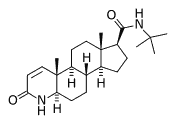
Androgenic hormones are known to influence the development of prostate cancer. Finasteride blocks the conversion of testosterone to the more potent androgen, dihydrotestosterone. Thompson and colleagues conducted a multicenter trial of finasteride for primary prevention of prostate cancer.
The authors enrolled 18,882 men older than 55 years who had a normal digital rectal examination, a prostate specific antigen (PSA) level below 3.0 ng per mL, and no clinically significant medical comorbidity. The patients were randomized to finasteride in a dosage of 5 mg daily or matching placebo. Each patient had an annual digital rectal examination and PSA level determination. Any patient with an abnormal digital examination or PSA level above 4.0 ng per mL underwent an ultrasound-guided needle biopsy, with a minimum of six samples obtained. The PSA level was doubled in those randomized to finasteride to provide an equivalent level, compared with those taking placebo. Four years into the study, this factor was increased to 2.3 to best equalize the number of patients in the two groups reaching the threshold for needle biopsy. All participants were offered needle biopsies at the end of the seven-year trial.
By the end of the study, biopsy-proven prostate cancer was detected in 18.4 percent of subjects taking finasteride, compared with 24.4 percent of those taking placebo. The decreased relative risk of developing prostate cancer while taking finasteride was not changed substantially by age, race, family history of prostate cancer, or PSA level at study entry. High-grade prostate cancer (Gleason score of at least 7 out of 10 on histologic grading of a cancer biopsy specimen) was more commonly found in finasteride users (37 percent of cancers detected in that group) than in those taking placebo (22.2 percent of detected cancers).
During the trial, approximately one half of all recommended biopsies were declined by patients, but the refusal rate did not differ significantly between the finasteride and placebo groups. The reported prevalence of erectile dysfunction or loss of libido increased from about 60 percent among placebo recipients to approximately 66 percent in the finasteride group. Rates of urinary frequency, incontinence, and urinary retention episodes were all slightly lower in patients taking finasteride.
The authors conclude that use of finasteride over a seven-year course decreases the overall rate of detected prostate cancer, but the drug does have sexual side effects and is associated with an increased incidence of high-grade prostate cancers.
Thompson IM, et al. The influence of finasteride on the development of prostate cancer. N Engl J Med July 17, 2003;349:215-24.
EDITOR'S NOTE: An accompanying editorial by Scardino (1) points out that the increase in high-grade cancers in the finasteride group may occur because these aggressive cancers are less dependent on androgens for growth and may have had a selective advantage in an environment of decreased dihydrotestosterone. Perhaps more important than this caution about the increased incidence of high-grade cancers, he added, is that the large majority of prostate cancers detected during the trial were asymptomatic and low-grade. Whether decreasing the rate of these cancers would actually translate into improved survival down the road is unknown and may be suspect given the known high overall survival rates for untreated prostate cancer.--B.Z.
REFERENCE
(1.) Scardino PT. The prevention of prostate cancer--the dilemma continues. N Engl J Med 2003;349: 297-9.
COPYRIGHT 2004 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group