective beta-adrenergic blocking agent with alpha!-blocking activity, was approved for treatment of severe heart failure in 2001. In March 2003, it received FDA approval for reducing the risk of death among heart attack patients with impaired cardiac function.26
Coreg efficacy was studied in a major trial designed to address the role of beta-blocking agents in patients post MI that were treated with recommended protocols including ACE inhibitors, thrombolytics, statins, and aspirin. all study participants had depressed left ventricular dysfunction after their myocardial infarction. The placebo-controlled, randomized trial enrolled more than 1,900 patients at over 160 sites in 17 countries. Treatment with Coreg reduced the risk of death for any reason by 23% (p=0.031).26 "Coreg had a consistent and beneficial effect on all-cause mortality as well as the combined end points of all-cause mortality plus hospitalization (total, CV, or for heart failure) in the overall study population and in all subgroups examined, including men and women, elderly and nonelderly, blacks, and nonblacks, and diabetics and nondiabetics."27
Coreg contains 3.125 mg, 6.25 mg, 12.5 mg or 25 mg of carvedilol and costs about $122 for 100 tablets.28 It is rapidly and extensively absorbed with a bioavailability of about 25% to 35% due to significant first-pass metabolism and the half-life ranges from 7 to 10 hours. Plasma concentrations are proportional to the oral dose administered. The rate of absorption is slowed when given with food with no real difference in bioavailability. This is significant because it means that taking Coreg with food is as effective and should minimize the risk of orthostatic hypotension.27
Coreg is extensively metabolized primarily by CYP450 enzymes so it may be affected by induction or inhibition of CYP450 enzymes. In fact, Rifampin decreased the concentration by about 70% and cimetidine increased the steady state AUC by 30% with no change in the concentration. Glyburide did not result in clinically relevant interaction for either compound. A single dose of hydrochlorothiazide also showed no effect on the pharmacokinetics of carvedilol. Digoxin (0.25 mg daily) given with 25 mg carvedilol for 14 days did increase steady-state concentrations of digoxin by 14% in twelve hypertensive patients. Torsemide and warfarin did not change pharmacokinetics when given with carvedilol.27 see package insert for additional drug interactions.
Coreg is 98% bound to plasma proteins independent of concentration over the therapeutic range. It is a basic, lipophilic compound with a substantial distribution into extravascular tissues. Plasma concentrations of carvedilol averaged about 50% higher in elderly compared to young subjects. Clients with hepatic impairment or renal insufficiency showed increased plasma concentrations of carvedilol following single-dose therapy.
Coreg is indicated for the treatment of mild to severe heart failure of ischemie or cardiomyopathic origin usually with concurrent use of diuretics, ACE inhibitors and digitals, to increase survival and to reduce the risk of hospitalization.27 Coreg is also indicated to reduce cardiovascular mortality in clinically stable patients in the post-acute phase of myocardial infarction and that have a left ventricular ejection fraction (MI) of
Coreg should not be given with inotropic medications, or to clients with asthma or other beta agonist-dependent breathing pathologies. It is contraindicated for clients with bronchial asthma (or related bronchospastic conditions), second or third degree AV block, sick sinus syndrome or severe bradycardia without a permanent pacemaker in place, patients with cardiogenic shock, or who have decompensated heart failure requiring the use of intravenous inotropic therapy. It can aggravate or precipitate symptoms of arterial insufficiency in patients with peripheral vascular disease. It should be used with caution in clients who will receive anesthetic agents that depress myocardial function. It is not recommended for clients showing hepatic impairment.27
Beta-blockers may mask manifestations of hypoglycemia especially tachycardia. There is a risk with Coreg of worsening hyperglycemia in congestive heart failure patients. Glucose levels should be monitored and clients warned of potential adverse effects. Beta blockage may also mask clinical signs of hyperthyroidism and abrupt withdrawal may be followed by an exacerbation of symptoms or even precipitate thyroid storm.
Coreg can be given as a treatment days to weeks following a heart attack. Clients should understand, as with any beta-blocker, they must avoid stopping therapy abruptly. Dosage reduction occurs gradually over a 1 to 2-week period with careful monitoring of the patient outcomes. Severe exacerbations of angina and the occurrence of myocardial infarction and ventricular arrhythmias have been reported in angina patients following the abrupt discontinuation of therapy with beta-blockers.27
Other reported adverse affects included shortness of breath, bradycardia, weight gain, fatigue, dizziness, and faintness. Clients with a history of an anaphylactic reaction should also be made aware that while taking betablockers they may be more reactive to the allergen and may be unresponsive to the usual doses of epinephrine used to treat allergic reaction.
Corcg is manufactured by GlaxoSmithKline.
DISCLOSURE
The authors have disclosed that they have no significant relationships or financial interests in any commercial companies that pertain to this education activity.
CE Test
Drug Approval Highlights for 2003
Instructions:
* Read the article beginning on page 8.
* Take the test, recording your answers in the test answers section (Section B) of the CE enrollment form. Each question has only one correct answer.
* Complete registration information (Section A) and course evaluation (Section C).
* Mail completed test with registration fee to: Lippincott Williams &Wilkins, CE Dept., 16th Floor, 345 Hudson St., NewYork, NY 10014.
* Within 3 to 4 weeks after your CE enrollment form is received, you will be notified of your test results.
* If you pass, you will receive a certificate of earned contact hours and an answer key. If you fail, you have the option of taking the test again at no additional cost.
* A passing score for this test is 29 correct answers.
* Need CE STAT? Visit http://www.nursingcenter.com for immediate results, other CE activities, and your personalized CE planner tool.
* No Internet access? Call 1-800-933-6525, ext. 331 or ext. 332, for other rush service options.
* Questions? Contact Lippincott Williams &Wilkins: 212-886-1331 or 212-886-1332.
Registration Deadline: February 28, 2006
Provider Accreditation:
This Continuing Nursing Education (CNE) activity for 2.5 contact hours and 2.5 pharmacology contact hours is provided by Lippincott Williams & Wilkins, which is accredited as a provider of continuing education in nursing by the American Nurses Credentialing Center's Commission on Accreditation and by the American Association of Critical-Care Nurses (AACN 11696, CERP Category O).This activity is also provider approved by the California Board of Registered Nursing, Provider Number CEP 11749 for 2.5 contact hours and 2.5 pharmacology contact hours. LWW is also an approved provider of CNE in Alabama, Florida, and Iowa and holds the following provider numbers: AL #ABNP0114, FL #FBN2454, IA #75. all of its home study activities are classified forTexas nursing continuing education requirements asType I.
Your certificate is valid in all states. This means that your certificate of earned contact hours is valid no matter where you live.
Payment and Discounts:
* The registration fee for this test is $17.95.
* If you take two or more tests in any nursing journal published by LWW and send in your CE enrollment forms together, you may deduct $0.75 from the price of each test.
* We offer special discounts for as few as six tests and institutional bulk discounts for multiple tests. Call 1-800-933-6525, ext. 332, for more information.
REFERENCES
1. Davilla GW, Daugherty CA, Sanders SW: A short-term, multicenter, randomized double-blind dose titration study of the efficacy and anticholinergic side effects of transdermal compared to immedicate release oral oxybutynin treatment of patients with urge urinary incontinence. J Urol 2001:166:140-145.
2. Dmochowski RR, Davila GW, Zinner NR, et al: Efficacy and safety of transdcrmal oxybutynin in patients with urge and mixed urinary incontinence. J Urol2002;168(2):580-586.
3. Wein A J, Rovener E S: Pharmacologie management of urinary incontinence in women. Urol Clin North Am 2002; 29(3): 537-550.
4. PDA Talk Paper. FDA Updates Labeling of Valtrex, T03-64. August 29, 2003. Retrieved November 31, 2003 at http://www.iya.gov/bbs/topics/ANSWERS/ 2003?ANSO 1250.html.
5. GlaxoSmithKline. Prescribing information Valtrex {valacyclovir hydrochloride) 2003. Retrieved November 31, 2003 from http://us.gsk.com/products/ assets/us_valtrex.pdf.
6. Presecrition Drugs. Valtrex 2003. Retrieved November 31, 2003 from http://www.prescriptiondrugs.com/valtrex.htm.
7. WcbMD Medical News retrieved by Brunilda Nazario, MD on March 21, 2003 for WebMD. Available at http://my.webmd.com/content/article/62/ 71711.htm?lastselectedguid={5FE84E90-BC77-4056-A91C-9531713CA348.
8. Roehrborn CG. Alfuzosin: Overview of phannacokinetics, safety, and efficacy of a clinically uroselectivc alpha-blocker. Urology 2001;58(Suppl 6A); 55-64.
9. {Therapeutic Research Center, 2003) New Drug: Uroxatral (Alfuzosin). Detail-Document #190909 2003. Retrieved 11/10/2003 from www.prescribersletter.com.
10. FDA Talk Paper. FDA Approves New Drug for Treatment of Erectile Dysfunction 2003. Retrieved August 19,2003 from http://www.fda.gov/bbs/topics/ANSWERS/2003/ANS01249.html.
11. GlaxoSmithKline. Levitra Prescribing information 2003. Retrieved November 30, 2003 from www.levitra.com.
12. GlaxoSmithKline. Patient Information 2003. Retrieved November 30, 2003 from www.levitra.com.
13. Bclshc R, Mendleman PM, Treanor J, et al: The efficacy of live, attenuated, cold-adapted, trivalent, intranasal influenza vaccine in children. N Engl J Medl998;338:1405-1412.
14. Nichol K, Mendelman, PM, Mallon, KD, et al: (1999). Effectiveness of live, attenuated intranasal influenza virus vaccine in healthy, working adults. JAMA 1999; 282: 137-144.
15. FDA Talk Paper TO3-49. FDA approves first biologic for allergy-related asthma. june 20, 2003. Retrieved November 30, 2003 from http://www.fda. gov/bbs/topics/ ANSWERS/2003/ ANS01236.html.
16. StoloffS: Xolair Advisory Committee Meeting Comments. May 15, 2003 retrieved from http://www.fda.gov/ohrms/dockets/ac/03/briefing/ 3952OPH 1_ 02_Stoloff.pd.
17. Genentech. Prescriber Information: Xolair (omalizumab) 2003. Relieved November 31, 2003 from http://www.gene.com/gcne/products/information/immunological/xolair/inscrt.jsp.
18. Leonard! C: Efalizumab: an overview. J Am Acad Dermatol 2003;49(2 Suppl): 98-104.
19. MD Consult. Newest I;DA Approvals: Psoriasis indication approved for Raptiva. Drug Information 2003. Retrieved November 11,2003 from http://home. mdconsult.com/das/news/body/l/drug/0/120104/l.html?pos=ncwfda.
20. Genentech. Prescriber Information: Raptiva (cfali/Aimab) 2003. Relieved November 31, 2003 from www.raptiva.com.
21. FDA Talk Paper TO3-66. FDA Approves First in New Class of Antibiotics. September 12, 2003 Retrieved November 30, 2003 from http://www.fda. gov/bbs/topics/ ANSWERS/2003/ANS01252.html.
22. Cubist Pharmaceuticals. Cubicin 2003. Retrieved November 31, 2003 from http://www.cubicin.com/documents/cubicin_large_pi.pdf.
23. O'Mara NB. Rosuvastatin (Crestor). Detail-document #190801 2003. Retrieved 31/10/2003 from www.prescribersietter.com.
24. McTaggart, F, Bucket! L, Davidson, R, et al: Preclinical and clinical pharmacology of rosuvastatin, a new 3-hydroxy-3-methyIglutaryl cocn/.ymc A rcductase inhibitor. Am J Cardiol 2001;87(5A):28B-32B.
25. Jones, PH, Davidson, MH, Stein, EA, et al: Comparison of the efficacy and safety of rosuvastatin versus atorvastatin, simvastatin, and pravastatin across dosses (STELLAR trial. Am J Cardiol 2003;92: 152-60.
26. GlaxoSmithKIine. Press Archive 2003. Retrieved November 30, 2003 from http://www.gsk.com/press_archive/ press_l 1012001.htm.
27. GlaxoSmithKIine. Prescribing Information 2003. Retrieved November 30, 2003 from http://us.gsk.com/products/assets/us_coreg.pdf.
28. Fillmyscripts. Pricing 2003. Retrieved November 30,2003 from http://www. fillmyscripts.com/Shopping.aspx http://www.fda.gov/medwatch/SAFETY/ 2003/03SEP_PI/Coreg_PI.pdf.
Gary Laustsen, RN, PhDc, CFNP
Lynn Wimett, RN, ANP, EdD
ABOUT THE AUTHORS
At Regis University, Denver, CoIo., Gary Laustsen is an Assistant Professor of Nursing, and Lynn Wimett is an Associate Professor of Nursing.
Copyright Springhouse Corporation Feb 2004
Provided by ProQuest Information and Learning Company. All rights Reserved