Liver has a unique spectrum of unctions, and is intricately linked to the other organs. An abnormality of the liver has great impact on every system of the body. Abscess in the liver is uncommon, difficult to localize and often difficult to drain adequately.
The Patient
On a quite Tuesday morning during my clinical rounds in the general surgical ward, I met Mr. K. 54 years old tea estate worker from Valparai. He was extremely debilitated and undernourished. He seemed anxious, frustrated & helpless.
History
He was admitted with low grade intermittent fever, pain in right hypochondria, jaundice, and clay coloured stools and high coloured urine for two weeks and with history of non-exertional breathlessness for three days.
He was from poor socio economic background, earning Rs. 3,500 per month. He used to be a smoker (10 beedies/day) and consumed alcohol regularly from 16 years of age and stopped the habit of smoking and drinking alcohol five years back.
The patient's physical examination was essentially remarkable. On examination, he was conscious, oriented, and febrile; icterus and bilateral pitting edema were present. His weight was 42 kg and height was 159 cm. Abdomen, soft and swelling, was seen in right hypochondrial region. Liver was film and tender and hepatomegaly was also present. Engorged veins were noticed over anterior abdominal wall. His vital signs were as follows: Temperature -102 degree F; Pulse - 98/mt; Respiration - 22/mt & BP-130/80 mmHg. He was given cool sponge bath & administered inj. Febrinil lamp as prescribed to bring down his body temperature to normal. Pruritis was controlled by
* Cool sponge baths
* Use of soft linens
* Trimmed nails
* Prevention of dry skin with emollients and moisturizers
* Cool environmental temperature.
The nurse obtained specimen for a blood studies, liver function test & obtained a USG abdomen. The results showed an increase in ESR level and WBC counts due to infection and a decrease in hemoglobin level to the extent of 6 gms/ dl (normal value 13-15 gms).
The liver function test showed a remarkable decrease in albumin level 1.7 gms/dl (3.7-5.3 gms/dl) and an increase in transaminase level due to liver cell damage & also hyperbilirubinemia2.6mg/dl (1.43 mg/ dl) was present. USG abdomen showed multiple loculated liver abscess and subphrenic abscess with multiple abdominal abscesses and from subphrenic abscess, 750 ml of green colored pus was drained. The pus was sent for culture and the report suggested few gram positive cocci in single and occasional gram negative bacilli were present.
From the above findings the patient was diagnosed as having liver abscess which was not having the characteristics of neither amebic nor pyogenic liver abscess.
Preoperative Management
He was treated with:
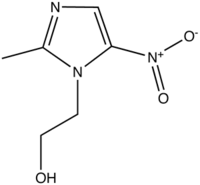
* Inj. Magnex 1 gm IV BD (Magnesium suplphate)
* Inj. Flagyl 500 mg IV Tid (metronidazole)
* Inj. Rantac 50 mg IV BD
* Inj. Febrinil 1amp SOS
* Inj. Vit 1 amp OD
He was on NPO, Ryles tube aspiration and DNS/RL 100ml/hr was administered alternatively. Fresh frozen plasma and 'O' positive blood were transfused to him in order to correct hypoalbuminemia & anemia respectively.
Intraoperative Management
As his general condition was stabilized, next day he was prepared for laproscopic surgery which was changed into laprotomy with open drainage due to incomplete drainage of pus (from multiple abscess). During surgery, drainage tube was kept in Morrison's pouch and another in the pelvis.
Postoperatively his general condition improved. After three days of surgery (third post op day), suddenly he developed severe diffused abdominal pain which wasn't relieved by analgesics. Endoscopy was performed and active ulcer was seen in the anterior inferior wall of the duodenum. Immediately patient was prepared and taken for second surgery. During the surgery it was surprising the ulcer was already perforated. Closure of perforation with feeding jejunostomy and cholycystectomy was performed.
Findings during surgery were:
* Lot of clots present all over abdominal cavity.
* Large ulcer 1.5 and 2 cm in first portion of duodenum.
* Gallbladder fundus adherent with ulcer and partially sealed.
Drainage tube was kept in the proximal jejunum. Gallbladder biopsy was sent and result showed chronic cholecystitis.
Postoperative Management
Immediately after second surgery, the patient was on mechanical ventilator in SIMV mode and advised for NPO, IV fluids, NG aspiration, chest physio & stockings. After 24 hours postoperatively (sixth post op day of first surgery & first post op day of second surgery), he was weaned from mechanical ventilator as his respiratory condition had improved. Post operatively, he was treated with
* Inj. Saltum 1.5 gms iv q8h
* Inj. Amikacin 500 mg IV BD
* Inj. Metrogyl 500 mg IV Tds
* Inj. Pantocid 40 mg IV BD (Ranitidine hydrochloride)
* Inj. Tramazac 75 mg IM stat (Diclofenac sodium)
* Inj. Febrinil 1 amp SOS
* Inj. MVI
Nursing Management
Altered nutritional status less than body requirements: His weight was 42 kg and was extremely debilitated & undernourished. High protein diet (NOVA) 60 gms/day was given through jejunostomy feeding 30 ml/hr.
Fluid and electrolyte imbalance: Initially DNS/RL 100 ml/hr was administered to replace deficits. Later the fluid rate was increased to 125 ml/hr. Intake and output chart was maintained hourly and a positive balance was maintained.
Fluid and electrolyte imbalance: Drainage was greenish in colour. Initially it was 400 ml and was continuously increasing in amount (more than 700ml). The serum potassium level was checked & result showed serum potassium level was too low 2.63 mEq/I (3.5-5mEq/I). It was treated with Inj. Kcl 40mEq/L intravenously and a decision was taken to refeed the drainage fluid (bile) nearly 30 ml/hr to him through nasogastric tube to prevent bicarbonate and potassium loss. This improved the potassium level to 3.6 mEq/L.
Impaired skin integrity : Surgical wound was soaked with bile and ostomy bag was used to prevent skin irritation. Sterile dressing was done twice daily.
After a week, gradually the drainage amount was decreased to 25 ml/day and surgical wound was healthy and healing. Jejunostomy feeding was supplemented with oral feeding as tolerated.
Condition at Discharge
* Weight - 45 kg
* Hb-11.2 gms/dl
* Albumin - 2.5 gms/dl
* Potassium - 4.46 mEq/L
Surgical wound was healthy and healing. His general condition had improved.
The health education was given to the patient and family about * importance of continuing adherence to medication regimen, and * reporting and signs and symptoms of :
1. infection (Chills, fever, diaphoresis)
2. spread of infection (worsening abdominal pain, increased difficulty in breathing)
3. deteriorating liver function (jaundice, ascities)
4. side effects of medicine
5. follow up.
Discharge teaching was given regarding :
* Prevention of recurrence
* Identification of potential contaminated sources of food and water and help to identify ways to decontaminate or avoid these sources such as iodine-releasing tablets in water and scalding of vegetables and not eating peeling of fresh fruits.
Conclusion
Because of advancement of technology in surgical procedures and nursing interventions, the patient's general condition was gradually improving. Ryle's tube, drainage tube and jejunostomy tube were removed. He was receiving solid bland high protein diet orally. Stool and urine became normal in colour. He was completely relieved from effects of the disease and happy at the time of discharge.
It was an amazing experience to study this case which helped me to enrich my knowledge & skills in giving care to the patient with liver abscess. I understood that the loculated liver abscess is a very complicated condition & it is very essential for the nurse to understand the course of the disease progress. Modern nurse has a very important role in making continuous assessment and providing high tech care to the patient which is only possible with specialized knowledge, willingness to serve and ability to perform effectively.
Bibliography:
1. Abid Sattar., Ramesh V. S., Bhooshan Pandit, Shobna J Bhatia. (2003). Amebic liver abscess in a tertiary care center. Indian Journal of Gastroenterology 22 (sup 1) A46-A47.
2. L. H. Blungart., (1988). Surgery of the Liver & Biliary Tract (vol II). Chruchil Livingstone; New York (933-942)
3. Michael J. Zinner et al (1997). Abdominal operations (VoI II). Prentice Hall International: New Jersey.
4. Mc Dermoh. W.V., Surgery of the liver. Blackwell scientific publication: Cambridge.
5. Phipps. W et al (1995). Medical surgical nursing (5th ed.) Mosby: St. Louis.
6. R. C. G. Russell., Williams. N. S., Bulstrode C. J. K., (2000). Short practice of surgery (23rd ed.) Arnold: publication.
7. Smeltzers. c., bare b.c., (1996). Text book of medical surgical nursing (8th ed.) Lippincot: St. Lewis.
The author is Assistant Professor at P.S.G. College of Nursing, Coimbatore.
Copyright Trained Nurses' Association of India Oct 2005
Provided by ProQuest Information and Learning Company. All rights Reserved