Incontinence Comes Out of the Closet
Unless 9-year-old Linda is wakened for a trip to the bathroom several times a night, she wets the bed. She's afraid to go on "sleep-overs' with friends, and time after time she comes home with her sweater tied around her hips to hide the fact that she's wet her clothes.
Greg, a successful young businessman, quit his job right after being promoted. The new position involved travel and, on the road, he was required to share hotel rooms. But he couldn't face his co-workers' finding out about his incontinence. Greg settled for a lower-paying job elsewhere.
Marion, age 72, dreads returning to her dentist. She wet the dental chair during her last visit because her appointment took longer than she had anticipated.
For Linda, Greg, Marion, and otherswho suffer from urinary incontinence, or the involuntary passing of urine, here's good news: Incontinence can be treated and often cured, even in the elderly.
The National Institute on Aging estimatesthat over 12 million Americans are incontinent. In nursing homes, more than 50 percent of patients over 65 are so affected; in fact, incontinence is the second most common reason for institutionalizing older people. (Dementia, or mental deterioration, is the first.) Outside nursing homes, incontinence afflicts about 17 percent of elderly men and 37 percent of elderly women. It's particularly troubling for older women because they generally live longer than men.
Incontinence is costly, in dollars andin psychological trauma. U.S. Surgeon General C. Everett Koop has estimated that, in nursing homes alone, the annual cost of caring for incontinent people is nearly $8 billion. And though incontinence isn't life-threatening, the stigma attached to clothes-wetting, bed-wetting, and the resultant odor can inflict profound consequences: humiliation, depression and social withdrawal. Even in the lives of people with only mild leakage, incontinence can be a ruling force.
Sad to say, only one in 12 peoplewith incontinence seeks medical help-- a fact perhaps due to embarrassment, isolation, or the mistaken notion that incontinence is normal with aging.
"Incontinence is no more a normalpart of aging than is chest pain or diabetes,' said Dr. Neil Resnick, of the Harvard Medical School, at a national conference sponsored in 1986 by the Food and Drug Administration and the Public Health Service Coordinating Committee on Women's Health Issues.
Normally, the urinary system removeswaste products from the body in a well-coordinated fashion. Through nerve pathways, the brain synchronizes the individual housecleaning tasks that nature has assigned to different body parts: The two kidneys move wastes from the blood into the urine, tubes called ureters (one per kidney) channel the urine to the sac-like muscle called the bladder for storage, and then, as needed, two sphincter muscles open and close the bladder outlet to control urine flow to the outside via a tube known as the urethra.
But sometimes the system doesn'twork the way it's supposed to. As Harvard's Resnick put it: "Either the bladder contracts when it should not, leading to the patient's being wet, or it fails to contract when it should, so that urine builds up and spills over . . .. Either the outlet is open when it ought to be closed or it is closed when it ought to be open.' Resnick added that such factors generally associated with aging, such as illness, medicines, and the weakening of the urinary system, can increase a person's risk of incontinence.
Incontinence occurs when one of thoseworking parts is adversely affected-- by an obstruction in the urethral tube, for instance, or by an abnormality in the sphincter muscle, bladder muscle, or both. It may result from a condition as common as chronic constipation, particularly if stool is impacted, or from the lack of nearby toilets, as may be the case for some patients in institutions. It may develop after a hysterectomy or prostate, rectal, or lower intestinal surgery. Obesity and childbirth also can contribute to incontinence. Other causes include drug side effects, multiple sclerosis, cancer, spinal cord injury, diabetes mellitus, stroke, Parkinson's or Alzheimer's disease, and birth defects --80 percent to 90 percent of children born with spina bifida are incontinent.
When acute (relatively severe, butof short duration) incontinence occurs, it's generally the result of another acute medical problem. For instance, a heart attack or some type of infection may cause a mental state called delirium, in which consciousness can become so clouded that the patient has difficulty controlling the bladder. Persistent incontinence, on the other hand, is not associated with an acute medical problem; it often worsens over time and can occur in different ways:
Stress incontinence. Minor physicalstress such as coughing, sneezing, laughing or lifting results in small amounts of urine leakage. This is common in older women, but is usually not seen in men unless there has been sphincter damage during surgery.
Overflow incontinence. The persondoesn't feel the urge to void or isn't able to urinate normal amounts ("normal' generally being 8 to 20 ounces), so the bladder overfills and spills small amounts of urine.
Urge incontinence. The person feelsa strong desire to urinate, but can't get to a toilet before the bladder empties.
Primary enuresis (EN-you-REE-sis).This is the term most commonly used for bed-wetting in children beyond the age (5 years) when they should be capable of bladder control and in adults who never gained nighttime control.
Reflex incontinence. The bladderfills and empties without the person's having any mental control over it at all.
The key weapon in the psychologicaland physical battle to stay dry is: Tell your physician about the incontinence, so that a correct diagnosis can be made and treatment options can be discussed. Ask whether you should consult a specialist in treating incontinence (for children, for example, a urologist who specializes in pediatric problems; for adults, a geriatrician, gynecologist or urologist). Early diagnosis and treatment are important for many reasons, but they can be life-saving when the incontinence is the first sign of a serious medical condition, such as a tumor. If help isn't forthcoming, see another doctor. are important for many reasons, but they can be life-saving when the incontinence is the first sign of a serious medical condition, such as a tumor. If help isn't forthcoming, see another doctor.
To begin the medical investigation,the physician usually takes a patient's history and performs an examination. Urine and blood specimens are collected, and tests are performed--how many and what type depend on the patient's symptoms and history.
Patients may be asked to undergoprocedures called "urodynamic' tests to help the physician pinpoint whether the problem lies in the urinary system and, if so, where. They're done on an outpatient basis. One such test measures the speed of urine flow from the bladder as the person urinates into a special toilet connected to a machine. An obstruction would cause the flow to be slower than normal. Other procedures test the sphincter and bladder muscles, as follows: One end of a catheter (a small plastic tube) is passed up the urethra to the bladder, and an electrode carried by the catheter is attached to the sphincter. Then, electrical impulses coming from the sphincter muscles and pressure changes within the bladder are recorded. The physician evaluates the readings to see whether the muscles are functioning normally.
Other types of tests may be orderedas well.
Physicians treat incontinence by treatingits underlying cause. Treatments include:
Battery-operated alarm. Used forbed-wetting, the alarm is triggered by the wetting. Initially, for children, it may be necessary for someone in the household to respond to the alarm and waken the patient. Once patients become conscious of the alarm, they should waken on their own when it rings. Eventually, the patients are supposed to become so used to waking when wetting occurs that they start waking beforehand.
Scheduled voiding regimens. Forurge incontinence, patients may be asked to wait longer before urinating, gradually increasing the "waiting period,' or to urinate only at assigned intervals. Mentally impaired patients may be prompted to stay dry by simply being asked if they need to urinate and, if so, helped to the toilet. What works for one incontinence problem may not work for another, so it's best to get medical advice before beginning a regimen. And, generally, women shouldn't put off urinating, as that can promote bladder infections.
"Kegel' exercises. In 1948 ArnoldKegel, M.D., who was practicing in Los Angeles at that time, introduced exercises to strengthen the pelvic floor muscles in women with stress incontinence and, so, to preserve or regain bladder control. It's possible to feel where these muscles are, at one end of the pelvic floor, by interrupting the flow several times during urination and, at the other end, by drawing in the muscle around the anus as if to stop a bowel movement. The patient is supposed to repeat the exercises--interrupting each urination and tightening the pelvic floor muscles from back to front--many times throughout the day.
Harvard's Resnick advises that allwomen who aren't pregnant practice Kegel exercises to strengthen the pelvic floor muscles, which, in turn, may help ward off incontinence later in life. But, he says, people usually need professional instruction to do them correctly.
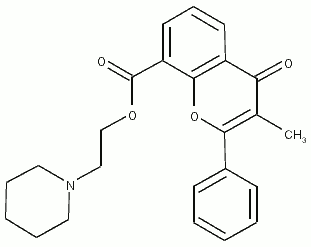
Drugs. Estrogen therapy is prescribedfor women with estrogen deficiency. The condition can cause the tissue lining of the urethra to become inflamed, and the irritated tissue can cause or worsen urge incontinence. The antispasmodic drug flavoxate is prescribed to treat incontinence associated with such conditions as cystitis (inflammation of the bladder). Flavoxate decreases muscle spasms in the bladder. However, the large dosages that are often required can be hazardous to other tissue, and the patient may have to contend with undersirable side effects, such as dry mouth, constipation, and blurred vision.
Reevaluation of drug therapy. Incontinencemay be due to drugs the person is taking for some other condition: Sedatives or tranquilizers may dull the senses so much that the urge to urinate isn't felt; anticholinergics prescribed for bowel spasm can decrease the bladder's ability to contract; diuretics, often given to lower blood pressure, increase urine production; and cold medicines may increase the bladder outlet's resistance so that the bladder doesn't completely empty. Upon reevaluation, the physician may find that a different drug will work without causing incontinence.
Surgical procedures. Even frail,elderly patients can easily tolerate a number of newer corrective procedures, says Resnick. Deep abdominal surgery is usually not required; rather, the surgeon works through the vagina or a tiny abdominal incision and uses an endoscope (a narrow tube-like instrument inserted via the urethra or the incision) to see inside the bladder. This way, the surgeon can relieve an obstruction, tie up pelvic floor tissues to return a sagging urethra or bladder to a normal position, or repair a constantly opening bladder outlet so that it closes properly. The hospital stay is usually only a day or two; a younger person may be in and out of the hospital the same day. Other surgical options may be to implant an artificial sphincter or to reconstruct the bladder. (See illustration.)
Sometimes the underlying cause ofthe incontinence can't be cured, but the situation is still far from hopeless. There are many measures to help a person stay dry: more frequent trips to the toilet, a portable commode for invalids, and self-catheterization (after proper instructions) to empty the bladder several times a day. There are urine collection devices and disposable pads and pants available from medical supply stores, certain drugstores, and home health-care catalogs. One product may work better than another, so a person may want to try several. Also, oral deodorant tablets can be taken as an aid to reduce urinary odor. The active ingredient, chlorophyllin copper complex, helps to mask the odor.
Incontinence will probably never leadthe list of tea-time topics of conversation. But health professionals, public health officials, women's groups, the media, makers of incontinence-related products, and others personally acquainted with the difficult problem are erasing the incontinence stigma. Actress June Allyson, appearing in ads that promote disposable absorbent pants, unashamedly acknowledges that her mother became incontinent after a stroke and that they're dealing with it. By being so frank, Allyson also promotes the idea that it's all right to talk about incontinence. Two support groups for incontinent patients were incorporated in 1983: HIP, or Help for Incontinent People, and The Simon Foundation, whose founder-director is herself incontinent. The groups offer information about such topics as recovery after prostate surgery, cleaning urine stains from clothing, incontinence-treatment products, and treatment options. To receive an information packet (there may be a charge), send the request and a stamped, self-addressed, business-size envelope to:
HIP, P.O. Box 544, Union, S.C.29379 (phone 803-585-8789), or
The Simon Foundation, P.B. Box835, Wilmette, Ill. 60091 (phone 1-800-23SIMON).
Photo: Many retail stores now carry productsfor managing the problems of incontinence: Leakproof underpants, panty liners, and odor-masking tablets, for instance. Medical supply stores sell a number of other aids intended for use with a doctor's advice. At left center is a urine collection system for use at bedside. Also shown are collection devices for use away from home.
Photo: Some patients with urinary incontinence--due to cancer, for instance --may be candidates for a surgical procedure in which a portion of the small intestine is used to make a substitute bladder. The resultant "Kock pouch,' pictured here, is named for the procedure's developer, Nils Kock, M.D., of Sweden. The surgeon first removes the bladder and dataches a segment of the small intestine to make the pouch and two valves, one for each end of the pouch. Collars of synthetic material are used to hold the valves in place. One end of the pouch is connected to the ureters; the valve there allows urine to flow freely from the kidneys into the pouch, but prevents backward flow. The other end opens to the outside through the abdomen; that valve prevents leakage and allows the patient to insert a catheter for drainage, as needed. No external collecting device is required.
COPYRIGHT 1987 U.S. Government Printing Office
COPYRIGHT 2004 Gale Group