Make sure you can administer this antiarrhythmic drug safely.
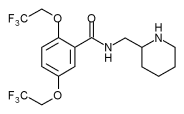
Flecainide (Tambocor) is a Class IC antiarrhythmic agent used to suppress and prevent lifethreatening ventricular arrhythmias such as sustained ventricular tachycardia in patients without structural heart disease. It's also indicated to prevent paroxysmal supraventricular tachycardias (PSVTs) and paroxysmal atrial fibrillation and flutter in patients with disabling symptoms. Because of its potentially life-threatening adverse effects, flecainide is reserved for patients whose arrhythmias haven't responded to other therapies. For complete drug information, see the package insert.
Q. How is flecainide administered and what's the usual dosage?
A. Flecainide is available as 50-mg, 100-mg, and 150-mg tablets. The usual initial adult dosage to treat sustained ventricular tachycardia is 100 mg P.O. every 12 hours, increased by 50 mg every 12 hours every 4 days. The daily maintenance dosage is 200 to 400 mg orally; the maximum daily dosage is 400 mg orally.
To treat PSVT or atrial fibrillation, the usual initial adult dosage is 50 mg orally every 12 hours, increased 50 mg every 12 hours every 4 days. The maximum daily dosage is 300 mg orally. In patients with severe renal impairment (creatinine clearance less than 20 ml/minute), reduce the initial dosage 25% to 50%.
Q. What adverse reactions should I watch for?
A. Like other antiarrhythmics, flecainide can produce new supraventricular or ventricular arrhythmias, worsen heart failure, or cause heart block. Because of these potentially serious adverse reactions, flecainide therapy should be started in the hospital, where the patient's cardiac rhythm can be monitored. Common adverse reactions are dizziness, visual disturbances, headache, fatigue, weakness, palpitations, nausea, and shortness of breath.
Q. When is flecainide contraindicated?
A. Flecainide is contraindicated in patients with second- or third-degree atrioventricular block or with right bundle-branch block when associated with a left hemiblock (bifascicular block) unless the patient has a pacemaker. Flecainide is also contraindicated in patients who are in cardiogenic shock and those hypersensitive to the drug.
Q. Which drugs interact with flecainide?
A. Flecainide may increase blood levels of digoxin and propranolol; patients taking propranolol and flecainide also may have increased flecainide levels. Cimetidine can increase flecainide blood levels 30%, so tell your patient to avoid taking over-the-counter products containing cimetidine.
Amiodarone also increases flecainide blood levels by an average of 60% (range, 5% to 190%). Disopyramide or verapamil, when taken with flecainide, can cause additive negative inotropic effects. These drugs shouldn't be given together unless the benefits outweigh the risks. Patients taking quinidine and flecainide may have increased flecainide concentrations.
Q. How should I monitor a patient who's receiving flecainide?
A. Initiate flecainide while your patient is hospitalized and monitor cardiac rate and rhythm, electrocardiogram, blood pressure, and kidney and liver function. Monitor his potassium and electrolyte levels to avoid imbalance-induced arrhythmias. Flecainide trough plasma levels should stay between 0.2 and 1 mcg/ml. Monitoring flecainide trough levels is especially important in patients with severe kidney or liver disease; slow elimination can result in toxic blood levels and adverse reactions.
Tell your patient to report any new or worsening symptoms, such as chest pain, palpitations, or dizziness.
SELECTED REFERENCES
American Hospital Formulary Service. Bethesda, Md., American Hospital Formulary Service, 2002.
Flecainide prescribing information. Northridge, Calif., 3M Pharmaceuticals, 1998.
Nursing2004 Drug Handbook, 24th edition. Ambler, Pa., Lippincott Williams & Wilkins, 2004.
By Marcy Portnoff Gever, PharmD, MEd
Marcy Portnoff Gever is an independent pharmacist consultant and educator in Ringoes, N.J.
Copyright Springhouse Corporation Dec 2004
Provided by ProQuest Information and Learning Company. All rights Reserved