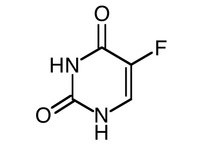
Intralesional 5-Fluorouracil in the Treatment of Keloids: An Open Clinical and Histopathologic Study
Kontochristopoulos G, MD, et al. Journal of the American Academy of Dermatology. 2005;52(3): 474-479.
Summary
The authors present an open-label trial to evaluate the efficacy of intralesional 5-fluorouracil (5-FU) in the treatment of keloids. Objectives included both clinical and histopathologic correlations. The study was comprised of 20 patients with keloids. Keloids were predominantly on the upper arms, back, and chest. The duration of keloids among patients spanned 0.2 to 20 years. Eleven patients had undergone prior treatment. After screening for pregnancy, chronic renal failure, and abnormal liver function tests and complete blood counts, patients underwent once weekly intralesional injections of 5-FU at a concentration of 50 mg/mL for an average of 7 treatments. Depending on the size of the keloid, multiple injections were given at 1-cm intervals. On average, 0.2 to 0.4 mL/[cm.sup.2] was injected at each treatment. In addition, 10 patients had punch biopsies of the injection sites both prior to and after 6 sessions of treatment. Biopsies were evaluated using hematoxylin and eosin staining as well as immunohistochemical staining for Ki-67 and transforming growth factor beta (TGF-beta). Patients were followed for recurrence of keloids up to 1 year. With the exception of one patient, all experienced reduction in the size of keloids. Complete resolution of a keloid was found in one patient, while 8 patients experienced a 75% reduction, 8 had a 50% reduction, and 2 had a 25% reduction in size. The authors state that keloids which had been untreated and were small in size had a more favorable response. Nine patients with improvement had recurrence 1 to 6 months after receiving their last injection. Of note, a statistically significant difference was found regarding duration of the keloid and recurrence. Keloids responding to treatment and of less than 2 years duration were less likely to recur. Regarding histopathology, 4 of 8 patients had complete resolution of thick hyalinized collagen noted prior to treatment and 4 of 6 patients had elimination of whorls of spindle cells seen prior to treatment. Ki-67 showed a statistically significant decrease in expression in all patients after treatment, while TGF-beta showed only a minimal decrease in 6 patients. Pain and hyperpigmentation at the injection site was noted in all patients. Six patients developed superficial ulcerations.
Comment
This was an interesting study as the authors tried to correlate both the histologic and clinical effects of 5-FU in the treatment of keloids. Importantly, recurrence was also evaluated. Although the majority of patients had a decrease in the size of their keloids, only one patient experienced complete resolution. Pain is an important side effect of this therapy; 4 patients needed 5-FU combined with Xylocaine secondary to intolerable pain. It would have been interesting to have compared this therapy with a more widely used treatment such as intralesional triamcinolone (IL-TAC). A comparison study between the two seems warranted to assess whether 5-FU is any more effective than IL-TAC, both in the resolution and recurrence of keloids.
COPYRIGHT 2005 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2005 Gale Group