Kroenke K, West SL, Swindle R, et al. Similar effectiveness of paroxetine, fluoxetine, and sertraline in primary care. JAMA 2001; 286:2947-55.
* BACKGROUND Although selective serotonin reuptake inhibitors (SSRIs) are the most commonly prescribed antidepressants, data comparing the effectiveness of the members of this class of antidepressants are limited. This study compared the effectiveness of 3 SSRIs in a naturalistic study designed to mimic typical primary care prescribing.
* POPULATION STUDIED Adult outpatients from 2 primary care research networks were eligible for the study if their primary care doctor had diagnosed a depressive disorder requiring medication. Patients were excluded if they were cognitively impaired, terminally ill, or suicidal; lived in a nursing home; were currently taking a non-SSRI antidepressant; or had recently taken an SSRI antidepressant. Data were analyzed from 546 patients (79% of those invited to participate), who were randomized and completed at least 1 follow-up interview.
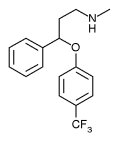
* STUDY DESIGN AND VALIDITY This was a randomized, controlled, unblinded trial designed to reflect actual primary care practice. After being diagnosed by their primary care physician (PCP) with clinical depression, with the PCP using his or her usual methods to make the diagnosis, patients were randomized through a concealed allocation procedure to receive daily doses of 20 mg paroxetine (Paxil), 20 mg fluoxetine (Prozac), or 50 mg sertraline (Zoloft). Both the patients and doctors were aware of the medication assignment. The PCP could adjust the dose to clinical response or change patients to a different medication. By the end of the study, less than half of the patients were taking the medication they had originally started.
The 3 groups were similar in baseline characteristics and in adherence to the study medications. Data analysis was by intention to treat. The outcomes assessors were not blind to treatment group assignment. Among this study's strengths are the large sample size and the naturalistic design that included physicians from a variety of community practices and patients with comorbid illnesses.
Three limitations are worth noting. First, adherence to the initially assigned medication was low; less than half of the patients were still taking their initially assigned medication on completing the study. Second, the outcomes assessors were not blinded to the patients' medication assignments. Third, in contrast to usual clinical practice, the medications were provided free of charge to the study participants.
* OUTCOMES MEASURED The primary outcome was change in the Mental Component Score (MCS) of the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36). The scoring of the MCS incorporates elements of the 8 subscales of the SF-36 and ranges from 0 to 100, with higher scores representing better mental health. Several other measures of depression and social functioning provided secondary outcomes.
* RESULTS Forty-one percent to 50% of participants stopped their initially assigned medication during the 9-month follow-up period. About 20O/a of participants switched to another antidepressant. Roughly 25% stopped taking antidepressants altogether before completion of the follow-up period.
Starting with any of the 3 agents, however, resulted in good outcomes. For the entire sample, the mean MCS improved from 30.9 at baseline to 48.3 at 9 months. The proportion of the sample meeting criteria for major depression decreased from 74% at baseline to 26% at 9 months. MCS improved similarly in the 3 groups (an average of about 16 points, a statistically significant and clinically meaningful change). There were no significant differences in psychological outcome measures among the SSRI treatment groups.
RECOMMENDATIONS FOR CLINICAL PRACTICE
This well-designed study of SSRI treatment for clinical depression in primary care settings found that paroxetine (Paxil), fluoxetine (Prozac), and sertraline (Zoloft) were equally effective for the treatment of depression. Additionally, since the rates of adherence and of adverse effects were similar among the 3 study medications, physicians should feet equally confident prescribing any of these SSRIs. Using the lowest-cost SSRI (fluoxetine just became available generically) is an ethical and reasonable approach.
Joseph B. Straton, MD Peter Cronholm, MD Department of Family Practice and Community Medicine University of Pennsylvania Philadelphia E-mail: straton@mail.med.upenn.edu
COPYRIGHT 2002 Appleton & Lange
COPYRIGHT 2002 Gale Group