Benzodiazepines are the most commonly prescribed sedative-hypnotic drugs in the United States. These agents are widely used in the management of insomnia, seizure disorders, and panic and anxiety states. Because of their sedative and amnestic properties, benzodiazepines are also used in patients who are undergoing anesthesia. In addition, these drugs are often implicated in intentional or iatrogenic overdose.
Serious toxicity seldom occurs with benzodiazepines. However, these agents can cause respiratory and central nervous system depression, which may lead to hypoventilation or aspiration of gastric contents. Selective pharmacologic reversal of these effects may obviate the need for mechanical ventilation or other invasive supportive procedures. The presence or absence of a clinical response to a benzodiazepine antagonist can also provide diagnostic information, analogous to the specific reversal of the effects of opiates by naloxone (Narcan).[1]
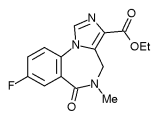
Flumazenil (Mazicon) has been approved by the U.S. Food and Drug Administration as an adjunct in the management of patients with benzodiazepine toxicity. The first specific benzodiazepine antagonist to be developed, flumazenil has been commercially available in the United States since late 1991. Chemically, this drug is classified as an imidazobenzodiazepine.
Mechanism of Action
The benzodiazepines are agonists--drugs that bind to a receptor and stimulate characteristic effects. Sedation, amnesia and anticonvulsant effects occur when a benzodiazepine agonist binds to its receptor.
In contrast, flumazenil is an antagonist--a drug that occupies a specific receptor site but has no intrinsic effects of its own. An antagonist blocks the effect of an agonist drug.
The benzodiazepine receptor is a complex structure that modulates chloride transport across neuronal cell membranes. This receptor is adjacent to the neuronal gamma-aminobutyric acid (GABA) receptor. The binding of an agonist to either the benzodiazepine or GABA receptor effects a "gating" function of the chloride channel. As a result, the intracellular concentration of chloride increases. This, in turn, alters the cellular resting potential, thereby reducing neuronal excitability.
Flumazenil has a greater affinity for the benzodiazepine receptor than do most available benzodiazepines (Table 1). In both animals and humans, flumazenil blocks the anxiolytic, muscle relaxant, sedative, ataxic, anticonvulsant, amnestic and anesthetic effects of the benzodiazepines.[2-4] Flumazenil does not antagonize the effects of any sedative drugs (e.g., ethanol, barbiturates) that do not act at the benzodiazepine receptor.[5,6]
Pharmacokinetics
When given intravenously, flumazenil reaches peak serum levels within minutes and has an initial distribution half-life of seven to 15 minutes. The drug is 40 to 50 percent protein bound and has a volume of distribution of 1.6 L per kg, which indicates significant tissue uptake.(2) Flumazenil is primarily metabolized by the liver and has a terminal half-life of 41 to 79 minutes.
The pharmacokinetics of flumazenil are not significantly affected by age, sex or renal impairment. Patients with moderate to severe liver disease or chronic stable kidney failure tolerate flumazenil without difficulty. Renal insufficiency does not alter the half-life of the drug, but the half-life increases to 1.3 to 2.4 hours in patients with moderate or severe hepatic dysfunction (manufacturer's package insert).
In various animal studies, flumazenil has been shown to have a very low degree of toxicity. Based on these data, the therapeutic or safety index of flumazenil in humans has been estimated to be over 3,000.[7] The therapeutic index is defined as the ratio between the median lethal dose (LD) and the median effective dose (ED). This [LD.sub.50]/[ED.sub.50] ratio is an excellent indicator of drug selectivity.
Adverse Effects
The adverse effects of flumazenil include dizziness, nausea, agitation, headache, fatigue, hot flushes and sweating. Adverse reactions to this drug are usually related to reversal of the therapeutic effects of benzodiazepines.
Precipitation of seizure activity is the most serious adverse reaction to flumazenil that has been reported. Although a true cause-and-effect relationship has not definitely been established, flumazenil may induce seizures in two specific clinical circumstances: (1) when patients are using a benzodiazepine chronically, especially if the drug is being used to manage a seizure disorder and (2) when overdose patients have ingested both a benzodiazepine and a tricyclic antidepressant agent. In the latter circumstance, it is believed that rapid reversal of the anticonvulsant effects of the benzodiazepine may unmask the convulsant properties of the tricyclic antidepressant.[8]
Two recently completed multicenter trinals have conclusively validated the safety and efficacy of flumazenil in the setting of polydrug overdose.[9] The few reported seizures in these trials were not conclusively linked to the administration of flumazenil. In most cases, the seizures were of short duration, were self-limited and were not life-threatening. However, because of the potential for the development of seizures, flumazenil should be used with caution in the setting of polydrug overdose if tricyclic antidepressant toxicity is suspected.
Since flumazenil is a competitive antagonist, any seizure activity that warrants pharmacologic treatment may be managed with a nonbenzodiazepine anticonvulsant. If a benzodiazepine is used, it must be administered in doses sufficient to overcome the competitive blockade.
Dosage
Several clinical parallels can be drawn between the use of flumazenil and naloxone. Both drugs are capable of rapidly reversing the sedation and respiratory depression caused by benzodiazepines and opiates, respectively, but both drugs may also precipitate acute withdrawal if they are used inappropriately. Clinical experience with naloxone has shown that drug titration using small, repetitive doses allows gradual, controlled awakening with a lower incidence of agitation. This approach has also been advocated for flumazenil.
Flumazenil is supplied at a standard concentration of 0.1 mg per mL in 5- or 10-mL vials. Generally, an initial bolus of 2 mL (0.2 mg) is given intravenously over 30 seconds. Although the manufacturer recommends waiting 30 seconds between boluses to assess the patient's response, it seems reasonable to wait a few minutes to allow the drug to be distributed.
Reversal of sedation and respiratory depression usually becomes evident within one to two minutes after flumazenil is administered, and the peak effect is reached in six to 10 minutes. If no response occurs after the initial bolus, repeat doses of 0.3 to 0.5 mg (3 to 5 mL) may be given incrementally.
As a general rule of thumb, less drug is needed for reversal of sedation following conscious sedation during medical procedures than for reversal of sedation in intentional overdose. Most patients who receive flumazenil after conscious sedation respond adequately to doses of 0.2 to 1.0 mg. Patients who have overdosed often require cumulative doses as high as 5.0 mg.
The half-life of flumazenil is rather short, averaging 50 minutes in patients who do not have significant liver disease. Most benzodiazepines, especially if they are taken in overdose, have half-lives that greatly exceed the half-life of flumazenil. For this reason, patients successfully treated with flumazenil must be watched closely for the recurrence of sedation. Recurrent sedation can be managed with repetitive bolus injections of flumazenil or with a flumazenil infusion delivered at a rate of 0.2 to 0.5 mg per hour.
Recurrent sedation is rarely a problem when short-acting benzodiazepines such as midazolam (Versed) are used for medical procedures. In most cases, patients can be safely discharged after a brief period of observation following the reversal of sedation.
Clinical Use
Management of intentional overdoses and the reversal of procedural sedation are two clinical areas in which flumazenil will have a considerable impact. Flumazenil antagonizes many of the deleterious side effects of the benzodiazepines.
RESPIRATORY DEPRESSION
The FDA requires that flumazenil labeling carry a disclaimer stating that the drug has not been established as an effective treatment for benzodiazepine-induced respiratory depression. However, clinical experience has shown that flumazenil is quite effective for this purpose.
Several studies[10,11] have shown that flumazenil causes an impressive reversal of benzodiazepine-induced hypoxemia. Other studies[12-17] have demonstrated improved spontaneous breathing with increased vital capacity, forced expiratory volume and blood oxygen saturation following the administration of flumazenil.
Of course, benzodiazepine-induced respiratory depression in the overdose setting may be aggravated by other co-ingestants, such as narcotics, alcohol or barbiturates. In this setting, a patient may not respond to flumazenil or may respond incompletely, either because an inadequate dose of flumazenil was used or because of additive respiratory depression from the other agents the patient has taken. For these reasons, flumazenil is not recommended as the initial treatment for benzodiazepine-induced hypoventilation. Patients who respond positively to flumazenil must be carefully monitored for recurrence of sedation and hypoventilation.
Symptom reversal is more complete when higher doses of flumazenil are used.[5,18] Although the drug often produces a dramatic reversal of sedation, its effect on amnesia is somewhat less reliable. Therefore, if flumazenil is used in the outpatient setting, discharge instructions should be given in verbal or written form to a reliable friend or family member who will be accompanying the patient.
INTRACRANIAL AND CEREBRA PERFUSION PRESSURES
Chiolero and colleagues[19] reported on the effects of flumazenil on intracranial and cerebral perfusion pressures in 15 patients with severe head injury who received midazolam sedation for mechanical ventilation. Continuous monitoring revealed two patterns of response to flumazenil. Following the administration of flumazenil, no significant change in intracranial pressure or cerebral perfusion pressure occurred when intracranial pressure was stable before the drug was given. On the other hand, when the intracranial pressure was abnormal, a dramatic increase in intracranial pressure and a concomitant decrease in cerebral perfusion pressure occurred following the administration of flumazenil.
Chiolero and colleagues[19] concluded that flumazenil should not be administered to patients with severe head injuries when there is evidence of unstable intracranial pressure. Aside from this, a review of data from the United States and elsewhere reveals no clinically significant post-treatment changes in other hemodynamic parameters after flumazenil is administered.[9,20,21]
Final Comment
As the first specific benzodiazepine antagonist, flumazenil would appear to have an assured place in the medical armamentarium. The availability of this drug adds a margin of safety when a benzodiazepine is used in anesthesia and conscious sedation. With a few precautions, flumazenil also can be quite useful in the diagnosis and treatment of intentional benzodiazepine overdose. REFERENCES [1.] Hojer J, Baehrendtz S, Matell G, Gustafsson LL. Diagnostic utility of flumazenil in coma with suspected poisoning: a double blind, randomised controlled study. Br Med J 1990;301:1308-11. [2.] Haefely WE. The story and activity of flumazenil (Anexate). Acta Anaesthesiol Belg 1989;40:3-9. [3.] Roncari G, Ziegler WH, Guentert TW. Pharmacokinetics of the new benzodiazepine antagonist Ro 15-1788 in man following intravenous and oral administration. Br J Clin Pharmacol 1986;22:421-8. [4.] Dunton AW, Schwam E, Pitman V, McGrath J, Hendler J, Siegel J. Flumazenil: US clinical pharmacology studies. Eur J Anaesthesiol Suppl 1988;2:81-95. [5.] Klotz U, Kanto J. Pharmacokinetics and clinical use of flumazenil (Ro 15-1788). Clin Pharmacokinet 1988;14:1-12. [6.] Richards JG, Burkard WP, Lorenz HP, Mohler H. Preclinical research findings with flumazenil (Ro 15-1788, [Anexate.sup.TM]): biochemistry and cytopharmacology. Eur J Anaesthesiol Suppl 1988;2:39-45. [7.] Amrein R, Hetzel W, Hartmann D, Lorscheid T. Clinical pharmacology of flumazenil. Eur J Anaesthesiol Suppl 1988;2:65-80. [8.] Lheureux P, Vranckx M, Leduc D, Askenasi R. Flumazenil in mixed benzodiazepine/tricyclic antidepressant overdose: a placebo-controlled study in the dog. Am J Emerg Med 1992;10:184-8. [9.] Flumazenil. Integrated summary of efficacy. Data on file. Nutley, N.J.: Roche Laboratories, a division of Hoffman-LaRoche Inc., 1990. [10.] Flumazenil and hypoxic ventilatory response [Letter]. Anesth Analg 1990;70:122-4. [11.] Alexander CM, Gross JB. Sedative doses of midazolam depress hypoxic ventilatory responses in humans. Anesth Analg 1988; 67:377-82. [12.] Radakovic D, Toia D, Bentzinger C. Double-blind, placebo-controlled study of the effects of Ro 15-1788 (flumazenil, [Anexate.sup.TM]) on recovery of ventilatory function after total intravenous anesthesia with midazolamalfentanyl. Eur J Anaesthesiol Suppl 1988; 2:279-82. [13.] Dimitriou B, Kottis G, Bathrelou S, Triantaphyllidis A. Flumazenil in reversal of the central effects of midazolam used as induction agent in general anaesthesia. Arzneimittel-Forschung 1989;39:399-400. [14.] Klausen NO, Juhl O, Sorensen J, Ferguson AH, Neumann PB. Flumazenil in total intravenous anaesthesia using midazolam and fentanyl. Acta Anaesthesiol Scand 1988;32: 409-12. [15.] Kulka PJ, Lauven PM, Schuttler J, Apffelstaedt C. Methohexital vs midazolam/flumazenil anaesthesia during laryngoscopy under jet ventilation. Acta Anaesthesiol Scand Suppl 1990,92:90-5. [16.] Philip BK, Simpson TH, Hauch MA, Mallampati SR. Flumazenil reverses sedation after midazolam-induced general anesthesia in ambulatory surgery patients. Anaesth Analg 1990;71:371-6. [17.] Weinbrum A, Geller E. The respiratory effects of reversing midazolam sedation with flumazenil in the presence or absence of narcotics. Acta Anaesthesiol Scand Suppl 1990; 92:65-9. [18.] Amrein R, Hetzel W. Pharmacology of Dormicum (midazolam) and Anexate (flumazenil). Acta Anaesthesiol Scand Suppl 1990;92:6-15. [19.] Chiolero RL, Ravussin P, Anderes JP, Ledermann P, de Tribolet N. The effects of midazolam reversal by RO 15-1788 on cerebral perfusion pressure in patients with severe head injury. Intensive Care Med 1988;14:196-200. [20.] Hartmann D, Fluckiger A, Ziegler WH, Timm U, Zell M. Experimental model for the investigation of kinetic and/or dynamic interactions between drugs and ethanol in humans. J Pharm Sci 1988;77:299-303. [21.] White PF, Shafer A, Boyle WA 3d, Doze VA, Duncan S. Benzodiazepine antagonism does not provoke a stress response. Anesthesiology 1989;70:636-9.
COPYRIGHT 1993 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group