Monday
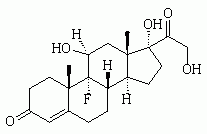
There is something cartoonish about Bernardo Marroquin--dangling arms, head that looks like it's rolling off his kyphotic neck, lumpish face and deadpan expression. Eighty-four years old, he presents with his daughter and multiple concerns, including legs that fall asleep and dizziness that landed him in our emergency room a few days ago. Laboratory tests were normal, but his chest x-ray revealed fibrotic changes and a possible mass. Today, his blood pressure drops from 130/80 mm Hg lying to 80/50 mm Hg standing. No wonder he feels dizzy! When I use a monofilament to test his sensation, he reports no feeling in his toes--nor in his feet, nor in his hands. Hmm. I check his cheeks. Still nothing. His daughter laughs. "Looks like you're dead! "He finally nods when I poke his forehead. Now, in my bewilderment, I feel cartoonish. Mr. Marroquin worked as a farm hand harvesting--and often burning--sugar cane fields. "He'd return charcoal black," says his daughter. Might that explain the chest x-ray? I prescribe Mr. Marroquin fludrocortisone for his orthostasis; check levels of vitamin [B.sub.12], folate, and thyroid-stimulating hormone for the bizarre neuropathic findings; and order a computed tomographic scan of his chest. Is there an ominous diagnosis lurking? I don't think so, but I do hope to make him feel better.
Tuesday
"Oscar's leaving me--for another woman!" I don't know which stuns me more--this bombshell, or the good humor with which Sandra, a youthful and energetic 55-year-old woman, delivers it. As the news sinks in, it occurs to me that I might have seen it coming. Oscar and Sandra have not been romantically intimate for a long time, something she told me after I'd been Oscar's doctor for years. I tried several times to talk it over with him--without results. "Everything's fine," he would insist, his stolid, opaque shyness contrasting with Sandra's animated openness. I finally gave up trying to intervene, hoping they would figure things out. And, they apparently have, in a way I hadn't anticipated. "You don't seem too upset," I observe. Sandra shrugs. "I'm not surprised. But I am worried. What will happen to my health insurance? I'm only covered under Oscar's plan." I'm initially startled that this is her top priority right now, then dismayed that anyone's medical care should be so unfairly vulnerable. "How are you doing?" I ask. She smiles sadly. "Maybe it's for the best." I nod, privileged to share the room with her and be part of this evolving chapter in her life saga.
Wednesday
While reading a book, I'm reminded of a patient. The Spirit Catches You and You Fall Down is Anne Fadiman's beautifully spun tale of a chronically ill Hmong girl whose American doctors, by ignoring her family's cultural beliefs, doom their well-meaning interventions to failure. I recall Mr. Valois, the erect, proud, 75-year-old Haitian man who presented one day with shortness of breath and a sore leg. When I diagnosed a pulmonary embolism based on a negative chest x-ray and positive venous Doppler study, he refused hospitalization--or any further testing. I was flabbergasted. We held a tortured conversation--in French, patois, and English. "You might die," I said. "I don't care," he replied. When I played my ace--enlisting his family to twist his arm--he only grew more obstinate. Defeated, I treated him with warfarin as an outpatient, imagining how other doctors might ridicule me. A week later, Mr. Valois got fed up with my blood tests and pills--and stopped treatment altogether. I was furious. I'd tried so hard and worried so much. My mood did not improve when he recovered completely. Today, from the safety of years and with this book in mind, I can finally appreciate the advanced lesson in patient-centered care that Mr. Valois delivered at the time to an unappreciative pupil.
Thursday
As I'm about to examine a patient, there's a knock on the door. A resident pokes her head in. "Sorry to interrupt," she says. "Something urgent in the back." I don't need the somber faces in our hushed conference room to tell me what it's about. Our associate program director has just died at age 45 of metastatic pancreatic cancer. All the medical skills we practice and teach could not save her. We all knew her prognosis; no one should be surprised. Yet, we are shocked. Numb. I'm reminded of wildlife programs, at that awful moment when a lion takes down a member of the gazelle herd. I've always wondered at the flickering reactions of the other gazelles as they watch--then look away from--their thrashing comrade. Now, I can guess. They are stunned--disbelieving. And, so are we, our entire staff, who have gathered with tears in our eyes, embracing one another, saying prayers for the departed and offering each other comfort. I finally tear myself away and return to my patient, who has her own issues, her own sadness. I do my best to be there for her. Later on, I'll return to this hollow feeling in my chest. Later on, it will be my turn to grieve.
Friday
Today, for the first time in memory, I give a patient money to buy food. Isabelle, a 40-year-old woman with a sad countenance and history of gestational diabetes, comes in with hematuria and flank pain--something I thought we'd cured a month ago by removing a ureteral stone. Before I enter the room, Yvette, my astute nursing assistant, pulls me aside. "She hasn't eaten in two days." Isabelle, listless and pale, is seated; her two-year-old child is draped across her chest. She doesn't mention food, but when I ask about her five children and their food pantry, a solitary tear trickles down her cheek. She looks away. She has no money until the first of the month. The children's father is no help. A check from her brother in California is due any day. After sorting out the urologic issue, I pull a couple of bills from my wallet and put them on the table. She pushes them away. I slide them back toward her; she relents." How much would you have given her?" I ask my daughters later. "A hundred dollars," Nikki answers. "More," says Ariel. I wasn't quite that generous. Still, I hope she had enough to cover some basics--and maybe a few treats, too.
Saturday/Sunday
As a family practice resident, I was taught about child development, but never this. These days, life with Ariel, 12, and Nikki, 10, can be summarized in two words: "beauty products." At a local discount emporium, they happily peruse tubes and tubs of lip gloss, mascara, eye liner, eye shadow, blush, skin cleanser, shampoos, conditioners, gels, tints, ad infinitum. Because Ariel often uses our bedroom as her styling salon, I find these products sprinkled across our bed and on my night stand. Conversation has become a challenge. If Ariel's anywhere near a mirror, her gaze drifts to her reflection, and I find myself chatting to her ear--to the tune of distracted "Uh-huhs"--while she tilts her head left and right, pouting her lips and making minute adjustments to strands of hair. As a man, I find this behavior puzzling; as a dad, I consider both my daughters exquisite without a speck of makeup. But, I'm told that their obsession is a developmental phase that shouldn't be derailed. So, I exercise patience, remembering their cutesy, unrealistically proportioned fashion dolls, which were eventually given awful haircuts and colored marker beards--and then cast aside. "You're beautiful," I tell my glamorized daughters, hoping that this phase, too, shall pass.
For the past dozen years, Dr. Paul Gross has been on the residency faculty of New York Medical College at St. Joseph's in Yonkers, New York (a city of 196,000). He divides his time between patient care, resident supervision, teaching, and life with his own family--a wife and two daughters.
Address correspondence to Paul Gross, M.D. (e-mail pgross@pol.net). In order to preserve patient confidentiality, the patients' names and identifying characteristics have been changed in each scenario.
COPYRIGHT 2004 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group