New data downplays use of statins for Alzheimer's disease prevention, according to John C.S. Breitner, MD, of VA Puget Sound Health Care System and the University of Washington, who presented at the 9th International Conference on Alzheimer's Disease.
Posting results from 3 long-term population studies, he said, "If you look at a 'snapshot' of statin users compared with non-users at a single moment in time, statin users seem to have a lower risk of Alzheimer's disease (AD). But if you look at people taking statins at enrollment in these studies and follow them over several years, the benefit of statins in warding off dementia largely disappears."
His presentation of the abstract, "Can statins prevent AD, or are they just prescribed less often to those with cognitive disorders?" compared findings of 3 population studies with results of simulated case-control or cross-sectional studies:
* The Cache County Study examined the association of statin use at baseline with incidence of AD (102 cases; 3,308 participants; 10,152 person-years) over 3 years.
* The Cardiovascular Health Study Cognition Study (CHSCS) looked at yearly exposure to statins among 2,798 participants who contributed 15,032 person-years. The CHSCS investigated the link between antecedent statin exposure and 244 instances of incident AD.
* The Adult Changes in Thought study examined association of antecedent statin use and 168 cases of incident AD among 2,356 participants contributing 13,110 person-years.
All studies assessed similar associations of other lipid-lowering agents and AD, and of statin and lipid-lowering agent use with all-cause dementia. All studies found marked differences in findings with simulated case-control or cross-sectional odds ratios vs. prospective design discrete-time or Cox hazard ratios.
"The new data suggest that much of the prior epidemiologic data may be flawed in that properly conducted longitudinal studies do not bear out the 'protective' relationship that has been observed earlier in cross-sectional studies," Dr. Breitner told Geriatrics. "At the least, there should be added caution about the 'statin story' in AD."
Researchers concluded that the inverse association of statin use and AD evident in cross-sectional studies does not appear to be sustained in prospective study designs.
The message to primary care: "Clinicians should not be prescribing statins for indications other than those approved by the FDA. To the extent that doctors felt some sense of 'statins will lower your cholesterol and prevent cardiovascular disease... and they may also prevent AD,' they should probably be less sanguine now about the last part of this argument."
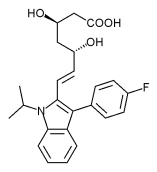
In contrast to Dr. Breitner's findings, Richard Parsons, PhD, of St. Georges Hospital Medical School, presented results suggesting that 4 statins (lovastatin, simvastatin, atorvastatin, and fluvastatin) reduce, to varying degrees, brain cells' production of a protein fragment, B-amyloid, thought to play a prominent role in Alzheimer's, with fluvastatin being the most effective. Long-term use of statins in patients would lead to a decrease in the overall amount of B-amyloid released.
Another study, led by P. Murali Doraiswamy, MD, director of psychiatry clinical trials at Duke University, examined all existing randomized controlled trials of statins in people without dementia (>30,000 participants). The researchers were unable to find evidence that statins protect against cognitive decline. A second smaller study of older individuals at risk of dementia showed that rates of brain tissue shrinkage, measured by magnetic resonance imaging, were the same for statin users and nonusers.
COPYRIGHT 2004 Advanstar Communications, Inc.
COPYRIGHT 2005 Gale Group