Background: Inhaled corticosteroids (ICSs) reduce local airway inflammation, which is an underlying cause of asthma symptoms. However, potential systemic side effects associated with ICS use are a major concern for asthmatic patients.
Methods: Adult patients (n = 60; [greater than or equal to] 18 years of age) with moderate-to-severe asthma were randomized to receive 4 weeks of treatment with ciclesonide (CIC), 320 [micro]g bid (CIC 640), CIC, 640 [micro]g bid (CIC 1280), fluticasone propionate (FP), 440 [micro]g bid (FP 880), FP 880 [micro]g bid (FP 1760), or placebo (PBO) [all doses expressed as ex-actuator; comparable to ex-valve doses of 800 and 1,600 [micro]g/d for CIC and 1,000 and 2,000 [micro]g/d for FP, respectively].
Results: After 29 days of treatment, CIC 640, CIC 1280, and FP 880 had no significant effect on the mean serum cortisol area under the curve for 0 to 24 h (AUC0-24h). FP 1760 produced a statistically significant suppression in mean serum cortisol AUC0-24h compared to PBO (p = 0.0009; 95% confidence interval [CI], = 117.5 to -32.1). Results obtained with cosyntropin st4imulation revealed no statistically significant differences among the groups. The CIC 640 group demonstrated a significant increase compared to the PBO group in 24-h urinary cortisol levels from baseline at week 4 (p = 0.0224; 95% CI, 0.0023 to 0.0283), while the other treatment groups revealed no change in this parameter. The incidence of treatment-emergent adverse events was similar in all groups, and all adverse events were mild or moderate in severity.
Conclusion: Treatment with moderate and high doses of CIC does not result in hypothalamic-pituitary-adrenal-axis suppression as compared with PBO.
Key words: asthma; ciclesonide; cortisol; fluticasone; hypothalamic-pituitary-adrenal axis
Abbreviations: ACTH = adrenocorticotrophic hormone; ANCOVA = analysis of covariance; AUC0-24h = area under the curve for 0 to 24 h; CFC = chlorofluorocarbon; CI = confidence interval; CIC = ciclesonide; CIC 640 = ciclesonide, 320 [micro]g bid; CIC 1280 = ciclesonide, 640 [micro]g bid; des-CIC = desisobutyryl-ciclesonide; FP = fluticasone propionate, FP 880 = fluticasone propionate, 440 [micro]g bid; FP 1760 = fluticasone propionate, 880 [micro]g bid; HFA = hydrofluoroalkane; HPA = hypothalamic-pituitary-adrenal; ICS = inhaled MDI = metereddose inhaler; OCS = oral corticosteroid; PBO = placebo
**********
Bronchial asthma is an inflammatory disease that is characterized by intermittent or chronic airway obstruction and airway hyperresponsiveness to exogenous allergens and/or physical stimuli. (1-3) Inhaled corticosteroids (ICSs) are generally accepted as first-line therapy for the long-term treatment of asthma owing to their antiinflammatory effects, which reduce the severity of symptoms, improve pulmonary function, diminish airway hyperresponsiveness, and prevent exacerbations and, possibly, airway remodeling. (4-6) Consequently, treatment guidelines advocate the early introduction and sustained use of ICSs in asthmatic adults and children. (2,3,7)
ICSs at recommended doses are generally safe, but the availability of newer more potent forms, the advent of chlorofluorocarbon (CFC)-free formulations that deliver the drug more effectively, and the trend toward higher and longer dosing have contributed to concerns regarding the safety of long-term treatment. (8-12) Known adverse effects of ICSs include oropharyngeal candidiasis and dysphonia, and the more serious systemic effects of adrenal insufficiency, Cushing syndrome, osteoporosis and bone fracture, posterior subcapsular cataracts, skin bruising, and possibly decreased growth velocity. (13,14) The systemic activity of corticosteroids, and their potential for adverse systemic effects, are generally assessed by the degree to which they cause hypothalamic-pituitary-adrenal (HPA)-axis suppression. (9,15,16)
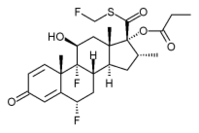
Ciclesonide (CIC), the newest generation of ICSs, is inhaled as an inactive parent compound, which is then hydrolyzed to its active form, desisobutyryl-CIC (des-CIC). CIC has been designed to have several favorable pharmacokinetic characteristics such as low oral bioavailability, rapid clearance, and high serum protein binding that would limit systemic exposure and side effects, while maintaining potent glucocorticoid receptor-binding activity in the lung. (17-21) Des-CIC, with a receptor-binding affinity 12 times that of dexamethasone, has one of the highest receptor-binding affinities for an ICS (relative receptor affinity, 1,200). (22) In addition, CIC is administered using a metered-dose inhaler (MDI) in a solution of hydrofluoroalkane (HFA) propellant, which allows for the production of small, highly respirable particles, which result in a significant percentage (>50%) of the administered dose being topically deposited in the lungs. (22,23)
The present study investigated the potential effects of CIC at doses of 320 and 640 [micro]g bid on HPA-axis function in patients with moderate-to-severe asthma. This is the first study to examine the effects of high doses of CIC for a prolonged duration (4 weeks) in patients with moderate-to-severe asthma. The overall study design was similar to that of the study of Affrime et al (24) and was double-blind, parallel, and placebo (PBO)-controlled. Treatment was administered for 4 weeks and included fluticasone propionate (FP) [440 and 880 [micro]g bid using an MDI-CFC] as an active comparator. The primary evaluation of HPA-axis function was the measurement of serum cortisol area under the curve for 0 to 24 h (AUC0-24h). Additional evaluations were the determination of the serum cortisol response to low-dose (1 [micro]g) cosyntropin and the measurement of 24-h urinary cortisol levels corrected for creatinine.
SUBJECTS AND METHODS
Study Population
The study population consisted of nonsmoking male and female adults ([greater than or equal to] 18 years of age) who had a [greater than or equal to] 3-month history of moderate-to-severe persistent asthma (FE[V.sub.1], [greater than or equal to] 40% and [less than or equal to] 80% of predicted). To be eligible, patients had to demonstrate at least a 12% reversibility of FE[V.sub.1] following two inhalations of albuterol (or a documented history of at least a 12% reversibility within 1 year). In addition, patients had to demonstrate normal HPA-axis function, which was defined as a basal AM serum cortisol level of [greater than or equal to] 5 [micro]g/dL and a serum cortisol level of [greater than or equal to] 18 [micro]g/dL at one or more of the following time points following the administration of low-dose (1 [micro]g) synthetic adrenocorticotrophic hormone (ACTH) cosyntropin (Cortrosyn; Organon Pharmaceuticals; Roseland, NJ): 20 min; 30 min; or 60 min. Women receiving oral contraceptives or hormone replacement therapy were also required to have an increase in serum cortisol levels of [greater than or equal to] 7 [micro]g/dL from basal to peak levels. Oral contraceptives (OCs) and hormone replacement therapy are known to bind to cortisol-binding globulin,s and the plasma certisol concentration is approximately twice as high in women who are receiving an oral contraceptive than in those who are not. (25) Additional]y, patients had to demonstrate that they could properly use an oral inhaler.
Patients were excluded from the study if they had a documented history of drug or alcohol abuse, had used ICSs, intranasal steroids, or ICSs in combination with long-acting bronchodilators within 3 months prior to screening, had used systemic corticosteroids within 3 months prior to screening or any investigational drug within 30 days prior to screening, or had used concomitant medications that were expected to interfere with the interpretation of study data. Any patient with a history of cardiovascular, pulmonary, neurologic, hepatic, renal, or any significant acute or chronic illness was also excluded. Patients who had oral candidiasis within 30 days prior to screening and female patients who were pregnant or lactating were excluded from the study.
Study Design
This was a single-center, randomized, double-blind, double-dummy, multiple-dose, parallel-group trial comparing the effects of CIC (R-CIC; Aventis Pharmaceuticals; Bridgewater, NJ), FP (Flovent; GlaxoSmithKline; Research Triangle Park, NC), and PBO on HPA-axis function in adult asthmatic patients with normal AM cortisol values at screening (Fig 1). The baseline period encompassed visits 1 to 3 (ie, days -14 to -9, days -10 to -7, and day -1). Double-blind treatment visits occurred at day 1 (randomization), day 8 (week 1), day 15 (week 2), day 22 (week 3), day 29 (week 4), and day 30 (hospital discharge). At visits 1 and 2 (prescreening and screening, days -14 to -7), adult patients with moderate-to-severe persistent asthma were assessed for eligibility to enter the study. Those meeting the inclusion criteria were classified as eligible patients (n = 60) on day -1 (visit 3), were admitted to the clinic as inpatients, and were randomized (day 1) to receive one of the following five treatments for 29 days: CIC, 320 [micro]g bid (CIC 640); CIC, 640 [micro]g bid (CIC 1280); FP, 440 [micro]g bid (FP 880); FP, 880 [micro]g bid (FP 1,760) [all doses are expressed as ex-actuator and were comparable to ex-valve doses of 800 and 1,600 [micro]g/d for CIC and 1000 and 2000 [micro]g/d for FP, respectively]; or PBO. Treatments were administered via MDI with an HFA-134a propellant for CIC (MDI canisters delivering 80 and 160 [micro]g per puff) and a CFC propellant for FP (MDI canisters delivering 110 and 220 [micro]g per puff). Each patient was provided with two MDI canisters of study medication in a blinded manner (ie, double-dummy) at randomization with at least one of the canisters being a PBO. Patients were to inhale four puffs from each MDI in the morning (at 8:00 to 8:30 AM) and four puffs in the evening (at 8:00 to 8:30 PM). Albuterol canisters were provided to the patients as rescue medication.
[FIGURE 1 OMITTED]
Patient compliance was assessed by canister weight and patient diaries. All study medication was administered under the direct supervision of the investigator/coordinator to confirm that the proper dose was taken and the proper inhalation technique was used. A patient was considered to be compliant on a given day if they took the study medication as per the protocol for that day (total, 16 puffs per day; ie, 4 puffs from each of the two canisters in the morning and 4 puffs from each of the two canisters in the evening). The overall percentage of compliance was defined as the percentage of compliant study days of all study days.
The investigation was conducted in accordance with the good clinical practice guidelines established by the International Conference on Harmonization in conformity with the Declaration of Helsinki. The clinical study protocol and informed consent documents were reviewed and approved by an independent ethics committee/institutional review board. Informed consent was obtained from all patients prior to conducting any study-related procedures. The safety of the various drug treatments was examined using clinical pharmacodynamic evaluations of HPA-axis function, laboratory results, and emergent adverse events due to treatment.
Pharmacodynamic Outcomes
Serum Cortisol AUC0-24h: The primary outcome was the change from baseline to day 29 in the serum cortisol concentration AUC0-24h. Twenty-four-hour serum cortisol levels were determined on day -1 (baseline period, prior to randomization) and at days 8, 15, 22, and 29. Blood samples (approximately 2.5 mL) were collected and analyzed from patients at over 24 h at 8:00 AM, 9:00 AM, 10:00 AM, 12:00 PM, 2:00 PM, 4:00 PM, 6:00 PM, 8:00 PM, and 10:00 PM of one day, and 12:00 AM, 2:00 AM, 4:00 AM, 6:00 AM, 7:00 AM, and 8:00 AM of the following day. Serum was isolated from each sample by centrifugation (1500g for 10 min), and cortisol was measured by electrochemiluminescence immunoassay (Elecsys Cortisol kit; Roche Diagnostics; Indianapolis, IN) at a central laboratory (Covance Central Laboratory Services; Indianapolis, IN). Briefly, the sample was incubated with a cortisol-specific biotinylated antibody and a ruthenium complex-labeled cortisol derivative. On the addition of streptavidin-coated microparticles, the complex was bound to a solid phase via interactions of both biotin and streptavidin. The microparticles were then magnetically captured on the surface of an electrode; the application of a voltage produced a chemiluminescent signal. The lower limit of quantitation of the assay was to 0.3 [micro]g/dL; the intra-assay precision was 1.0 to 1.4% coefficient of variation, and the inter-assay precision was 2.1 to 5.4% CV. Serum cortisol AUC0-24h values were calculated using the trapezoidal rule for numerical integration using the actual recorded collection times.
1 [micro]g of Cosyntropin-Stimulated Serum Cortisol: One of the secondary outcomes was serum cortisol measurements obtained after low-dose (1 [micro]g) cosyntropin stimulation. The cosyntropin test was conducted during the screening period and at day 30 (or early termination). Serum cortisol measurements were obtained 15 min prior to the administration of cosyntropin. Subsequently, 1 [micro]g of cosyntropin was injected as a 1-mL bolus between 8:00 AM and 8:15 AM. Blood samples were collected at 20, 30, and 60 min after the cosyntropin injection. The peak cortisol level was defined as the highest of the three measured serum cortisol levels. Cortisol levels in response to cosyntropin were "also determined by electrochemiluminescence immunoassay.
24-h Urinary Cortisol Level: Another secondary outcome was the change from baseline to day 29 (or early termination) in 24-h urinary free cortisol level corrected for creatinine (in micrograms per milligram creatinine). Patients were required to completely empty their bladders prior to the start of urine collection, and then collect all subsequent urine for 24 h. Urine samples were analyzed using high-performance liquid chromatography with an ultraviolet detector. Briefly, the sample was treated with methanol to extract the cortisol and to precipitate proteins, and an internal standard was added. Following solid-phase extraction through a C18 cartridge and elution with dichloromethane, the sample was dried down, reconstituted with mobile phase, and injected onto a reverse-phase ODS column. The lower limit of quantitation was 0.50 [micro]g/dL, the intraassay precision was 2.2 to 4.6% CV, and the interassay precision was 4.7 to 5.5% CV.
Safety Analysis
Safety evaluations were based on the following: (1) physical examination results, vital signs, body weight, and clinical laboratory safety values obtained during the screening period and at day 30 (or early study termination); (2) oropharyngeal examination (if a fungal infection of the mouth or throat was suspected, a culture was to be taken and sent to the central laboratory for testing to confirm the diagnosis by either symptoms or direct examination) results obtained at baseline and at days 1, 8, 22, and 30 (or early study termination); and (3) adverse events, recorded throughout the study and until 14 days after the last dose of the study drug. Hematology, serum chemistry, and urinalysis tests were carried out according to standard methodologies. All blood assays for laboratory safety and efficacy variables were conducted by one company (Covance Central Laboratory Services).
Statistical Analysis
The primary population for all pharmacodynamic analyses was the intent-to-treat population. This population included all randomized patients who had received at least one dose of study medication and who had a valid baseline measurement and at least one valid postbaseline measurement of the primary analysis variable (ie, serum cortisol AUC0-24h). The serum cortisol AUC0-24h was considered to be valid if each of the following time intervals contained at least one actual collection time of a nonmissing cortisol measurement: 7:30 am to 8:30 am; 9:30 am to < 2:00 pm; 2:00 pm to 6:00 pm; 6:00 pm to <10:00 pm; 10:00 pm to 2:00 am; 2:00 am to 6:30 am.
Demographic and baseline characteristics were summarized by treatment group and overall to assess the comparability of the five treatment groups at baseline. Continuous data were summarized using summary statistics, including the number of patients, and the mean, SD, median, minimum, and maximum values. The data for categoric variables were summarized using frequency distributions. Baseline variables were tested for among-treatment heterogeneity. The baseline imbalance for continuous variables was assessed using a nonparametric analysis of variance model with a parameter for treatment, modeled as a fixed effect. The nonparametric analysis of variance was performed by ranking the response variable without regard to treatment classification. Baseline imbalance for categoric variables was compared among treatment groups using a Cochran-Mantel-Haenszel test.
The primary analysis of change from baseline in primary and secondary variables at the end of the study was conducted using an analysis of covariance (ANCOVA) method. The ANCOVA model included such factors as age, sex, baseline FE[V.sub.1], and serum cortisol AUC0-24h as covariates. Pairwise comparisons were based on least-squares estimates and SE values from the above primary analysis model ([alpha] = 0.05 was the threshold for statistical significance for these comparisons). Two-sided 95% confidence intervals (CIs) for the treatment difference were constructed for each treatment comparison. Based on data from the study by Affrime et al, (24) and assuming an SD of 50 [micro]g*hr/dL and a mean PBO of 230 [micro]g.hr/dL for the change from baseline in serum cortisol AUC0-24h after 4 weeks of treatment, the following calculation was used: with a sample size of 12 patients per treatment group (60 patients total), the study would have 90% power (at [alpha] = 0.05, two-sided test) to detect a difference of approximately 30 percentage points with respect to mean PBO in the change from baseline in serum cortisol AUC0-24h between the two treatment groups.
RESULTS
Patient Disposition and Demographics
A total of 77 subjects with at least a 3-month history of moderate-to-severe persistent asthma and normal HPA-axis function were screened to participate in the study. Sixty subjects met the eligibility requirements and were randomized (12 per group) to double-blind treatment with CIC 640, CIC 1280, FP 880, FP 1760, or PBO. Seventeen patients were not randomized due to a failure to meet cosyntropin entry criteria (n = 10), a failure to meet FE[V.sub.1] entry criteria (n = 4), withdrawal of consent (n = 2), or smoking (n = 1). All randomized patients received at least one dose of study medication and completed the entire 29 days of treatment. Since all patients completed the study, future reference will be to "end-of-study" values.
There were no statistically significant differences in demographic characteristics among the groups at baseline (Table 1). Only 8 of the 33 female patients (of a total of 60 patients) randomized to the five groups were using OC or HRT at baseline.
Patient Compliance
Fifty-nine of 60 patients were 100.0% compliant with therapy. One patient in the FP 1760 group missed a day and a half of treatment and had an overall compliance rate of 93.3%.
Pharmacodynamics
Mean Serum Cortisol AUCO-24h: The baseline mean serum cortisol AUC0-24h values were comparable in all CIC and FP treatment groups, although the PBO group displayed a nonsignificantly higher value due to the inclusion of three patients with mean serum cortisol AUC0-24h of >300 [micro]gxh/dL (Table 2).
At the end of the study, there was no significant change from baseline in the mean serum cortisol AUC0-24h values for the PBO, CIC 640, CIC 1280, and FP 880 groups (Table 2). In the FP 1760 group, the mean serum cortisol AUC0-24h (adjusted) was significantly lower at the end of the study compared with baseline. Since the 95% CI for the difference between the day 29 and baseline values did not contain 0 (-107.1 to -49.1), this was a statistically significant effect. The mean change in serum cortisol AUC0-24h in the FP 1760 group at day 29 was also significantly different from that of the PBO group (p = 0.0009; 95% CI, -117.5 to -32.1) and the CIC 1280 group (p = 0.0013; 95% CI, 28.3 to 110.0) [Table 2]. Further, in the FP 1760 group there were more patients with reductions in serum cortisol AUC0-24h based on threshold evaluations (Table 3).
The changes in mean serum cortisol AUC0-24h in patients receiving CIC 640, CIC 1280, and FP 880 were not significantly different from those in patients receiving PBO at any time point in the trial. By comparison, the reduction in mean serum cortisol AUC0-24h with FP 1760 was statistically significant at all time points and increased with time of treatment (Fig 2).
[FIGURE 2 OMITTED]
In order to examine serum cortisol AUC0-24h independent of differences in baseline values, changes in this parameter at 29 days of treatment were expressed as the percentage change from baseline (Fig 3). At 29 days, the percentage change in serum cortisol AUC0-24h in the CIC groups was not significantly different from that of the PBO group (CIC 640, p = 0.5901; CIC 1280, p = 0.7760). The percentage change in serum cortisol AUC0-24h in the FP 1760 group was significantly different from that of the PBO group (p < 0.01). In addition, the percentage change in serum cortisol AUC0-24h for the FP 1760 group was significantly different from those of the CIC 640, CIC 1280, and FP 880 groups (p < 0.01).
[FIGURE 3 OMITTED]
1 [micro]g of Cosyntropin-Stimulated Serum Cortisol: Peak cortisol was defined as the highest of the three serum cortisol levels measured at 20, 30, and 60 min after stimulation with 1 [micro]g of cosyntropin. At baseline, precosyntropin and peak cosyntropin-stimulated cortisol levels were similar in the five treatment groups (Table 4, Fig 4, top). In the FP 1760 group, there was a decrease in the adjusted mean change from baseline. However, as indicated by the 95% CIs, none of the treatments produced a statistically significant change in the peak serum cortisol response vs baseline values (Table 4; Fig 4, middle). The degree of stimulation (ie, cosyntropin value--precosyntropin value) at baseline and following 29 days of treatment was also determined. All treatments resulted in increases in the mean degree of cosyntropin stimulation at the end of the study vs baseline; however, none of the changes were statistically significant among the treatments (Fig 4, bottom).
[FIGURE 4 OMITTED]
24-h Urinary Cortisol: The mean ([+ or -] SD) urine volume collected was 1,828.8 [+ or -] 561.1 mL. None of the treatment groups showed a statistically significant decrease in 24-h urinary cortisol levels from baseline at day 29 as compared to PBO. However, there was a statistically significant increase in urinary cortisol levels in the CIC 640 group compared to the PBO group (p = 0.0224; 95% CI, 0.0023 to 0.0283) [Fig 5].
[FIGURE 5 OMITTED]
Safety
The incidence of treatment-emergent adverse events was similar in the five treatment groups, and all adverse events were classified as mild or moderate in severity (Table 5). The body system with the highest overall incidence of events was the nervous system (33 to 50% in the different treatment groups) with headache being the most frequently reported event and the only event classified as possibly treatment-related. The percentage of patients with possibly treatment-related headache varied among treatment groups, ranging from 8.3% with CIC 640 to 41.7% with FP 880 and PBO. There were no serious adverse events. The mean baseline values for routine laboratory test results were similar across all treatment groups. The mean changes from baseline to the end of the study in laboratory values were small and not clinically significant for all study groups.
DISCUSSION
ICSs are generally accepted as first-line therapy for the long-term treatment of asthma. (2,3) Patients having severe asthma typically receive high daily doses of ICSs for extended periods of time. (2,3,7) Therefore, the known adverse events associated with ICSs have particular importance in this patient population.
CIC is a novel ICS that has a number of features designed to decrease local (oropharyngeal) and systemic side effects, while maintaining high antiasthmatic activity. (17-21) CIC is administered in solution via an MDI inhaler using HFA-134a as a propellant, with particle sizes of 1.1 to 2.1 [micro]m, (22) thus optimizing lung deposition and limiting oropharyngeal deposition. (26) CIC itself is an inactive parent compound that to a large extent is converted on-site within the lung to its active moiety des-CIC, but is only minimally converted to des-CIC in the oropharynx. (27,28) Des-CIC has excellent antiinflammatory properties by virtue of its high binding coefficient with glucocorticoid receptors. (29) Des-CIC is esterified in the target tissue, forming a storage molecule that may be retained within the lung for extended periods, (30) which may contribute to once-daily dosing. Both CIC and des-CIC possess high protein binding and rapid clearance. (22,31,32) Additionally, the oral bioavailability (due to the swallowed portion of the inhaled dose) of CIC and des-CIC is < 1%. (22,32)
CIC has been shown to be safe and effective in the treatment of persistent asthma. In randomized, PBO-controlled trials, treatment at doses up to 640 [micro]g/d improved lung function and asthma symptoms, decreased airway hyperresponsiveness, and reduced the use of rescue medication. (5,19,33-36) The doses of ICSs evaluated in the present study were based on previous clinical trial experience with CIC and the approved dosing for FP. Doses of CIC ranging from 80 to 1,280 [micro]g/d have been evaluated in US phase III studies of asthmatic patients. The highest dose of CIC in this study (1,280 [micro]g/d) was twice the highest dose evaluated in US phase III safety and efficacy trials in patients with severe asthma who were not dependent on oral corticosteroids (OCS), and was equal to the higher of two doses examined in OCS-dependent patients (640 and 1,280 [micro]g/d). Treatment guidelines for adults (2,3) recommend high-doses of ICSs (Flovent dose, > 660 [micro]g/d) for severe persistent asthma and low-to-medium doses of ICSs (Flovent dose, 264 to 660 [micro]g/d) for moderate persistent asthma. The FP dose of 880 [micro]g bid is the highest dose that has been approved for use and is recommended for patients with severe asthma who are dependent on OCS. (37) Additionally, it has been shown that at the lower dose range, a CIC dosage of 160 [micro]g qd was shown to have an effect on FE[V.sub.1] that was similar to that of an FP dosage of 88 [micro]g bid. (38)
Assessments of HPA-axis function have been used to evaluate the potential for systemic side effects of ICSs. (9,15,16) The present study evaluated the potential effects of 4 weeks of treatment with CIC on HPA-axis function in patients with moderate-to-severe asthma. The primary evaluation of HPA-axis function in this study was the change in serum cortisol AUC0-24h. The study was statistically powered to detect differences between active treatment groups and the PBO group in terms of the change from baseline in serum cortisol AUC0-24h. The FP CFC-MDI formulation, rather than the FP HFA-MDI formulation, was used as an active comparator. At the time of this study, the FP HFA-MDI formulation was not available in the United States.
Patients receiving CIC, 640 [micro]g/d, CIC, 1,280 [micro]g/d, and FP, 880 [micro]g/d, had mean serum cortisol AUC0-24h levels that were unchanged from baseline (results are within the limits of variability) and were similar to that in the PBO group, while patients treated with high-dose FP (1,760 [micro]g/d) had significantly suppressed serum cortisol AUC0-24h values. The results obtained with low-dose cosyntropin stimulation and 24-h urinary cortisol levels corrected for creatinine showed no statistically significant HPA-axis suppression with any of the active treatments, although high-dose FP was the only treatment that produced a negative mean change from baseline in peak cortisol with the cosyntropin test.
The observed results with CIC were consistent with those of several previous studies (20,35,36,39-41) conducted in healthy subjects as well as in asthmatic subjects that have demonstrated that CIC does not suppress HPA-axis function. In a PBO-controlled crossover study (20) of 12 healthy subjects, CIC, 640 [micro]g/d, administered once daily (AM or PM) or 320 [micro]g twice daily for 7 days, did not change the 24-h serum cortisol profile. In the PBO-controlled crossover study conducted by Derom and coworkers (36) in 26 asthmatic patients, the same daily doses of CIC and FP were administered as in the present study, but for 9 days rather than 4 weeks. None of the doses of CIC suppressed plasma cortisol AUC0-24h or 24-h urinary cortisol levels, whereas both doses of FP suppressed these parameters. No influence on urinary cortisol has been observed following a single dose of CIC, 2,880 [micro]g/d, and the cortisol profile for doses of 400 and 1,600 [micro]g/d for 1 week were equivalent to that for PBO. (42) Moreover, a pooled analysis of CIC at doses of up to 2,880 [micro]g/d in healthy volunteers and patients with asthma showed minimal effects on adrenal function. (31)
The finding that FP, 880 [micro]g/d, did not cause HPA-axis suppression is consistent with those of some previous studies, (40,43) although several studies (9,12,16,24,36,44,45) have demonstrated HPA-axis suppression with this and/or lower doses of FP. In patients with moderate-to-severe asthma, factors such as airflow obstruction and ventilation perfusion mismatch can alter drug deposition in the lungs and change systemic absorption. A reduced airway caliber has been shown to reduce the lung bioavailability of FP (44,46); it is known that the systemic bioavailability of inhaled FP is more than halved in asthmatic patients compared to healthy control subjects. (46) The patient population in this trial consisted of patients with moderate-to-severe asthma, with a mean FE[V.sub.1] percent predicted that ranged from 56.2 to 64.8% at baseline. This phenomenon might also explain the lack of adrenal suppression with the lower dose of FP in the present study.
The suppression of serum cortisol AUC0-24h observed in patients receiving FP, 1,760 [micro]g/d, was expected. This dose is known to cause the suppression of the HPA-axis (13,24,47) and has been used previously in other studies as an active comparator. (24,36) The study by Affrime et al, (24) in which one of the component studies had a similar parallel-group design, compared the effects of FP, 1,760 [micro]g/cl, mometasone furoate, MDI 800 and 1,600 [micro]g/d, and PBO on the HPA axis. Statistically significant suppression of plasma cortisol AUC0-24h was found after the administration of FP, 1,760 [micro]g/d, and mometasone furoate, 1,600 [micro]g/d. A recent study (48) of patients with moderate persistent asthma evaluated the effects of CIC, 1,280 [micro]g/d, and FP, 1,760 [micro]g/d, on the plasma cortisol response to human corticotrophin-releasing factor. Serum cortisol, beth prior to and in response to human corticotrophin-releasing factor, was suppressed from baseline by FP, 1,760 [micro]g/d, in contrast to CIC, 1,280 [micro]g/d, which did not. The overnight 10-h urinary cortisol level was also suppressed by FP, 1,760 [micro]g/d, but not by CIC, 1,280 [micro]g/d.
The dissociation in effects on basal HPA-axis function (assessed by serum cortisol AUC0-24h) and dynamic HPA-axis function (assessed by low-dose cosyntropin stimulation) observed in the present study might be explained by the much longer treatment periods required to produce adrenocortical atrophy and reduced adrenal reserve, whereas the effects on basal adrenocortical secretion can be seen even after single dosing. Similar discordant results have been reported previously for FP and other ICSs. (24,49,50) Additionally, compared to integrated serum cortisol measurements, 24-h urinary cortisol measurements may have greater variability and be less reliable in assessing changes in HPA-axis function. (9,16) However, both the low-dose cosyntropin stimulation and 24-h urinary cortisol measurements are sensitive markers of HPA-axis suppression, and the 1-month duration should have been long enough to produce suppression of the ACTH response. One explanation for this is that while the suppression of serum cortisol AUC0-24h for the higher dose of FP was statistically significant, it may not be clinically relevant if it did not produce a commensurate suppression of the ACTH-stimulated cortisol response.
Previous studies have shown comparable efficacy and potency for CIC and FP in reducing airway responsiveness, and in improving pulmonary function and asthma symptoms. In the PBO-controlled crossover study conducted by Derom and coworkers (36) in 26 asthmatic patients, all doses of CIC (320 [micro]g qd, 640 [micro]g qd, and 640 [micro]g bid) and both doses of FP (440 [micro]g bid and 880 [micro]g bid by CFC-MDI) decreased hyperresponsiveness to adenosine monophosphate, as demonstrated by a more than doubling of the dose yielding a provocative concentration causing a fall of 20% in FE[V.sub.1], although no dose response was demonstrated for any of the two steroids. In a double-blind crossover study (51) conducted in 19 mild-to-moderate asthma patients, there was no significant difference after 4 weeks of treatment with CIC, 320 qd, or FP, 210 [micro]g bid (administered by HFA-MDI), in reducing hyperresponsiveness to methacholine. In another double-blind study, (38) lower doses of CIC (160 [micro]g qd) and FP (HFA-MDI, 88 [micro]g bid) administered for 12 weeks were equally effective in improving FE[V.sub.1], FVC, peak expiratory flow, asthma symptoms, and the use of rescue medication in 529 adult asthma patients having baseline FE[V.sub.1] percent predicted values of 50 to 90% at baseline and not receiving ICSs at baseline.
In summary, these data support the finding that CIC administered at doses of up to 1,280 [micro]g/d does not result in a statistically significant suppression of HPA-axis function in patients with moderate-to-severe asthma. Data from this study also indicate that, compared with PBO, there was a statistically significant adrenal suppression following treatment with FP, 1,760 [micro]g/d, but not FP, 880 [micro]g/d. The absence of the suppression of HPA-axis function with CIC was paralleled by its good tolerability.
ACKNOWLEDGMENT: The authors thank David B. Allen, MD, George Chrousos, MD, Robert Dhuly, MD, and Hershel Raff, PhD, for their assistance in the development of the protocol for this study. The authors also wish to thank Jerry M. Herron, MD and James Williams, MD.
REFERENCES
(1) Sly RM. New guidelines for diagnosis and management of asthma. Ann Allergy Asthma Immunol 1997; 78:427-437
(2) National Asthma Education and Prevention Program. Expert panel report 2: guidelines for the diagnosis and management of asthma. Bethesda, MD: National Heart, Lung, and Blood Institute, 1997; NIH Publication No. 97-4051
(3) National Asthma Education and Prevention Program. Expert panel report: guidelines for the diagnosis and management of asthma; update on selected topics--2002 (EPR-update 2002). J Allergy Clin Immunol 2002; 110(suppl):S141-S219
(4) Barnes PJ, Pederson S. Efficacy and safety of inhaled corticosteroids in asthma: report of a workshop held in Eze, France, October 1992. Am Rev Respir Dis 1993; 148(suppl): S1-S26
(5) Taylor DA, Jensen MW, Kanabar V, et al. A dose-dependent effect of the novel inhaled corticosteroid ciclesonide on airway responsiveness to adenosine-5'-monophosphate in asthmatic patients. Am J Respir Crit Care Med 1999; 160: 237-243
(6) Davies DE, Wicks J, Powell RM, et al. Airway remodeling in asthma: new insights. J Allergy Clin Immunol 2003; 111:215-225
(7) Hamelmann E, Schleimer RP. Corticosteroid treatment in bronchial asthma: for better or for worse? J Allergy Clin Immunol 2003; 111:248-250
(8) Derendorf H. Pharmacokinetic and pharmacodynamic properties of inhaled corticosteroids in relation to efficacy and safety. Respir Med 1997; 91(suppl):22-28
(9) Martin RJ, Szefler SJ, Chinchilli VM, et al. Systemic effect comparisons of six inhaled corticosteroid preparations. Am J Respir Crit Care Med 2002; 165:1377-1383
(10) Brus R. Effects of high-dose inhaled corticosteroids on plasma cortisol concentrations in healthy adults. Arch Intern Med 1999; 159:1903-1908
(11) Lipworth BJ, Jackson CM. Safety of inhaled and intranasal corticosteroids: lessons for the new millennium. Drug Saf 2000; 23:11-33
(12) Szefler SJ, Martin RJ, King TS, et al. Significant variability in response to inhaled corticosteroids for persistent asthma. J Allergy Clin Immunol 2002; 109:410-418
(13) Lipworth BJ. Systemic adverse effects of inhaled corticosteroid therapy: a systemic review and meta-analysis. Arch Intern Med 1999; 159:941-955
(14) Allen DB, Bielory L, Derendorf H, et al. Inhaled corticosteroids: past lessons and future issues. J Allergy Clin Immunol 2003; 112(suppl):S1-S40
(15) Lipworth BJ, Seckl JR. Measures for detecting systemic bioactivity with inhaled and intranasal corticosteroids. Thorax 1997; 52:476-582
(16) Nelson HS, Stricker W, Casale TB, et al. A comparison of methods for assessing hypothalamic-pituitary-adrenal (HPA) axis activity in asthma patients treated with inhaled corticosteroids. J Clin Pharmacol 2002; 42:319-326
(17) Ciclesonide: BY 9010, ciclesonide-DPI, ciclesonide-MDI, EL 876. Drugs R D 2002; 3:407-410
(18) Dent G. Ciclesonide (Byk Gulden). Curr Opin Investig Drugs 2002; 3:78-83
(19) Kanniess F, Richter K, Bohme S, et al. Effect of inhaled ciclesonide on airway responsiveness to inhaled AMP, the composition of induced sputum and exhaled nitric oxide in patients with mild asthma. Pulm Pharmacol Ther 2001; 14:141-147
(20) Weinbrenner A, Huneke D, Zschiesche M, et al. Circadian rhythm of serum cortisol after repeated inhalation of the new topical steroid ciclesonide. J Clin Endocrinol Metab 2002; 87:2160-2163
(21) Reynolds NA, Scott LJ. Ciclesonide. Drugs 2004; 64:511-519
(22) Rohatagi S, Derendorf H, Zech K et al. PK/PD of inhaled cortidosteroids: the risk/benefit of inhaled ciclesonide. J Allergy Clin Immunol 2003; 111:A598
(23) Drollmann A, Hasselquist BE, Boudreau RJ, et al. Ciclesonide shows high lung deposition in 2D and 3D-imaging. Am J Respir Crit Care Med 2002; 165:A188
(24) Affrime MB, Kosoglou T, Thonoor CM, et al. Mometasone furoate has minimal effects on the hypothalamic-pituitary-adrenal axis when delivered at high doses. Chest 2000; 118:1538-1546
(25) Seidegard J, Simonsson M, Edsbacker S. Effect of an oral contraceptive on the plasma levels of budesonide and prednisolone and the influence on plasma cortisol. Clin Pharmacol Ther 2000; 67:373-381
(26) Bethke TD, Boudreau RJ, Hasselquist BE, et al. High lung deposition of ciclesonide in 2D and 3D imaging. Eur Respir J 2002; 20(suppl):s109
(27) Dietzel K, Engelstatter R, Keller A. Ciclesonide: an on-site-activated steroid. Prog Respir Res 2001; 31:91-93
(28) Richter K, Kanniess F, Biberger C, et al. Comparison of the oropharyngeal deposition of inhaled ciclesonide and fluticasone propionate in patients with asthma. J Clin Pharmacol 2005; 45:146-152
(29) Kaliner M, Rohatagi S, Zech K, et al. The receptor binding of ciclesonide: comparison to other inhaled corticosteroids. Ann Allergy Asthma Immunol 2003; 90:129-130
(30) Nave R, Meyer W, Fuhst R, et al. Formation of fatty acid conjugates of ciclesonide active metabolite in the rat lung after 4-week inhalation of cicleosonide. Pulmon Pharmacol Therap available online April 27, 2005
(31) Rohatagi S, Arya V, Zech K, et al. Population pharmacokinetics and pharmacodynamics of ciclesonide. J Clin Pharmacol 2003; 43:365-378
(32) Nave R, Bethke TD, Van Marle SP, et al. Pharmacokinetics of [14C]ciclesonide after oral and intravenous administration to healthy subjects. Clin Pharmacokinet 2004; 43:479-486
(33) Chapman KR, Patel P, D'Urzo AD, et al. Maintenance of asthma control by once-daily inhaled cicleosonide in adults with persistent asthma. Allergy 2005; 60(3): 330-337
(34) Engelstatter R, Langdon C, Bethke T, et al. Efficacy of ciclesonide after 12-week treatment of bronchial asthma. Am J Respir Crit Care Med 2002; 165:A766
(35) O'Connor BJ, Kilfeather S, Cheung D, et al. Treatment of moderate to severe asthma with ciclesonide: a long-term investigation over 52 weeks. Eur Respir J 2002; 20(suppl): S406
(36) Derom E, Van De Velde V, Marissens S, et al. Effects of inhaled ciclesonide and fluticasone propionate on cortisol secretion and airway responsiveness to adenosine 5'monophosphate in asthmatic patients. Pulm Pharmacol Ther 2005; 18:328-336
(37) GlaxoSmithKline. Flovent prescribing information. In: Physicians' desk reference. Montvale, NJ: Medical Economics Company, 2003; 1523-1526
(38) Buhl R, Vinkler I, Magyar P, et al. Once daily ciclesonide and twice daily fluticasone propionate are equally effective in the treatment of patients with asthma. Am J Respir Crit Care Med 2004; 169:A91
(39) Kerwin E, Chervinsky P, Fish J, et al. Ciclesonide has no effect on hypothalamic-pituitary-adrenal (HPA)-axis at once-daily doses of 80 [micro]g, 160 [micro]g or 320 [micro]g in the treatment of patients with mild-to-moderate asthma. Am J Respir Crit Care Med 2004; 169:A90
(40) Lipworth BJ, Kaliner MA, LaForce CF et al. Effect of ciclesonide and fluticasone on hypothalamic-pituitary-adrenal axis function in adults with mild-to-moderate persistent asthma. Annals Allergy Asthma Immunol 2005; 94:465-472
(41) Kaliner M, White M, Chervinsky P, et al. Ciclesonide, a novel inhaled corticosteroid (ICS), does not suppress hypothalamic-pituitary-adrenal (HPA)-axis function [abstract]. Allergy Clin Immunol Int 2003; (suppl):O-17-1
(42) Aventis Pharmaceuticals. Study BY9010/FHP009: safety, tolerability and pharmacodynamics of the new topical steroid ciclesonide in healthy male volunteers following ascending single dose and repeated dose inhalations over 7 days. Bridgewater, NJ: Aventis Pharmaceuticals, 1998; Report No. 117E/97
(43) Chervinsky P, van As A, Bronsky EA, et al. Fluticasone propionate aerosol for the treatment of adults with mild to moderate asthma: the Fluticasone Propionate Asthma Study Group. J Allergy Clin Immunol 1994; 94:676-683
(44) Weiner P, Berar-Yanay N, Davidovich A, et al. Nocturnal cortisol secretion in asthmatic patients after inhalation of fluticasone propionate. Chest 1999; 116:931-934
(45) Fowler SJ, Orr LC, Wilson AM, et al. Dose-response for adrenal suppression with hydrofluoroalkane formulations of fluticasone propionate and beclomethasone dipropionate. Br J Clin Pharmacol 2001; 52:93-95
(46) Brutsche M, Brutsche IC, Munawar M, et al. Comparison of pharmacokinetics and systemic effects of inhaled fluticasone propionate in patients with asthma and healthy volunteers: a randomized crossover study. Lancet 2000; 356:556-561
(47) Wilson AM, Lipworth BJ. 24 hour and fractionated profiles of adrenocortical activity in asthmatic patients receiving inhaled and intranasal corticosteroids. Thorax 1999; 54:20-26
(48) Lee DK, Fardon TC, Bates CE, et al. Airway and systemic effects of hydrofluoroalkane formulations of high dose eiclesonide and fluticasone in moderate persistent asthma. Chest 2005; 127:851-860
(49) Clark DJ, Grove A, Cargill RI, et al. Comparative adrenal suppression with inhaled budesonide and fluticasone propionate in adult asthmatic patients. Thorax 1996; 51:262-266
(50) Wilson AM, McFarlane LC, Lipworth BJ. Effects of low and high doses of inhaled flunisolide and triamcinolone acetonide on basal and dynamic measures of adrenocortical activity in healthy volunteers. J Clin Endocrinol Metab 1998; 83:922-925
(51) Lee DKC, Haggart K, Currie GP, et al. Effects of hydrofluoroalkane formulations of ciclesonide 400 [micro]g once daily vs fluticasone 250 [micro]g twice daily on methacholine hyper-responsiveness in mild-to-moderate persistent asthma. Br J Clin Pharmacol 2004; 58:26-33
* From the National Jewish Medical & Research Center (Dr. Szefler), Denver, CO; and Aventis Pharmaceuticals, a member of the Sanofi-Aventis Group (Drs. Rohatagi, Kundu, and Banerji, and Mr. Lloyd), Bridgewater, NJ.
This study was supported by Aventis Pharmaceuticals, a member of the Sanofi-Aventis Group (Bridgewater, NJ) and ALTANA Pharma.
Manuscript received August 26, 2004; revision accepted February 1, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Stanley J. Szefler, MD, National Jewish Medical & Research Center, 1400 Jackson St, Room J313, Denver, CO 80206; e-mail: szeflers@njc.org
Placebo
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group