Captopril (Capoten) was the first angiotensin converting enzyme (ACE) inhibitor to be developed and marketed in the United States. It was followed closely by two longer-acting agents - enalapril (Vasotec) and lisinopril (Prinivil, Zestril). Multiple studies found that when these agents were used alone, they effectively controlled blood pressure in 50 percent of hypertensive patients; when used in combination within a diuretic, they were effective in 80 to 90 percent of patients with hypertension.[1] Consequently, the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure[1] in 1988 recommended that ACE inhibitors be added to the list of first-line agents for the treatment of essential hypertension.
The available ACE inhibitors have also been shown to be effective in treating congestive heart failure. Improvement has been demonstrated in symptoms,[2,3] hemodynamic parameters[4,5] and New York Heart Association (NYHA) functional class.[6,7] Some studies have also shown a decrease in mortality among patients with severe congestive heart failure who are treated with ACE inhibitors.[2,8,9] However, the precise role of these agents in the treatment of congestive heart failure, relative to the role of other available therapies, is still being defined.
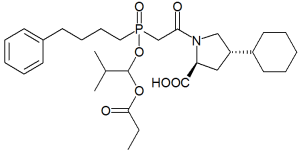
Because of their effectiveness, as well as their excellent side effect and safety profiles, ACE inhibitors now are widely used. In 1992, both captropril and enlapril were among the 20 most frequently prescribed drugs in the United States.[10] In the past several years, the U.S. Food and Drug Administration has approved four new ACE inhibitors: benazepril (Lotensin), fosinopril (Monopril), quinapril (Accupril) and ramipril (Altace). All four agents are converted in vivo to their active forms: benazeprilat, fosinoprilat, quinaprilat and ramiprilat, respectively.
Therapeutic Effectiveness
BENAZEPRIL
In one study[11] of 17 patients with essential hypertension (diastolic blood pressure of 95 to 110 mm Hg), the administration of 10 mg of benazepril per day was shown to decrease diastolic blood pressure to less than 95 mm Hg in seven patients. When the dosage was increased to 10 mg twice daily, 12 (70 percent) of the 17 patients responded to the drug, with an average decrease in diastolic blood pressure of 12 mm Hg.
In a large multicenter study,[12] 206 patients with essential hypertension (diastolic blood pressure of 95 to 114 mm Hg) were randomized to receive once-daily doses of placebo, benazepril or hydrochlorothiazide. The response rates for daily doses of 2, 5 and 10 mg of benazepril were noted to be no greater than the response rate for placebo (25 percent). Overall, the response rate for 20 mg of benazepril (46 percent) was comparable to the response rate for 25 mg of hydrochlorothiazide alone (42 percent). The average reduction in blood pressure with benazepril was 13 mm Hg systolic and8 mm Hg diastolic. In black patients, however, benazepril was found to be less effective than hydrochlorothiazide. (A similar effect has been noted for other ACE inhibitors.). The side effect experienced by study subjects who were given benazepril were no different that those experienced by subjects who were given placebo. Increasing the dosage to 40 and 80 mg of benazepril per day resulted in minimal further improvement in blood pressure.[13]
Benazepril has also been tested at dosages of 2, 5 and 10 mg per day in a small group of patients with NYHA class III or IV congestive heart failure.[14] After four weeks of treatment, symptoms of dyspnea on exertion were improved in 76 percent of patients, and more than 50 percent of patients reported that they no longer had symptoms. Several patients also noted improvement in dyspnea at rest, paroxysmal nocturnal dyspnea and pedal edema. The presence of jugular venous distention and an S3 gallop was noted in fewer patients following treatment with benazepril.
FOSINOPRIL
The response to fosinopril in patients with mild to moderate hypertension has been evaluated in two large multicenter trials.[15,16] The first was three-month double-blind trial followed by an additional 10 to 13 months of open-label study.[15] The initial dosage of 10 mg of fosinopril per day was titrated up to a maximum of 80 mg per day. Twenty-five mg of chlorthalidone was added in patients whose diastolic blood pressure was still greater than 90 mm Hg following treatment with the maximum dosage of fosinopril.
This study found that fosinopril in dosages of 40 and 80 mg per day was significantly more effective than placebo in lowering diastolic blood pressure. Blood pressure control was maintained during the long-term phase of the study, with no evidence of drug tolerance. However, 50 percent of patients required a diuretic for adequate blood pressure control (Table 1).[15] The most common adverse effects reported were dizziness or lightheadedness, cough and gastrointestinal disturbances, which are similar to the symptoms reported with other ACE inhibitors. The discontinuation rate due to side effects was 6.1 percent, which is also comparable to the discontinuation rates for other drugs in this class. Similar results were obtained in a second large study involving more than 400 white patients.[16]
[TABULAR DATA OMITTED]
Fosinopril has also been compared with other antihypertensive agents in two double-blind studies of patients with mild to moderate hypertension.[17,18] When fosinopril was compared with enalapril, no differences were found in response rates, degree of reduction of diastolic blood pressure or reported adverse effects.[17] When fosinopril was compared with sustained-release nifedipine in patients 60 to 80 years of age, no differences were noted in the reduction of either systolic or diastolic blood pressure.[18] The most common adverse effects were the same as the ones reported in other studies.[15,16]
QUINAPRIL
Quinapril has been extensively studied in the treatment of both hypertension and congestive heart failure. A large, multicenter, placebo-controlled trial[19] found that once-daily quinapril therapy was as efficacious as twice-daily therapy, and both regimens were shown to be significantly more effective than placebo. Hypertensive patients (diastolic blood pressure of 95 to 115 mm Hg) in this single-blinded trial were treated with quinapril in a dosage of 20 mg per day for the first four weeks, 40 mg per day for the next four weeks and 80 mg per day for weeks 8 to 12. The response rate for 40 mg of quinapril was greater than 50 percent (average decrease in diastolic blood pressure of 10 to 12 mm Hg). The response rate for 80 mg of quinapril was greater than 65 percent (average decrease in diastolic blood pressure of 12 to 13 mm Hg). The response rate for placebo was 20 percent (average decrease in diastolic blood pressure of 7 mm Hg). There were no significant differences between one- and twice-daily dosing.
A second study[20] compared quinapril with enalapril in the treatment of mild to moderate hypertension. Patients were started on either drug in a dosage of 10 mg per day. Responders were defined as those in whom diastolic blood pressure decreased to 90 mm Hg or less or decreased from their baseline level by 10 mm Hg. Dosages were doubled at four-week intervals in nonresponders. Patients who still did not respond after 12 weeks of ACE therapy were also given hydrochlorothiazide in a dosage of 25 mg per day. No differences were noted between quinapril and enalapril - either alone or in combination with hydrochlorothiazide - in the degree of response achieved (decrease in diastolic blood pressure) or in the response rate.
In this study, adverse effects were reported by 40 percent of the patients who received enalapril and by 31 percent of those who received quinapril. However, none of the side effects were reported as being severe. Headache, cough and dizziness were the most common adverse effects in each group. Differences in symptoms between the two groups were not statistically significant.
Finally, the efficacy of quinapril, 10 to 40 mg twice daily, was compared with the efficacy of captopril, 25 to 100 mg twice daily, in 172 patients with moderate to severe hypertension (diastolic blood pressure of 110 to 120 mm Hg).[21] Overall response rates, degrees of response and adverse effect profiles did not differ significantly between the treatment groups.
Quinapril has also been studied in a large group of patients with NYHA class II or III congestive heart failure.[22] Dosages of 5 to 20 mg twice daily resulted in significant improvement in exercise tolerance. The response rate, defined as "improved exercise tolerance," was greater for class III patients (70 percent) than for class II patients (28 percent). Side effects, with the exception of a 3 percent incidence of cough, were not significantly different than side effects reported with placebo. In a follow-up open-label trial,[22] the overall response rate, defined as 20 percent improvement or normalization of exercise tolerance, was 60 percent. In 71 percent of patients, a dosage of only 5 mg twice daily was required to maintain effectiveness.
Quinapril was compared with digoxin in a double-blind, crossover study of patients with NYHA class II congestive heart failure who were already receiving 25 mg of hydrochlorothiazide per day.[23] Quinapril, 5 to 10 mg administered twice daily, resulted in a significant decrease in blood pressure and an improvement in exercise tolerance, whereas digoxin therapy resulted in mildly increased blood pressure and no significant change in exercise tolerance. The addition of digoxin produced no further improvement in patients who were taking effective doses of quinapril.
In another study, Banas[24] demonstrated a decrease of one to two NYHA classes in patients with congestive heart failure who were treated for 16 weeks with an average of 10 to 15 mg of quinapril per day, given in divided doses.
RAMIPRIL
The effectiveness of ramipril in mild to moderate hypertension has been evaluated in several multicenter trials. Once such double-blind study[25] showed that the response rates after six weeks of therapy (63 to 77 percent) were significantly higher than those after two weeks of therapy (30 to 49 percent), even when the same doses (1.25 mg, 2.5 mg and 5 mg) were used. No placebo controls were used in the study. These results were confirmed in a second large multicenter trial[26] in which 216 patients received ramipril in dosages ranging from 2.5 to 10 mg per day.
Witte and Walter[27] compared the effectiveness of ramipril with the effectiveness of captopril in 248 patients who had a diastolic blood pressure of 95 to 120 mm Hg. After six weeks, 65 percent of the subjects in each group had normal blood pressure. Hydrochlorothiazide, 50 mg per day, was added to the regimen in nonresponders, but the ACE inhibitor dosage was not changed. At the end of 12 weeks, the response rates in patients receiving ramipril and those receiving captopril were not significantly different. No placebo controls were used in this study. Side effects occurred in 7 percent of the study subjects who received ACE inhibitors alone and in 10 to 12 percent of those who were also given hydrochlorothiazide.
In another trial,[28] ramipril (5 or 10 mg per day) was compared with enalapril (10 or 20 mg per day). Both drugs were given with and without a diuretic. No differences in response rates for ramipril and enalapril were noted when the drugs were given without a diuretic (55 and 59 percent, respectively) or when they were given with a diuretic (73 and 76 percent, respectively).
Kaneko and co-workers[29] have noted no difference between once- and twice-daily dosing of ramipril.
A seven-week trial[30] of ramipril therapy in patients with NYHA class III or IV congestive heart failure demonstrated a decrease in the mean NYHA class from 3.4 to 1.8, with improvements noted in each of the 11 patients studied. Some patients displayed an increase in exercise tolerance and needed a markedly decreased dose of furosemide, although the averages for the whole group showed no significant change in these parameters.
In other studies,[31,32] improvement in patients with congestive heart failure following ramipril therapy was comparable to that achieved with captopril. The adverse effects of ramipril and captopril were similar. However, the adverse effects of ramipril lasted three times longer than the adverse effects of captopril.[31]
Elimination
The elimination of benazepril, quinapril and ramipril, like that of the older ACE inhibitors, is almost exclusively renal.[33,34] The clearance of these drugs has been shown to change in a linear fashion with creatinine clearance. Consequently, it is recommended that the dosages of these drugs be decreased in patients with a creatinine clearance of less than 30 mL per minute.
The elimination route of fosinopril is different from that of the other new ACE inhibitors. Almost half of a dose of fosinoprilat, the active form of fosinopril, is found in the feces, which indicates a non-renal clearance route for this agent.[35] In patients with varying degrees of renal failure, hepatic clearance increases as renal clearance decreases, so that little, if any, accumulation occurs.[36]
In an open-label study[37] of fosinopril, enalapril and lisinopril in 29 patients with a creatinine clearance of less than 30 mL per minute, peak drug concentrations and accumulations on day 1 and day 10 were significantly lower for fosinopril than they were for enalapril and lisinopril. Creatinine clearance (as a measure of renal function) was not altered in any of those patients. Consequently, investigators recommend that the dosage of fosinopril does not need to be altered, even in patients with severe renal failure or in elderly patients with declining renal function.[38]
Adverse Effects
Most of the information about the adverse effects of ACE inhibitors has been derived from experience with captopril and enalapril in treating large numbers of patients with hypertension. The side effect and safety profiles of ACE inhibitors continue to be excellent.
Class-specific side effects of ACE inhibitors include symptomatic hypotension (especially in patients with volume or salt depletion), dizziness, headache, fatigue and cough. Cough had emerged as the most common side effect, with an incidence as high as 25 percent in some studies.[39,40] Angioedema is an infrequent but serious class-related phenomenon, with an incidence of 0.1 to 0.2 percent.[41]
Side effects thought to be related to the sulfhydryl group of captopril include rash and taste disturbances. Rarely, neutropenia occurs in patients receiving captopril.
It is expected that the newer agents will have the same class-specific side effects as the other ACE inhibitors. Heart rate was monitored in many of the studies and was found not to change[11,15,17,21,22,25] or to decrease slightly with any of the ACE inhibitors studied.[18,27] No major alterations were noted in renal function,[12,15,19,22,25,27,32,36] although serum creatinine levels were found to be mildly elevated in some patients.[17,20] However, renal function should be monitored in all patients treated with ACE inhibitors.
As a class, ACE inhibitors should not be used during pregnancy. All of these agents must carry a warning that use in the second and third trimesters could result in injury or death in the developing fetus.
Cost
At the recommended starting doses, there is little difference in the costs of the currently available agents (Table 2). However, at moderate to high doses, the new agents may be considerably less expensive.
[TABULAR DATA OMITTED]
Final Comment
ACE inhibitors are effective and popular agents in the treatment of hypertension, although no long-term data currently demonstrate a decrease in morbidity and mortality with their use (as exist for some other agents, such as diuretics and beta-adrenergic receptor blockers). In particular, the ACE inhibitors are widely used in hypertensive patients with coexisting congestive heart failure or diabetes mellituts. These agents also offer many benefits in the treatment of congestive heart failure, alhough their exact role is still being defined.
The four new ACE inhibitors appear to be as effective as their older counterparts. However, they have not yet been proven to offer any major clinical advantages over previously available agents, with the possible exception of once-daily dosing.
REFERENCES
[1.] The 1988 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med 1988;148:1023-38. [2.] CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med 1987;316-1429-35. [3.] The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 1991;325:293-302. [4.] Kramer BL, Massie BM, Topic N. Controlled trial of captopril in chronic heart failure: a rest and exercise hemodynamic study. Circulation 1983;67:807-16. [5.] Awan NA, Amsterdam EA, Hermanovich J, Bommer WS, Needham KE, Mason DT. Long-term hemodynamic and clinical efficacy of captopril therapy in ambulatory management of severe chronic congestive heart failure. Am Heart J 1982;103(4 Pt 1):474-9 [6.] Awan NA, Evenson MK, Needham KE, Win A, Mason DT. Efficacy of oral angiotensin-converting enzyme inhibition with captopril therapy in severe chronic normotensive congestive heart failure. Am Heart J 1981;101:22-31. [7.] Ader R, Chatterjee K, Ports T, Brundage B, Hiramatsu B, Parmley W. Immediate and sustained hemodynamic and clinical improvement in chronic heart failure by an oral angiotensin-converting enzyme inhibitor. Circulation 1980;61:931-7. [8.] Cohn JN, Johnson G, Ziesche S, Cobb F, Francis G, Tristani F, et al. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med 1991;325:303-10. [9.] Chatterjee K, Parmley WW, Cohn JN, Levine TB, Awan NA, Mason DT, et al. A cooperative multicenter study of captopril in congestive heart failure: hemodynamic effects and long-term response. Am Heart J 1985;110:439-47. [10.] Top 200. Am Drug 1993;207:49-53. [11.] Valvo E, Casagrande P, Bedogna V, Antiga L, Alberti D, Zamboni M, et al. Systemic and renal effects of a new angiotensin converting enzyme inhibitor, benazepril, in essential hypertension. J Hypertens 1990;8:991-5. [12.] Moser M, Abraham PA, Bennett WM, Brachfeld N, Goodman RP, McKenney JM, et al. The effects of benazepril, a new angiotensin-converting enzyme inhibitor, in mild to moderate essential hypertension: a multicenter study. Clin Pharmacol Ther 1991;49:322-9. [13.] Gomez HJ. Dose-response studies with benazepril in mild to moderate hypertension. Clin Cardiol 1991;14(8 Suppl 4):IV22-7. [14.] Mirvis DM, Insel J, Boland MJ, Cinquegrani MP, Ghali, JK, Rubin SA, et al. Chronic therapy for congestive heart failure with benazepril HCl, a new angiotensin converting enzyme inhibitor. Am J Med Sci 1990;300;354-60. [15.] Anderson, RJ, Duchin KL, Gore RD, Herman TS, Michaels RS, Nichola PS, et al. Once-daily fosinopril in the treatment of hypertension. Hypertension 1991;17:636-42. [16]. Pool JL. Antihypertensive effect of fosinopril, a new angiotensin converting enzyme inhibitor: findings of the Fosinopril Study Group II. Clin Ther 1990;12-520-33. [17.] Goldstein RJ, Angelo JE, Ferraro LA, Gilderman LI, Zinny MA, et al. Multicenter, randomized, double-blind, parallel comparison of fosinopril sodium and enalapril maleate for the treatment of mild-to-moderate essential hypertension. Drug Invest 1991;3(Suppl 4):38-44. [18.] Clementy J, Auboiron, J, Araud JM, Ballan G, Texier JF, et al. Double-blind, randomized study of fosinopril vs nifedipine SR in the treatment of mild-to-moderate hypertension in elderly patients. Drug Invest 1991;3 (Suppl 4):45-53. [19.] Maclean D. Quinapril: a double-blind, placebo-controlled trial in essential hypertension. Angiology 19889;40(4 Pt 2):370-81. [20.] Taylor SH. A comparison of the efficacy and safety of quinapril with that of enalapril in the treatment of milk to moderate essential hypertension. Angiology 1989;40(4 Pt 2):382-2. [21.] Schnaper HW. Comparison of the efficacy and safety of quinapril v.s captopril in treatment of moderate to severe hypertension. Angiology 1989;40(4 Pt 2):389-95. [22.] Riegger GA. Effects of quinapril on exercise tolerance in patients with mild to moderate heart failure. Eur Heart J 1991;12:705-11. [23.] Kromer EP, Elsner D, Riegger GA. Digoxin, converting-enzyme inhibition (quinapril), and the combination in patients with congestive heart failure functional class II and sinus rhythym. J Cardiovasc Pharmacol 1990:6(1):9-14. [24.] Banas JS Jr. Preliminary hemodynamic report of the efficacy and safety of quinapril in acute and chronic treatment of patients with congestive heart failure. Angiology 1989;40(4 Pt 2):396-404. [25]. Walter U, Forthofer R, Witte PU. Dose-response relation of the angiotensin converting enzyme inhibitor ramipril in mild to moderate essential hypertension. Am J Cardiol 1987;59:125D-132D. [26.] Kostin JB. Double blind study of ascending doses of ramipril in patients with mild-to-moderate hypertension. Adv Ther 1991;8:6-17. [27.] Witte PU, Walter U. Comparative double-blind study of ramipril and captopril in mild to moderate essential hypertension. Am J Cardiol 1987;59:115D-120D. [28.] Zabludowski, J, Rosenfeld J, Akbary MA, Rangoonwala B, Schinzel S. A multi-centre comparative study between ramipril and enalapril in patients with mild to moderate essential hypertension. Curr Med Res Opin 1988;11:93-106. [29.] Kaneko Y, Omae T, Yoshinaga K, Iimura O, Inagaki Y, Ishii M, et al. Effect of ramipril, a new angiotensin converting enzyme inhibitor, on diurnal variations of blood pressure in essential hypertension. Am J Cardiol 1987;59;86D-91D. [30.] Crozier IG, Ikram H, Nicholls MG, Jans S. Global and regional hemodynamic effects of ramipril in congestive heart failure. J Cardiovasc Pharmacol 1989;14:688-93. [31.] de Graeff PA, Kingma JH, Viersma JW, Wesseling H, Lie KI. Acute and chronic effects of ramipril and captopril in congestive heart failure. Int J Cardiol 1989;23:59-67. [32.] Manthey J, Osterzil KJ, Rohrig N, Dietz R, Hackenthal E, Schmidt-Gayk H, et al. Ramipril and captopril in patients with heart failure: effects on hemodynamics and
vasoconstrictor systems. Am J Cardiol 1987;59:171D-175D. [33.] Kaiser G, Ackermann R, Sioufi A. Pharmacokinetics of a new angiotension-converting enzyme inhibitor, benazepril hydrochloride, in special populations. Am Heart J 1989;117:46-51. [34.] Begg EJ, Robson RA, Bailey RR,Lynn KL, Frank GJ, Olson SC. The pharmacokinetics and pharmacodynamics of quinapril and quinaprilat in renal impairment. Br J Clin Pharmacol 1990;30:213-20. [35.] Singhvi SM, Duchin KL, Morrison RA, Willard DA, Everett DW, Frantz M. Disposition of fisonopril sodium in healthy subjects. Br J Clin Pharmacol 1988;25:9-15. [36.] Hui KK, Duchin KL, Kripalani KJ, Chan D, Kramer PK, Yanagawa N. Pharmacokinetics of fosinopril in patients with various degrees of renal function. Clin Pharmacol Ther 1991;49:457-67. [37.] Sica DA, Cutler RE, Parmer RJ, Ford NF. Comparison of the steady-state pharmacokinetics of fosinopril, lisinopril an enalapril in patients with chronic renal insufficiency. Clin Pharmacokinet 1991;20-420-7. [38.] Duchin KL, Kripalani KJ, MR, Dean AV, Natarajan CS. Review of the pharmacokinetics of fosinopril in special populations. Drug Invest 1991;3(Suppl 4):18-24. [39.] Simon SR, Black HR, Moser M, Berland WE. Cough and ACE inhibitors. Arch Intern Med 1992;152: 1698-700. [40.] Goldszer RC, Lilly LS, Solomon HS. Prevalence of cough during angiotensin-converting enzyme inhibitor therapy. Am J Med 1988;85:887. [41.] Roberts JR, Wuerz RC. Clinical characteristics of angiotensin-converting enzyme inhibitor-induced angioedema. Ann Emerg Med 1991;20-555-8.
COPYRIGHT 1993 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group