For most patients, asthma is not controlled as defined by guidelines; whether this is achievable has not been prospectively studied. A 1-year, randomized, stratified, double-blind, parallel-group study of 3,421 patients with uncontrolled asthma compared fluticasone propionate and salmeterol/fluticasone in achieving two rigorous, composite, guideline-based measures of control: totally and well-controlled asthma. Treatment was stepped-up until total control was achieved (or maximum 500 µg corticosteroid twice a day). Significantly more patients in each stratum (previously corticosteroid-free, low- and moderate-dose corticosteroid users) achieved control with salmeterol/fluticasone than fluticasone. Total control was achieved across all strata: 520 (31%) versus 326 (19%) patients after dose escalation (p
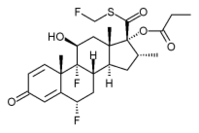
Keywords: antiasthmatic agents; fluticasone propionate; guidelines; quality of life; salmeterol
The goal of asthma management is to achieve and maintain control of the disease without side effects from the therapies used (1-3). Large, multinational, community-based surveys of asthma have shown, however, that the majority of patients have an alarmingly high rate of symptoms and disruption of life from their disease, indicating that this goal is not being achieved (4-6). As a result, some have suggested that asthma control, as defined in guidelines, is unrealistic for the "vast majority" of patients (7). If this conclusion is correct, it is necessary to consider whether this shortcoming is caused by the refractory nature of the disease, limitations of current treatments, or a problem of treatment strategies, coupled with low physician and patient expectations and treatment compliance (8). Surprisingly, most clinical studies assessing the efficacy of "controller" therapies in asthma do not address whether control was achieved but rather focus on improvements in individual end points obtained with fixed doses of treatment. Assessment of individual asthma end points alone, such as lung function, may overestimate the level of asthma control achieved (9). Furthermore, such limited end points may not reflect what is important to the patient, whose quality of life is more dependent on the overall impact of the disease rather than on a single measure (10). To date, no studies have assessed the benefits of aiming for complete, comprehensive, and sustained clinical control in a controlled study that allows for dose escalation, as necessary, to achieve this. As a result, the full efficacy potential or limitations of current treatments have not been formally evaluated. We therefore conducted a 1-year prospective trial, Gaining Optimal Asthma controL (GOAL), to compare the efficacy of two recommended controller therapies: an increasing dose of fluticasone propionate alone or in combination with the long-acting β^sub 2^-agonist salmeterol to achieve asthma control as defined in the Global Initiative for Asthma/National Institutes of Health guidelines (3, 11). Some of the results of this study have been previously reported in abstract form (12-27).
METHODS
Study Design and Assessment of Asthma Control
GOAL was a 1-year, stratified, randomized, double-blind, parallel-group study comparing the efficacy and safety of individual, predefined, stepwise increases of salmeterol/fluticasone propionate (salmeterol/fluticasone; Seretide/Advair; GlaxoSmithKline, Middlesex, UK) with fluticasone propionate (fluticasone; Flixotide/Flovent; GlaxoSmithKline) alone in achieving two predefined composite measures of asthma control.
The definitions of control were derived from the treatment goals of the Global Initiative for Asthma/National Institutes of Health guidelines (3, 11): "totally controlled" or "well controlled" or uncontrolled (if neither definition was fulfilled). Both control definitions were composite measures that included the following asthma outcomes: PEF, rescue medication use, symptoms, night-time awakenings, exacerbations, emergency visits, and adverse events (Table 1). Equal weighting was given to each criterion. Totally controlled and well-controlled weeks were defined by achievement of all of the specified criteria for that week. Totally controlled asthma was achieved if the patient, during the 8 consecutive assessment weeks, recorded 7 totally controlled weeks and had no exacerbations, emergency room criteria, or medication-related adverse event criteria for each day of each week. Well-controlled asthma was achieved if the patient recorded 7 of 8 well-controlled weeks, and failure to achieve any one of these would result in failure to achieve control for that week. Failure of the exacerbation, emergency visit, or adverse event criteria resulted in the automatic failure of control status (totally and well-controlled definitions) for the entire 8-week period, irrespective of how well asthma was controlled at other time points during the 8 weeks. Well-controlled asthma was similarly assessed over 8 weeks but was allowed a low level of symptoms and rescue medication use, as outlined in Table 1.
During the run-in period, patients continued on their usual dose (if any) of inhaled corticosteroid treatment. Those who did not achieve at least two well-controlled weeks in the 4-week run-in period were randomized to one of three strata based on their inhaled corticosteroid dose during the 6 months before screening: stratum 1, no inhaled corticosteroid; stratum 2, 500 µg or less of beclomethasone dipropionate daily or equivalent; or stratum 3, more than 500 to 1,000 µg or less of beclomethasone dipropionate daily or equivalent (see Figure E1 in the online supplement).
During phase I, the dose escalation phase, treatment was "stepped up" every 12 weeks until totally controlled asthma was achieved or the highest dose of study drug reached (salmeterol/fluticasone 50/500 µg twice a day or fluticasone 500 µg twice a day). In strata 1 and 2, there were a maximum of three treatment steps: salmeterol/fluticasone 50/ 100, 50/250, 50/500 µg twice a day or fluticasone 100, 250, 500 µg twice a day. In stratum 3, there were up to two treatment steps: salmeterol/ fluticasone 50/250, 50/500 µg twice a day or fluticasone 250, 500 µg twice a day.
Patients entered phase II either after achieving totally controlled asthma or after 12 weeks on the maximum dose of study medication. During phase II, patients remained on the dose at which they achieved totally controlled asthma or the maximum dose of study medication until the end of the 1-year double-blind treatment period. To assess the potential incremental effect of time on attainment of control, particularly in those not achieving the target level of totally controlled asthma, no stepdown in treatment was performed during phase II.
Patients who failed to achieve totally controlled asthma in phase 1 were reassessed at the end of phase II (Weeks 44-52). Those that still had not achieved totally controlled asthma at this time entered a 4-week, open-label phase during which all patients, regardless of initial randomization, were given oral prednisolone (0.5 mg/kg up to 60 mg/day for 10 days) and salmeterol/fluticasone 50/500 µg twice a day for 4 weeks.
Patients
Patients recruited by investigators from general practice and hospital clinics were 12 years old or more and less than 80 years old with at least a 6-month history of asthma, a demonstrated improvement in FEV^sub 1^ of 15% or more (and ≥ 200 ml) after inhalation of a short-acting β^sub 2^-agonist documented within the previous 6 months or as assessed during run-in, a smoking history of less than 10 pack-years, and no use of long-acting inhaled or oral β^sub 2^-agonists within the previous 2 weeks. The study was approved by local research ethics committees, and all patients or their guardians gave written informed consent.
Outcomes
Control was assessed over an 8-week period before each clinic visit at Weeks 12, 24, 36, and 52. The primary objective was to determine the proportion of patients who achieved well-controlled asthma with salmeterol/fluticasone combination compared with fluticasone alone during phase I. Additional end points included the cumulative proportion of patients achieving control in phase II, the dose of inhaled corticosteroid and time required to achieve the first well-controlled week; proportion of patients and dose to achieve totally controlled asthma; the time to achieve the first totally controlled week; asthma quality of life (using the Asthma Quality of Life Questionnaire [AQLQ]) (28); the rate of exacerbations (requiring oral corticosteroids, hospitalisations or emergency visits); and morning predose clinic FEV^sub 1^. Adverse event information was collected at each clinic visit, and 24-hour urinary cortisols were collected in all patients attending study centers in the United States and Canada. Information on study design and analysis of results is provided in the online supplement.
RESULTS
Subject Characteristics
A total of 5,068 patients from 326 centers in 44 countries were screened: 3,421 qualified for inclusion. Baseline characteristics of the intention-to-treat population (3,416) were comparable between treatment groups within each stratum (Table 2 and Table E1 of the online supplement). A total of 3,039 patients completed phase I, and 2,890 completed phase II. Reasons for withdrawal from each phase were adverse events (57 and 17 patients in phases I and II, respectively), consent withdrawn (81 and 30), lost to follow-up (74 and 37), asthma exacerbation (10 and 3), ineligible for the study, protocol violation, or unevaluable data (98 and 19), and other (57 and 43). Of the 1,659 patients who had not achieved totally controlled asthma in either phase I or phase II and were therefore eligible for the 4-week open-label phase, 157 were withdrawn before entry, and 22 were withdrawn during the 4 weeks. Reasons for withdrawal were adverse events (3 and 4 patients before or during the 4 weeks, respectively), consent withdrawn (6 and 2), lost to follow-up (3 and 8), protocol violation or unevaluable data (15 and 3), and other (130 and 5), which included a reluctance to take oral corticosteroids (see Figure E2 of the online supplement). Compliance (the proportion of patients who used ≥ 80% of study medication, as assessed using the dose counter on the Diskus/ Accuhaler; GlaxoSmithKline) during the blinded phases was 89% for both treatment groups.
Effect of Treatment on Achievement of Guideline-defined Asthma Control
For all strata, the proportion of patients who achieved well-controlled and totally controlled asthma at the end of phase 1 of the study was significantly greater for salmeterol/fluticasone compared with fluticasone. Well-controlled asthma was achieved in 71% and 65% of patients for salmeterol/fluticasone and fluticasone, respectively, in stratum 1 (odds ratio [OR], 1.32; 95% confidence interval [CI], 1.01-1.73; p = 0.039), 69% and 52% in stratum 2 (OR, 2.13; 95% CI, 1.65-2.74; p
In phase I, totally controlled asthma was achieved in 42% and 31% of patients for salmeterol/fluticasone and fluticasone, respectively, in stratum 1 (OR, 1.71; 95% CI, 1.30-2.24; p
In each stratum, the proportion of patients achieving control at the same or a lower dose of inhaled corticosteroid was greater for those treated with salmeterol/fluticasone. A similar number of patients were able to achieve control with the lowest dose of salmeterol/fluticasone compared with up to 250 µg of fluticasone alone (Figures 1A and 1B). The odds of achieving well-controlled and totally controlled asthma at the same or lower dose of inhaled corticosteroid for salmeterol/fluticasone versus fluticasone in stratum 1 increased by at least 40% (well controlled: OR, 1.40; 95% CI, 1.12-1.76; p = 0.003; totally controlled: OR, 1.78; 95% CI, 1.38-2.30; p
Analysis of time to asthma control, defined as the time to the first well-controlled week or totally controlled week during Weeks 1-12, showed that control was achieved significantly faster with salmeterol/fluticasone compared with fluticasone alone (all strata p ≤ 0.002). The week by which 50% of patients achieved their first well-controlled week was Week 3 versus Week 4 for salmeterol/fluticasone and fluticasone, respectively, in stratum 1, Week 2 versus Week 7 in stratum 2, and Week 5 versus Week 10 in stratum 3 (all p
Longitudinal Effect of Treatment on Achieving Guideline-defined Asthma Control
During the constant dose phase (phase II), additional patients achieved both well-controlled and totally controlled asthma (Figures 1A and 1B). The cumulative proportion of patients achieving well-controlled asthma at the end of phase II were as follows: stratum 1, 78% on salmeterol/fluticasone and 70% on fluticasone (p = 0.003); stratum 2, 75% and 60%, respectively (p
Figure 2 shows the proportion of patients (noncumulative) who achieved well-controlled asthma status for a single week (a well-controlled week) in each week of the study. This increased progressively during the study and reached 1,142 (77%) for salmeterol/fluticasone and 966 (68%) for fluticasone across all strata.
Effect of Oral Corticosteroids and High-dose Combination Therapy in Patients not Totally Controlled at the End of the Study
An additional 40 (7%), 52 (9%), and 59 (10%) patients of those previously on fluticasone alone who had not achieved well controlled asthma in phase 1 or phase II achieved it during the maximum treatment phase with oral corticosteroids plus salmeterol/fluticasone 50/500 (in strata 1-3, respectively). Similarly, an additional 35 (6%), 54 (9%), and 63 (11%) patients who had not achieved totally controlled asthma in phase I or phase II achieved it during the maximum treatment phase. Of those patients previously on salmeterol/fluticasone, an additional 25 (5%), 23 (4%), and 39 (7%) patients achieved well-controlled status, and 25 (5%), 37 (6%), and 31 (5%) achieved totally controlled asthma with the addition of oral corticosteroids in strata 1-3, respectively.
Effect of Treatments on Exacerbations
The mean annual rates of exacerbations requiring oral corticosteroids and/or hospitalization or emergency visits were low in both treatment groups but were significantly lower in the salmeterol/fluticasone group in each stratum (p ≤ 0.009) (Figure 3). In all strata, there was a consistent trend for a reduction in the annualized rate of exacerbations in phase II compared with the exacerbation rates in phase I (see online supplement Figure E3). This was seen even when allowing for patients who had withdrawn during the study. For patients achieving totally controlled and well-controlled asthma in phase I, the annualized exacerbation rates in phase II were 0.05 and 0.13, respectively; in contrast, the annualized exacerbation rate for those not achieving at least well-controlled asthma was 0.23 (all strata, both treatments combined).
Effect of Treatments on Asthma Quality of Life
Overall AQLQ scores improved in both groups throughout the study, with a statistically significant difference in favor of salmeterol/fluticasone in strata 2 and 3 (Table 3). The proportion of patients who achieved near-maximal mean overall AQLQ scores (≥ 6) increased from 6-10% at baseline to 62% versus 62% (salmeterol/fluticasone versus fluticasone) in stratum 1; 64% versus 53% in stratum 2; and 57% versus 45% in stratum 3 at Week 52. There was a trend for higher quality of life scores in patients who gained control. Achieving totally controlled and well-controlled asthma in phase I was associated with mean overall AQLQ scores of 6.4 and 6.1, respectively, in phase II; in contrast, the mean overall AQLQ score for those not achieving at least well-controlled asthma was 5.3 (all strata, both treatments combined).
Effect of Treatments on FEV^sub 1^ Values
The mean morning prebronchodilator FEV^sub 1^ increased in both groups, with significantly larger improvements in the salmeterol/ fluticasone group (Table 3). For patients achieving totally controlled and well-controlled asthma in phase I, the percentage predicted FEV^sub 1^ at phase II endpoints were 94% and 87%, respectively; for those not achieving at least well-controlled asthma, the percentage predicted FEV^sub 1^ was 82% (all strata, both treatments combined).
Adverse Events and Urinary Cortisol
Serious adverse events were observed during the double-blind period in 4% and 3% of patients in the salmeterol/fluticasone and fluticasone arms, respectively. The most common serious adverse events (not necessarily related to treatment) across all strata were asthma, occurring in 8 (
DISCUSSION
Our results demonstrate that in the majority of patients with uncontrolled asthma across a wide range of severities, comprehensive guideline-defined control can be achieved and maintained. More patients achieved both totally controlled and well-controlled asthma with combination inhaled salmeterol/fluticasone more rapidly and at a lower dose of corticosteroid than with inhaled fluticasone alone. Patients that achieved control recorded very low rates of exacerbations and near-maximal health status scores. Furthermore, in stepping up treatment in an attempt to achieve guideline-defined total control, even those patients who did not attain our stringent definitions of control showed considerable improvements in health status and a reduction in exacerbation rates. The overall AQLQ score for all groups and strata approached or surpassed the value of 6, suggesting that asthma no longer had a significant impact on quality of life, and AQLQ scores were higher for salmeterol/fluticasone than for fluticasone (10, 28). A greater degree of improvement was also seen in lung function; morning FEV^sub 1^ improved to within a range considered normal. The absence of a reference group prevents a formal assessment of the improvement in these measures, but compared with rates and measures recorded before study entry, the improvements appear substantial, with a consistent trend for further improvement in the maintenance dose phase.
Because no widely accepted measures of asthma control were available, two composite measures from the Global Initiative for Asthma/National Institutes of Health guideline goals of treatment were developed and proposed as targets for control. As single measures are likely to overestimate control, a composite measure was selected to assess the total impact of this disease on patients (9). Totally controlled asthma was the complete absence of all features of asthma for at least 7 of 8 weeks. Well controlled was a pragmatic adaptation based on what is permitted by the guidelines as control, also sustained for at least 7 of 8 weeks. Such stringent and sustained measures of asthma control have never previously been assessed in a clinical trial. The results of our study suggest that total control should be the aim of treatment for all asthma patients. It is a realistic outcome for corticosteroid-naïve patients, and although it may not be achieved by the majority of patients previously on moderate or high doses of inhaled corticosteroids, by stepping up treatment and aiming for total control of asthma, considerable benefits are achieved in almost all patients. This is particularly true for exacerbations, which were virtually eliminated in patients who achieved guideline-defined control (either total control or well controlled).
Because the focus of this study was to establish the proportion of patients with asthma that could achieve the target level of control, even if this took several months, the approach adopted was to continue treatment for the full duration of the trial and not step-down, as recommended in the guidelines. This also permitted evaluation of incremental benefit (in secondary outcomes), both in those that reached this level and those that did not. During sustained treatment, a further 8 to 12% achieved totally controlled asthma, and further improvements in FEV^sub 1^, exacerbation rates, and quality of life were observed, particularly in those that attained totally controlled asthma. This delayed realization of the full benefits of treatment may reflect a more gradual resolution of the airway inflammation with prolonged dosing (29, 30). This effect is suggested by the results of the open-label phase in which relatively few patients benefited from the additional "maximum" treatment with 10 days of high-dose oral corticosteroid and 4 weeks of salmeterol/fluticasone 50/500 µg twice a day. Those who showed a response in this phase were predominantly patients who had not previously received salmeterol/fluticasone. This finding suggests that the treatments and dosing approach had achieved as much as, or close to maximum benefit, at least as far as clinical total control is concerned. However, it must be recognized that some of the reasons for nonattainment of this level were technical (such as patients with missing data) and potentially diagnostic errors. In addition, the target threshold value for PEF of 80% of predicted used in the definition of control was a pragmatic interpretation of the Global Initiative for Asthma goal of achieving "normal or near-normal" lung function and for some patients might have been unduly strict. Even among those that failed to achieve the prescribed definitions of control, clinical benefit was considerable, as judged by the group mean data of individual end points, such as lung function and health status. Because for ethical reasons the study was not placebo controlled, the potential placebo effect of participation in a study on attainment of asthma control (resulting, e.g., from improved adherence to treatment) cannot be evaluated. This would not be expected to affect treatment comparisons. Further analysis of factors that might potentially be associated with no-attainment of asthma control, such as cigarette smoking history (31, 32), age, atopy, sex, and duration of asthma is required.
The greater benefit of the salmeterol/fluticasone combination over inhaled fluticasone alone is consistent with the results of many clinical trials (33, 34), but this is the first study to demonstrate its advantage in achieving comprehensive sustained asthma control. Differences between treatments were apparent for each end point: the number that achieved control, the dose of corticosteroid at which control was achieved, and the time to first control week. In addition, salmeterol/fluticasone was more effective than fluticasone in achieving improvement in all secondary end points, irrespective of whether patients achieved the predefined levels of control. The greater improvements noted with salmeterol/ fluticasone over fluticasone alone were maintained over the duration of the trial with no evidence of the fluticasone alone group "catching up." Such results further confirm the benefits of the addition of salmeterol to inhaled corticosteroids. These differences in treatment effect were consistently seen across all levels of baseline therapy, even those patients entering the study as corticosteroid-naïve or corticosteroid-free. The greater efficacy of combination therapy in patients who were corticosteroid-naïve contrasts with a previous report in which little additional benefit was found with the addition of the long-acting β^sub 2^-agonist formoterol to the inhaled corticosteroid budesonide in subjects who were corticosteroid-naïve with mild disease (35). This difference may be accounted for by differences in patient selection (with OPTIMA recruiting patients with very mild asthma), treatment approach (as treatments were stepped up, if required, in GOAL as opposed to using fixed doses), and outcome selection (with GOAL using a rigorous composite measure).
Application of these findings to the management of patients with asthma in general is strengthened by the large size of this study, which involved subjects over a wide range of age, geographic location, ethnicity, and baseline treatment. The requirement for reversibility of at least 15% was to ensure that patients with asthma were selected, as is generally required in asthma treatment trials. It is recognized that this may limit the applicability of the results to patients who do not demonstrate this characteristic feature. The high median reversibility obtained likely reflects the fact that short-acting β^sub 2^-agonists were withheld for at least 6 hours before reversibility testing and patients were on no other bronchodilators. Furthermore, the aim of recruitment was to enroll patients who had failed to achieve guideline-defined control; evidence from recent surveys has shown that over 95% of patients with asthma failed to achieve this (6). A surprising feature was the similarity of baseline characteristics across the strata. This may be explained by the fact that only patients with uncontrolled asthma were recruited, and patients with different levels of severity might tolerate similar levels of symptoms and take just enough treatment to maintain themselves at that level (6, 8, 36).
Treatment guidelines recommend either a stepwise increase in treatment or starting with a high dose and then stepping down once control is achieved. A stepwise increase in treatment was used for all three strata. While the aim of this study was not to compare the stepwise approach to the high-dose approach, in each stratum, it was observed that between 40% and 53% of patients reached totally controlled asthma at the lowest dose of inhaled fluticasone when used in combination with salmeterol. Similarly, no attempt was made to step down treatment once control was achieved, as proposed in treatment guidelines. This aspect of treatment, although widely used, has not been well researched.
A study by Reddel and colleagues (30) has shown that reliever use, airway hyperresponsiveness, and overall asthma control (though less stringently defined than in GOAL) continued to improve during inhaled corticosteroid down titration. The results from our study suggest that additional benefit may be derived from sustaining regular treatment for up to 6 to 9 months (the duration of the trial) without stepping down; however, the absence of control arms employing step-down routines in GOAL prevents conclusions about whether this is an effect of prolonged treatment or of sustained dose. Further studies are required.
As the aim of treatment in this study was total control, it called for step up of treatment even though patients had become "well controlled." For this reason, a majority ended the study on the highest dose of treatment (68% of patients on salmeterol/ fluticasone and 76% of patients on fluticasone; all strata). Because the dose-response relationship for inhaled corticosteroids in asthma is relatively flat, the benefits of increasing the dose relative to risk diminish as the dose is increased. In relationship to benefit, the sustained treatment at higher doses enabled more patients to achieve the goal. However, there was also potential for additional adverse effects, particularly because the treatment was not stepped down once control was achieved. It is therefore significant that the overall frequency and nature of self-reported adverse events were similar to most other trials involving inhaled corticosteroids in asthma and predominantly affected the upper respiratory tract (33, 34, 37). In clinical practice, the decision on whether to aim for total control in patients who have reached a lesser level of control when this involves doubling the dose of controller treatment will need to be made on an individual basis in consultation with the patient.
One strategy for minimizing the risk of adverse effects is to step down treatment when the desired level of control is achieved. Although recommended in guidelines (1, 2), step down has not been extensively studied and is largely based on expert opinion. In this study, treatment was sustained at a constant dose throughout phase II to assess whether control could be maintained, and the study did not attempt to address the matter of step down. Sustained treatment carries the risk of other long-term effects that might take years to become significant. These include adrenocortical suppression and reduced bone mineral density. The doses of inhaled corticosteroids used in this study were those for which registration has been obtained and for which extensive safety data are available. For this reason, examination of these effects was restricted to a comparison of 24-hour urinary cortisol levels (a sensitive indicator of suppression) in a subset of patients. Interpretation of these results needs to consider a number of study design variables, including the corticosteroid dose on study entry and treatment duration at each dose. Consistent with other studies (38, 39) with fluticasone at similar doses, lowering of mean levels of 24-urinary cortisol was evident, but the values remained within or above the normal range in most patients (92%). There was also no difference between treatments, in spite of the larger number of patients in the salmeterol/fluticasone group that did not require the highest dose. Taken together, these results confirm an effect of inhaled corticosteroids on the hypothalamic-pituitary-adrenal axis, but in none was this associated with clinical evidence of adrenal suppression.
The recommendation that total control should be the aim of management for all patients with persistent asthma is based on the fact that, as demonstrated in this study, it is achievable in a considerable proportion of patients (41%; all strata) and that it is associated not only with the greatest improvement in usual asthma end points but also results in a majority of patients achieving health status that approaches complete freedom from the impact of asthma (asthmatic but without asthma). Additionally, asthma exacerbations are reduced to levels that are arguably as low as might be expected. As a treatment strategy, aiming at total control brings asthma management in line with approaches used in other chronic diseases, for example, sustained glycemic control in diabetes or ideal blood pressure in hypertension. This may serve to raise the expectations of patients and physicians and help to address the problem of the relatively poor level of care and of asthma control currently being experienced by patients with asthma worldwide (4-6).
In summary, this study has shown that guideline-defined control of asthma can be achieved in the majority of patients with uncontrolled asthma with combination salmeterol/fluticasone treatment. This approach should be the preferred treatment selection for patients whose asthma is uncontrolled, regardless of their previous inhaled corticosteroid regimen. Salmeterol/fluticasone achieves sustained control of asthma as defined by a composite of relevant clinical goals of treatment in more patients, more rapidly and at a lower dose of inhaled corticosteroids than fluticasone alone. In addition, the approach of aiming for total control and maintaining treatment resulted in the virtual elimination of exacerbations and near-normal quality of life in the majority of patients and brought substantial benefit even to those who failed to achieve this high level of control.
Conflict of Interest Statement: E.D.B. has received honoraria for speaking at scientific meetings and courses financed by AstraZeneca in 2003 and GlaxoSmithKline (GSK) in 2002 and 2003 and has served on Advisory Boards for AstraZeneca, Boehringer Ingelheim and GSK; H.A.B. has received the following payments from GSK ($1,399 in 2004 for speaking at an Advisory Board meeting and $7,000 in 2003 for chairing and lecturing in a Master Class and at a speakers summit), and as per University of California at San Francisco policy, consulting fees are paid to his department; J.B. has been reimbursed by GSK for attending several conferences as a speaker and received a total honorarium of euro13,000 for the past 3 years and has been a member of the GSK Advisory Board and received a total honorarium of euro13,000 for 2001 and 2002; W.W.B. has received consultancy fees for the past 3 years from the following companies with a total consultancy fee for these 3 years for Bristol-Myers Squibb ($2,000), Dynavax ($3,000), Hoffman La Roche ($2,000), Schering ($3,000 for 2002-2003), and Fujisawa ($3,000) and has also served on Advisory Boards in various capacities over the past three years (2001-2003) with the following reimbursements for GSK ($8,500), Aventis ($2,000), Schering ($4,000), Pfizer ($4,000 for 2004), and AstraZeneca ($2,000) and has also received honorarium for speaking or other educational activities in the past 3 years from Merck ($7,000 for 2003), GSK ($2,500 for 2003), and Aventis ($2,500 for 2003) and has received industry-sponsored support for research from GSK ($750,000 for 2002 and 2003) and for participation in multicenter trials for Fujisawa ($250,000 for 2002 and 2003), GSK ($500,000 for 2001-2003), Aventis ($2000,000 for 2001-2003), Hoffman LaRoche ($120,000 for 2002), Pfizer ($100,000 for 2003), Genetech/Novartis ($100,000 for 2002 and 2003), and Merck ($100,000 for 2003); T.J.H.C. has received more than $10,000 per annum over the past 3 years to cover serving as a consultant to GSK as well as serving on advisory boards and giving lectures and has also participated as a speaker at scientific meetings organized and financed by AstraZeneca and Merck, Sharp, and Dohme; R.A.P. has received money from various pharmaceutical companies for serving as a consultant for Almirall Prodesfarma ($10,000 in 2003), Altana ($10,000 in 2002), AstraZeneca ($10,000 in 2003, $10,000 in 2002, $10,000 in 2001), Boehringer lngelheim ($10,000 in 2003, $10,000 in 2002, $10,000 in 2001), GSK ($10,000 in 2003, $10,000 in 2002, $10,000 in 2001), Schering Plough ($10,000 in 2001); S.E.P. has received euro13,000 in 2001 and euro12,000 in 2002 for speaking at scientific meetings or courses organized and financed by AstraZeneca and euro8,000 in 2001 and euro10,000 in 2002 for speaking at scientific meetings or courses organized and financed by GSK. The Regents of the University of California has received payments from GlaxoSmithKline of $485,000 for research conducted under Homer Boushey's direction between 1999 and 2001 and made unrestricted gifts for research and training of $8,323 in 2002 and $4,500 in 2003 and $2,371 in 2004 and GSK also paid $7,390 to the Regents of the University of California for Homer Boushey's service on the Scientific Advisory Board for this study. The University of Denmark has received unrestricted grants from AstraZeneca (euro14,000 in 2001) and GSK (euro120,000 in 2001, 2002, and 2003).
Acknowledgment: The authors acknowledge the contribution of Professor Ann Woolcock who assisted with the study design. They thank the investigators and staff at all study sites and at GlaxoSmithKline who helped to organize and run the study and L. Frith, M. Gibbs, N. Gul, M. Ho, and D. Lawrence for assistance with statistical analysis and compilation of the manuscript.
References
1. Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention: NHLBI/WHO Workshop Report. Bethesda: National Institutes of Health, National Heart, Lung and Blood Institute; 2002. Publication No. 02-3659.
2. British Thoracic Society (BTS) and Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. Thorax 2003;58:i1-i94.
3. National Asthma Education and Prevention Program. Guidelines for the diagnosis and management of asthma: expert panel report 2. Bethesda: National Institutes of Health, National Heart, Lung and Blood Institute; 1997. Publication No. 97-4051.
4. Adams RJ, Fuhlbrigge A, Guilbert T, Lozano P, Martinez F. Inadequate use of asthma medication in the United States: results of the asthma in America national population survey. J Allergy Clin Immunol 2002;110:58-64.
5. Lai CKW, de Guia TS, Kim Y-Y, Kuo S-H, Mukhopadhyay A, Soriano JB, Trung PL, Zhong NS, Zainudin N, Zainudin BM. Asthma control in the Asia-Pacific region: the Asthma Insights and Reality in Asia-Pacific Study. J Allergy Clin Immunol 2003;111:263-268.
6. Rabe KF, Vermeire PA, Soriano J, Maier WC. Clinical management of asthma in 1999: the Asthma Insights and Reality in Europe (AIRE) study. Eur Respir J 2000;16:802-807.
7. Holt S, Kljakovic M, Reid J. Asthma morbidity, control and treatment in New Zealand: results of the Patient Outcomes Management Survey (POMS), 2001. N Z Med J 2003;116:U436.
8. Jones KG, Bell J, Fehrenbach C, Pearce L, Grimley D, McCarthy TP. Understanding patient perceptions of asthma: results of the Asthma Control and Expectations (ACE) survey. Int J Clin Pract 2002;56:89-93.
9. Bateman ED, Bousquet J, Braunstein GL. Is overall asthma control being achieved? A hypothesis-generating study. Eur Respir J 2001;17:589-595.
10. Bateman ED, Frith L, Braunstein GL. Achieving guideline-based asthma control: docs the patient benefit? Eur Respir J 2002;20:588-595.
11. Global Initiative for Asthma (GINA). Pocket guide for asthma management and prevention. Bethesda: National Institutes of Health, National Heart, Lung, and Blood Institute; 1998. Publication No. 95-3659B.
12. Bateman E, Boushey B, Bousquet J, Busse W, Clark T, Pauwels R, Pedersen S. Achievement of guideline-based asthma control with salmeterol/fluticasone propionate compared with fluticasone propionate alone: results of the GOAL study [abstract]. 4th Triennial World Asthma Meeting Abstract Book, February 16-19, 2004. Bangkok, Thailand: Asthma Foundation of Thailand; 2004. p. 131.
13. Boushey H, Bateman E, Bousquet J, Busse W, Clark T, Pauwels R, Pedersen S. Achieving total control of asthma with salmeterol/fluticasone propionate versus fluticasone propionate alone: GOAL study results [abstract]. 4th Triennial World Asthma Meeting Abstract Book, February 16-19, 2004. Bangkok, Thailand: Asthma Foundation of Thailand; 2004. p. 132.
14. Pedersen S, Bateman E, Boushey H, Bousquet J, Busse W, Clark T, Pauwels R. Aiming for guideline defined total control of asthma improves one-year asthma outcomes: results of the GOAL study [abstract]. 4th Triennial World Asthma Meeting Abstract Book, February 16-19, 2004. Bangkok, Thailand: Asthma Foundation of Thailand; 2004. p. 120.
15. Busse W, Bateman E, Boushey H, Bousquet J, Clark T, Pauwels R, Pedersen S. Aiming to achieve total control with salmeterol/fluticasone propionate and fluticasone propionate alone is well tolerated: GOAL 1-year safety data [abstract]. 4th Triennial World Asthma Meeting Abstract Book, February 16-19, 2004. Bangkok, Thailand: Asthma Foundation of Thailand; 2004. p. 138.
16. Pauwels R, Bateman E, Boushey H, Bousquet J, Busse W, Clark T, Pedersen S. Addition of oral corticosteroids to combination therapy has little impact on achieving total control of asthma [abstract]. 4th Triennial World Asthma Meeting Abstract Book, February 16-19, 2004. Bangkok, Thailand: Asthma Foundation of Thailand; 2004. p. 135.
17. Busse W, Bateman E, Boushey H, Bousquet J, Clark T, Pauwels R, Pedersen S. Achieving GINA/NIH guideline-based asthma control with salmeterol/fluticasone compared with fluticasone alone: the results of the GOAL study. J Allergy Clin Immunol 2004;113(2 Suppl 1):S114.
18. Pauwels R, Bateman E, Boushey H, Bousquet J, Busse W, Clark T, Pedersen S. Can total control of asthma he achieved? The results of the GOAL study. J Allergy Clin Immunol 2004;113(2 Suppl 1 ):S276-S277.
19. Boushey H, Bateman E, Bousquet J, Busse W, Clark T, Pauwels R, Pedersen S. Improvements in asthma outcomes following 1 year of treatment with salmeterol/fluticasone or fluticasone alone when stepped up to achieve guideline-defined total control. J Allergy Clin Immunol 2004;113(2 Suppl 1):S114-S115.
20. Clark T, Bateman E, Boushey H, Bousquet J, Busse W, Pauwels R, Pedersen S. Salmeterol/fluticasone and fluticasone alone are well tolerated over 1 year of treatment stepped-up to achieve total control: safety results of the GOAL study. J Allergy Clin Immunol 2004;113(2 Suppl 1):S115.
21. Bousquet J, Bateman E, Boushey H, Busse W, Clark T, Pauwels R, Pedersen S. The effect of oral corticosteroids and high-dose combination therapy on achieving control of refractory asthma. J Allergy Clin Immunol 2004;113(2 Suppl 1):S113.
22. Clark T, Bateman E, Boushey H, Bousquet J, Busse W, Pauwels R, Pedersen S. Time course of achievement of individual clinical goals of asthma treatment: the results of the GOAL study [abstract]. Am J Respir Crit Care Med 2004;169:A318.
23. Pauwels R, Bateman E, Boushey H, Bousquet J, Busse W, Clark T, Pedersen S. Aiming for total control of asthma reduces the risk of exacerbations: a comparison of salmeterol/fluticasone propionate vs fluticasone propionate alone [abstract]. Am J Respir Crit Care Med 2004;169:A87.
24. Bateman E, Boushey H, Bousquet J, Busse W, Clark T, Pauwels R, Pedersen S. Achieving and maintaining guideline defined asthma control with salmeterol/fluticasone propionate versus fluticasone propionate alone: the results of the GOAL study [abstract]. Am J Respir Crit Care Med 2004;169:A87.
25. Bateman E, Pauwels R, Boushey H, Bousquet J, Busse W, Clark T, Pedersen S. Aiming for total control of asthma significantly improves asthma-related quality of life: salmeterol/fluticasone propionate versus fluticasone propionate alone. Am J Respir Crit Care Med 2004;169:A87.
26. Clark TJH, Bateman ED, Boushey H, Bousquet J, Busse W, Pauwels R, Pedersen S. Aiming for total control of asthma in ICS-free patients improves traditional outcomes: results of the Gaining Optimal Asthma controL (GOAL) study [abstract]. 23rd Meeting of the European Academy of Allergology and Clinical Immunology Meeting, June 12-16, 2004. Amsterdam, The Netherlands: 204. p. 669.
27. Pedersen SE, Bateman ED, Boushey H, Bousquet J, Busse W, Clark T, Pauwels R. Aiming for total control of asthma in patients taking inhaled corticosteroids improves traditional outcomes: results of the Gaining Optimal Asthma controL (GOAL) study [abstract]. 23rd European Academy of Allergology and Clinical Immunology Meeting Abstract Book, June 12-16, 2004. Amsterdam, The Netherlands: 204. p. 670.
28. Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax 1992;47:76-83.
29. Ward C, Pais M, Bish R, Reid D, Feltis B, Johns D, Walters EH. Airway inflammation, basement membrane thickening and bronchial hyperresponsiveness in asthma. Thorax 2002;57:309-316.
30. Reddel HK, Jenkins CR, Marks GB, Ware SI, Xuan W, Salome CM, Badcock CA, Woolcock AJ. Optimal asthma control, starting with high doses of inhaled budesonide. Eur Respir J 2000;16:226-235.
31. Chaudhuri R, Livingston E, McMahon AD, Thomson L, Borland W, Thomson NC. Cigarette smoking impairs the therapeutic response to oral corticosteroids in chronic asthma. Am J Respir Crit Care Med 2003;168:1308-1311.
32. Pedersen B, Dahl R, Karlstrom R, Peterson CG, Venge P. Eosinophil and neutrophil activity in asthma in a one-year trial with inhaled budesonide: the impact of smoking. Am J Respir Crit Care Med 1996;153:1519-1529.
33. Kavuru M, Melamed J, Gross G, LaForce C, House K, Prillaman B, Baitinger L, Woodring A, Shah T. Salmeterol and fluticasone propionate combined in a new powder inhalation device for the treatment of asthma: a randomized, double-blind, placebo-controlled trial. J Allergy Clin Immunol 2000;150:1108-1116.
34. Shapiro G, Lumry W, Wolfe J, Given J, White MV, Woodring A, Baitinger L, House K, Prillaman B, Shah T. Combined salmeterol 50mcg and fluticasone propionate 250 mcg in the Diskus device for the treatment of asthma. Am J Respir Crit Care Med 2000;161:527-534.
35. O'Byrne PM, Barnes PJ, Rodriguez-Roisin R, Runnerstrom E, Sandstrom T, Svensson K, Tattersfield A. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. Am J Respir Crit Care Med 2001;164:1392-1397.
36. Chapman KR, Ernst P, Grenville A, Dewland P, Ziminerman S. Control of asthma in Canada: failure to achieve guideline targets. Can Respir J 2001;8:35A-40A.
37. Aubier M, Pieters WR, Schlösser NJJ, Steinmetz K-O. Salmeterol/fluticasone propionate (50/500 µg) in combination in a Diskus inhaler (Seretide/Advair) is effective and safe in the treatment of steroid-dependent asthma. Respir Med 1999;93:876-884.
38. Li JTC. Ford LB, Chervinsky P, Weisberg SC, Kellerman DJ, Faulkner KG, Herje NE, Hamedani A, Harding SM, Shah T. Fluticasone propionate powder and lack of clinically significant effects on hypothalamic-pituitary-adrenal axis and bone mineral density over 2 years in adults with mild asthma. J Allergy Clin Immunol 1999;103:1062-1068.
39. Allen DB, Bielory L, Derendorf H, Dluhy R, Colice GL, Szefler SJ. Inhaled corticosteroids: past lessons and future issues. J Allergy Clin Immunol 2003;112:S1-S40.
40. European Community for Coal and Steel. Standardisation of lung function tests as contained in the report of the working party of the European Community for Steel and Coal. Bull Eur Physiopathol Respir 1983;19:1-95.
41. Polgar G, Promadhat V. Pulmonary function testing in children: techniques and standards. Philadelphia: WB Saunders Company; 1971. p. 254.
Eric D. Bateman, Homer A. Boushey, Jean Bousquet, William W. Busse, Tim J. H. Clark, Romain A. Pauwels, and Søren E. Pedersen for the GOAL Investigators Group
University of Cape Town, Cape Town, South Africa; University of California, San Francisco, San Francisco, California; Hôpital Arnaud De Villeneuve, Montpellier, France; University of Wisconsin Medical School, Madison, Wisconsin; Imperial College, London, United Kingdom; Ghent University Hospital, Ghent, Belgium; and University of Southern Denmark, Kolding Hospital, Kolding, Denmark
(Received in original form January 9, 2004; accepted in final form July 14, 2004)
Supported by GlaxoSmithKline R&D Limited.
Correspondence and requests for reprints should be addressed to Eric D. Bateman, M.D., F.R.C.P., UCT Lung Institute, P.O. Box 34560, Groote Schuur 7937, Cape Town, South Africa. E-mail: ebateman@uctgsh1.uct.ac.za
This article has an online supplement, which is accessible from this issue's table of contents online at www.atsjournals.org
Am J Respir Crit Care Med Vol 170. pp 836-844, 2004
Originally Published in Press as DOI: 10.1164/rccm.200401-033OC on July 15, 2004
Internet address: www.atsjournals.org
Copyright American Thoracic Society Oct 15, 2004
Provided by ProQuest Information and Learning Company. All rights Reserved