IN THIS ARTICLE, you'll learn about nine new drugs marketed in the first half of 2003, including:
* adalimumab, given once every other week for rheumatoid arthritis (RA)
* eletriptan hydrobromide, a new option for treating acute migraine and associated symptoms
* atomoxetine HCl, an important new type of medication for children and adults with attention deficit hyperactivity disorder (ADHD)
* alefacept, the first biologic therapy for moderate or severe psoriasis.
Unless otherwise specified, the information in the following summaries applies to adults, not children. Consult the package insert for information about each drug's safety during pregnancy and breast-feeding. Also consult the package insert, a pharmacist, or a comprehensive drug reference for more details on precautions, drug interactions, and adverse reactions* for all these drugs.
The author has disclosed that he has no significant relationship with or financial interest in any commercial companies that pertain to this educational activity.
Antiarthritic drug
Adalimumab
Given once every other week to reduce symptoms and slow progression of rheumatoid arthritis
Endogenous cytokines such as tumor necrosis factor (TNF) are important mediators of inflammation and joint destruction in patients with rheumatoid arthritis (RA). Adalimumab (Humira, Abbott), the newest recombinant monoclonal antibody that targets TNF, is derived from human cells. Like infliximab, it binds specifically to TNF-alpha, reducing symptoms and progression of structural joint damage for patients with moderately to severely active RA who've had an inadequate response to one or more disease-modifying antirheumatic drugs (DMARDs), such as methotrexate. It may be used alone or in combination with other DMARDs.
Like etanercept, another TNF inhibitor, adalimumab is administered subcutaneously (S.C.) and may be self-administered by the patient. But adalimumab's longer dosage interval-the usual recommendation is one injection every other week-makes it more convenient than etanercept, which has been administered twice a week but has recently been approved for once-a-week administration. Another advantage is that adalimumab is supplied in prefilled syringes for easier administration by patients who may be disabled by arthritis.
Adalimumab and the other TNF inhibitors alter immune defenses, raising the risk of infections and certain cancers. Patients with active RA taking TNF inhibitors are at particular risk for developing lymphomas, although the role of TNF inhibitors as a cause or a contributing factor hasn't been established.
Although RA is currently the only labeled indication for adalimumab, researchers are evaluating it as a treatment for other disorders, such as Crohn's disease, polyarticular-course juvenile RA, psoriatic arthritis, and ankylosing spondylitis.
Precautions: (1) Don't use adalimumab in patients with active infections. (2) Because tuberculosis has been associated with use of TNF inhibitors, make sure patients are tested for active or latent tuberculosis before starting treatment. (3) Use cautiously in patients with preexisting or recent-onset central nervous system demyelinating disorders. (4) Don't give live vaccines concurrently with TNF inhibitors. (5) Discontinue therapy if symptoms suggestive of a lupuslike syndrome develop. Some patients have developed autoantibodies from TNF inhibitor therapy.
Adverse reactions: injection-site reactions, headache, rash, upper respiratory infection, sinusitis
Supplied as: prefilled syringes and vials containing 40 mg of adalimumab
Dosage: 40 mg S.C. injection once every other week
Nursing considerations: (1) Teach the patient to notify her health care provider if she develops an infection during treatment. If the infection is serious, adalimumab treatment should be stopped until the infection is treated and eradicated. (2) If adalimumab is used as monotherapy, the health care provider may prescribe once-weekly injections for a better response. (3) Tell the patient to store adalimumab in the refrigerator, but not to freeze it.
Antiparasitic drug
Nitazoxanide
New treatment for dangerous diarrhea in children
Nitazoxanide (Alinia, Remark) is an antiprotozoal drug indicated to treat diarrhea caused by Cryptospondium parvum and Giardia lamblia in children ages 1 to 11. It's the first drug approved specifically for cryptosporidiosis and the only drug approved for giardiasis in children that's available in liquid form.
Cryptosporidiosis is characterized by diarrhea, abdominal cramps, loss of appetite, low-grade fever, nausea, and vomiting. It's usually self-limiting in healthy children, but it can be prolonged and life-threatening in those who are immunocompromised from such conditions as human immunodeficiency virus (HIV) infection.
Giardiasis, which is usually contracted from drinking contaminated water, causes diarrhea, abdominal cramps, bloating, weight loss, and malabsorption. The standard treatment is a 5-day course of metronidazole (Flagyl), although this isn't a labeled indication for the drug. In clinical trials, nitazoxanide was similarly effective when given as a 3-day course of treatment.
Nitazoxanide was well tolerated in trials. Most adverse reactions were mild and transient.
Precautions: (1) Use cautiously in children with hepatic, biliary, or renal disease. (2) The potential for competition for protein binding sites exists when nitazoxanide is used concurrently with other drugs that are also highly protein-bound. This can cause a shift in plasma drug concentrations and increase the potential for adverse reactions.
Adverse reactions: abdominal pain, diarrhea, yellow discoloration of the sciera (rare)
Supplied as: a powder; when reconstituted as directed, each 5 ml of suspension contains 100 mg of nitazoxanide
Dosage: For children ages 12 to 47 months: 100 mg every 12 hours for 3 days. For children ages 4 to 11 years: 200 mg every 12 hours for 3 days
Nursing considerations: (1) Administer each dose with food. (2) The suspension may be stored for 7 days at room temperature. (3) Discard any unused portion after 7 days.
Drug for migraine
Eletriptan hydrobromide
Seventh triptan joins the class to fight migraine and associated symptoms.
Eletriptan hydrobromide (Relpax, Pfizer) is the seventh triptan to be marketed for treatment of migraine, joining almotriptan, frovatriptan, naratriptan, rizatriptan, sumatriptan, and zolmitriptan. Classified as selective serotonin receptor agonists, these drugs are all indicated to treat acute migraine with or without aura in adults.
Triptans are thought to act on receptors in the extracerebral, intracranial vessels that become dilated during a migraine attack and on nerve terminals in the trigeminal nerve. Stimulating these receptors constricts cranial vessels, inhibits neuropeptide release, and reduces nerve impulse transmission along trigeminal pain pathways.
Besides relieving headache pain, the triptans also relieve the nausea, vomiting, photophobia, and phonophobia associated with an acute migraine attack. They're not indicated for migraine prophylaxis or for hemiplegic or basilar migraine.
The various triptans are considered similarly effective, although those available in nasal spray or injection formulations take effect faster than oral formulations. (Eletriptan is available only in oral form.) However, because of individual differences, some patients may experience better results with one drug than another.
Precautions: (1) Contraindicated in patients with uncontrolled hypertension, severe hepatic impairment, or ischemic heart disease and in patients with findings consistent with ischemic heart disease, coronary artery vasospasm, or other significant underlying cardiovascular disease. Cardiovascular problems should be ruled out in asymptomatic patients with significant risk factors. (2) Contraindicated in patients with history of cerebrovascular disease, including transient ischemic attacks and stroke. (3) Don't administer within 24 hours of treatment with another triptan or ergot-type medication unless the benefit outweighs the risk of additive vasospastic reactions (for example, when one dose of a triptan doesn't relieve an attack). (4) Use cautiously in patients also taking monoamine oxidase type A inhibitors. Avoid concurrent use if possible. (5) Use cautiously with selective serotonin reuptake inhibitors, such as fluoxetine (Prozac). (6) Don't give within 72 hours of treatment with CYP 3A4 inhibitors such as ketoconazole (Nizoral), itraconazole (Sporanox), nefazodone, clarithromycin, troleandomycin, ritonavir, or nelfinavir; these drugs may increase the action of eletriptan. (7) Use cautiously with other CYP 3A4 inhibitors such as verapamil, which is sometimes prescribed off-label for migraine prophylaxis.
Adverse reactions: dizziness, somnolence, asthenia, dry mouth, paresthesia, and chest or throat tightness, pain, or pressure
Supplied as: 20-mg and 40-mg tablets
Dosage: 40 mg P.O. If headache returns, repeat the dose after 2 hours, to a maximum of 80 mg in 24 hours.
Nursing considerations: (1) Patients who arc intermittent or long-term users of a triptan should be monitored for coronary artery disease (CAD). Triptan use should be discontinued if CAD develops. (2) If a triptan is prescribed for an asymptomatic patient with significant CAD risk factors, give the first dose in a clinical setting and monitor her reaction. (3) Teach her that eletriptan is indicated only for relief of a migraine attack, not migraine prophylaxis. (4) Warn her not to exceed the recommended maximum dosage (no more than 40 mg per single dose or 80 mg in a 24-hour period). (5) Tell her to contact her health care provider if her headaches become more frequent or difficult to control. (6) Remind her not to share eletriptan (or any other drug prescribed for her) with others.
Drug for ADHD
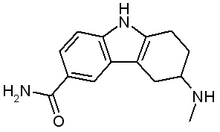
Atomoxetine HCl
Important new drug treats attention deficit hyperactivity disorder in both children and adults.
Approved to treat attention deficit hyperactivity disorder (ADHD) in children, adolescents, and adults, atomoxetine HCl (Strattera, Lilly) is the first drug for ADHD demonstrated to be effective in adults as well as children.
Unlike other drugs prescribed for ADHD, such as amphetamine, dextroamphetamine, methylphenidate (Ritalin), and pemoline (Cylert), it's not a central nervous system stimulant or a controlled substance. A selective norepinephrine reuptake inhibitor, atomoxetine increases the availability of norepinephrine, which is believed to play a role in regulating impulse control, organization of thoughts, and attention.
In clinical studies spanning 9 weeks, patients treated with atomoxetine lost an average of 0.4 kg of body weight; those in the placebo group gained 1.5 kg on average. The effects of atomoxetine on height and weight over time aren't known, so a child's growth should be closely monitored during treatment. The drug's safety and effectiveness for children under age 6 haven't been evaluated.
Because atomoxetine isn't a controlled substance, prescriptions and refills can be more readily obtained. Its an important alternative for patients who don't tolerate stimulants well or who don't want to use a controlled substance.
Precautions: (1) Contraindicated in patients with narrow-angle glaucoma because of an increased risk of mydriasis. (2) Contra-indicated in patients known to be hypersensitive to atomoxetine. (3) Use caution in patients with conditions that predispose them to hypotension because some patients taking atomoxetine have experienced orthostatic hypotension. (4) Use caution in patients with hypertension, tachycardia, or cardiovascular or cerebrovascular disease because atomoxetine may increase blood pressure and heart rate. (5) Contraindicated for concurrent use with a monoamine oxidase inhibitor (MAOI); treatment with an MAOI shouldn't be initiated within 2 weeks of discontinuing atomoxetine. (6) Because atomoxetine is metabolized primarily via the CYP 2D6 enzyme pathway, its activity may be influenced by other drugs that inhibit this pathway. Consult the product insert for information about possible drug interactions that may require a dosage adjustment or other precautions. (7) Reduce the dosage of atomoxetine in patients with moderate to severe hepatic insufficiency.
Adverse reactions: In adults: dry mouth, insomnia, nausea, constipation, decreased appetite, urinary hesitation/retention, dysmenorrhea, erectile disturbance, decreased libido, dizziness. In children and adolescents: upper abdominal pain, vomiting, nausea, fatigue, dyspepsia
Supplied as: 10-mg, 18-mg, 25-mg, 40-mg, and 60-mg capsules
Dosage: variable, depending on the patients age, weight, concurrent medications, and response to treatment. See the package insert for guidelines.
Nursing considerations: (1) Atomoxetine can be taken without regard to food. It can be discontinued without tapering. (2) Because of the potential for dizziness, warn the patient to avoid activities requiring alertness, such as driving, until he learns how the drug affects his performance. (3) Document the patient's blood pressure and pulse at baseline, following dosage increases, and periodically throughout treatment. For a pediatric patient, also monitor growth.
Drug for psoriasis
Alefacept
First biologic therapy for moderate or severe chronic plaque psoriasis
Psoriasis is a chronic, relapsing disease caused by faulty signals in the immune system. Skin cells regenerate too quickly, and, in the most common form of psoriasis, create unsightly plaques that can itch, bleed, and crack and may be painful. The disorder can restrict joint motion and cause emotional distress. Treatments include topical corticosteroids and other topical medication, phototherapy, and, for severe cases, chemophototherapy and various systemic drugs.
Alefacept (Amevive, Biogen) is the first biologic therapy approved to treat psoriasis. Biologic therapy stimulates or restores the immune systems ability to fight disease. An immunosuppressive drug given parenterally, alefacept interferes with the activation of psoriasis-related T cells.
Alefacept is indicated for adults with moderate to severe chronic plaque psoriasis who are candidates for systemic therapy or phototherapy. Although clinical response to the drug may take 2 months to develop, it may produce longer remissions than other treatments.
Alefacept was approved for both intramuscular (I.M.) and intravenous (I.V.) use, but because it's nearly always given I.M., the manufacturer is discontinuing the I.V. formulation. Alefacept is distributed by AmerisourceBergen and Priority Healthcare through a restricted program.
Precautions: (1) Don't give to patients with subnormal CD4+ T lymphocyte counts, serious infections, or a history of systemic cancer. (2) Use caution when administering alefacept to patients at high risk for cancer and those with chronic or recurrent infections. (3) Discontinue alefacept if the patient develops a serious infection or hypersensitivity reaction. (4) Withhold or discontinue treatment if lymphocyte levels drop below recommended levels (see product insert for guidelines). (5) Avoid concurrent use with other immunosuppressive therapies.
Adverse reactions: pharyngitis, cough, dizziness, nausea, pruritus, myalgia, injection-site pain and inflammation, chills (mainly with I.V. injection)
Supplied as: single-use vials of lyophilized powder containing 15 mg of the drug for I.M. administration
Dosage: 15 mg I.M. once a week for 12 weeks
Nursing considerations: (1) Rotate injection sites and administer new injections at least 1 inch (2.5 cm) from the last site. Avoid areas where the skin is tender, bruised, red, or hard, including areas affected by psoriasis. (2) Store alefacept at room temperature and protect it from light. (3) Reconstitute the powder with 0.6 ml of sterile water for injection (supplied with the medication). Swirl the vial gently but don't shake it. (4) Administer the medication immediately after reconstitution or refrigerate it and administer within 4 hours. Discard reconstituted medication if it's not administered within 4 hours. (5) Monitor the patient's CD4+ T lymphocyte count weekly during therapy. (6) The prescriber may order a second 12-week course of therapy if the patient's CD4+ T lymphocyte counts are within normal limits and at least 12 weeks have passed since the previous course of treatment. (7) Alefacept is classified in Pregnancy Category B and shouldn't be used during pregnancy unless the benefits clearly outweigh the risks. Women who become pregnant while taking alefacept or within 8 weeks of discontinuing it should be enrolled in the Biogen Pregnancy Registry (1-866-263-8483). (8) The safety and effectiveness of vaccines for patients taking alefacept isn't known.
Depigmenting drug
Mequinol
Wiping away age spots
Solar lentigines, also known as age spots or liver spots, are localized, pigmented, macular lesions that occur on skin chronically exposed to sunlight. Mequinol (Solage, Galderma), a topical solution consisting of the monomethyl ether of hydroquinone and the retinoid tretinoin, is indicated for topical treatment of solar lentigines in conjunction with a comprehensive skin care and sun-avoidance program. Mequinol is available only in combination with tretinoin.
Although the mechanism isn't fully understood, mequinol may inhibit the formation of melanin precursors. It's not a cure, and after ending treatment, most patients experience some repigmentation over time. Its effectiveness and safety in patients with dark skin haven't been established.
The mequinol/tretinoin solution causes dermal irritation and may cause burns if the treated skin is exposed to sunlight or sunlamps. During treatment, patients must comply with a sunavoidance program and wear protective clothing outdoors.
Precautions: (1) Contra-indicated in children, pregnant women, and women of childbearing potential. (2) Don't use in patients with sunburn, eczema, or any condition involving chronic skin irritation or inflammation. (3) Don't use in patients with a personal or family history of vitiligo. (4) Don't use concurrently with a medication known to cause photosensitivity, such as tetracyclines, fluoroquinolones, sulfonamides, and thiazides.
Adverse reactions: skin irritation, erythema, burning, stinging, tingling, desquamation, pruritus, halo hypopigmentation of surrounding skin, temporary hypopigmentation of treated lesions
Supplied as: a topical solution of 2% mequinol and 0.01% tretinoin in 77.8% ethyl alcohol
Dosage: apply twice daily, morning and evening, at least 8 hours apart
Nursing considerations: (1) Tell the patient to avoid or minimize exposing treated areas of skin to sunlight, including sunlamps, because of the greater potential for sunburn. (2) Protect the bottle from light by storing it in the carton after opening. Because the solution is flammable, keep it away from heat and open flame. (3) Teach the patient to apply the solution to lesions using the applicator tip and to avoid applying it to surrounding skin, eyes, mouth, paranasal creases, and mucous membranes. (4) Tell her not to shower or bathe the treated area for at least 6 hours after applying the solution. However, she may apply cosmetics after 30 minutes. (5) Teach her to avoid other skin products or treatments that have a strong drying effect, such as products with a high alcohol content, astringents, spices or limes, medicated soaps and shampoos, permanent wave solutions, electrolysis, and hair depilatories or waxes. (6) Tell her that she should see improvement within 24 weeks. She should stop treating any skin areas that become the same color or lighter than surrounding skin.
Antineoplastic drug
Gefitinib
Oral drug receives accelerated approval as a treatment for lung cancer.
Non-small-cell lung cancer (NSCLC), the most common kind of lung cancer, usually expresses normal or high quantities of epidermal growth factor receptor (EGFR), which is thought to stimulate the growth and proliferation of cancer cells. Gefitinib (Iressa, Astra-Zeneca) appears to selectively inhibit the tyrosine kinases associated with EGFR and is the first antineoplastic drug with this mechanism of action approved by the Food and Drug Administration (FDA).
Gefitinib is indicated for monotherapy in patients with locally advanced or metastatic NSCLC after failure of first-line treatment with both platinum-based and docetaxel chemotherapies. An oral drug, gefitinib was approved under the FDA's accelerated approval process based on its ability to shrink tumors in clinical trials. However, considerable variation in response occurred among patient subgroups. For example, the response rate was about 18% in women versus 5% in men, and 29% in nonsmokers versus 5% in current or previous smokers. For unknown reasons, gefitinib wasn't effective when combined with other chemotherapies, and it's not indicated for first-line use or as part of combination therapy.
Unlike many chemotherapeutic drugs, gefitinib isn't likely to cause myelosuppression or alopecia. However, it may cause interstitial lung disease (ILD), which is potentially fatal. Characterized by acute onset of dyspnea, possibly accompanied by cough and fever, ILD can worsen quickly. If the patient develops sudden new or rapidly worsening pulmonary symptoms, treatment should be interrupted and the symptoms evaluated.
Precautions: (1) Monitor the patient for signs and symptoms of ILD and discontinue gefitinib therapy if ILD is confirmed. (2) Because gefitinib is metabolized by the liver, monitor liver function tests and discontinue treatment if marked elevations occur. (3) Use cautiously with drugs that inhibit or induce the CYP 3A4 metabolic pathway, such as itraconazole, ketoconazole, phenytoin (Dilantin), and rifampin (Rifadin). Gefitinib undergoes extensive hepatic metabolism, and these drugs may affect its metabolism. See the product insert for details on these and other possible drug interactions.
Adverse reactions: diarrhea, rash, acne, dry skin, nausea, vomiting, amblyopia (vision reduction or dimness), conjunctivitis
Supplied as: 250-mg film-coated tablets
Dosage: 250 mg once a day
Nursing considerations: (1) Tell the patient that she can take gefitinib without regard to food. (2) Teach her to call her health care provider immediately if she suddenly develops shortness of breath, fever, or any new pulmonary symptoms while taking gefitinib. (3) Some patients taking warfarin (Coumadin) concurrently have experienced international normalized ratio (INR) elevations and bleeding. If your patient is taking warfarin concurrently, closely monitor her INR. (4) Some patients taking gefitinib have experienced eye pain, corneal erosions or ulcers, and aberrant eyelash growth. Instruct the patient to contact her health care provider if she experiences eye pain. (5) If she experiences intolerable dermatologic adverse reactions or diarrhea, tell her to inform her health care provider. He may help her manage symptoms by interrupting therapy for up to 14 days. (6) Warn her not to exceed the recommended dosage.
Drug for Fabry disease
Agalsidase beta
Orphan drug is the first approved for this rare genetic disorder.
Fabry disease, a serious genetic disorder of glycosphingolipid metabolism, affects about 1 in 40,000 men. (Although women may also be affected, they typically don't experience severe symptoms.) A deficiency of alpha-galactosidase A results in progressive accumulation of glycosphingolipids in body tissues, impairing vascular, renal, cardiac, autonomic, and central nervous system function. Most patients die in their 40s or 50s.
Agalsidase beta (Fabrazyme, Genzyme), the first drug approved for Fabry disease, is a recombinant human alpha-galactosidase A enzyme. The drug was approved by the FDA under the accelerated approval mechanism.
The drug is supplied as a lyophilized powder or cake in single-use vials containing 35 mg of agalsidase beta. Following reconstitution and dilution, administer agalsidase beta by I.V. infusion-1 mg/kg every 2 weeks. See the product insert for details about reconstituting and diluting the drug, calculating the dosage, and titrating the infusion rate.
Adverse reactions to agalsidase beta include infusion reactions (fever, rigors, chest pain or tightness, headache, hypotension, hypertension, nausea), pruritus, myalgia, dyspnea, urticaria, and abdominal pain.
To prevent or minimize transfusion reactions, which may be severe, pretreat the patient with an antipyretic, antihistamine, or corticosteroid, as directed. If a transfusion reaction occurs, slow or stop the infusion as indicated and intervene appropriately. Although transfusion reactions tend to lessen with continued treatment, serious reactions can occur even after extended treatment. Closely monitor patients with cardiac problems, who may be at greater risk for severe complications if a transfusion reaction occurs.
Store the vials in the refrigerator. Let the vial reach room temperature by leaving it out for about 30 minutes before administering the drug; don't heat or microwave it. Give the reconstituted drug immediately if possible, or within 24 hours if it's stored in the refrigerator.
Agalsidase beta is supplied through a restricted distribution program by TheraCom and Accredo Health. The cost of treatment is at least $175,000/year for a patient weighing 154 pounds (70 kg). Because of the small number of patients who are candidates for the treatment, a registry program has been established to evaluate its long-term performance. Information is available at 1-800-745-4447 or http:// www.fabryregistry.com.
Drug for MPS I
Laronidase
Help for children with a debilitating enzyme deficiency
Mucopolysaccharidosis I (MPS I) is a rare genetic disorder characterized by a deficiency of alpha-L-iduronidase. This enzyme deficiency allows glycosaminoglycan substrates to accumulate, causing widespread cellular, tissue, and organ dysfunction that can affect appearance, physical abilities, and sometimes mental development.
Children with the most severe form, called Hurler syndrome, die before age 10 from cardiac and respiratory complications. Those with Hurler-Scheie syndrome, a less severe form of MPS I, may survive into their 20s. Those with the mildest form, Scheie syndrome, may live well into adulthood but can still experience breathing problems, heart disease, and deformities.
Laronidase (Aldurazyme, Genzyme), a version of alpha-L-iduronidase produced by recombinant DNA technology, is indicated for patients with Hurler and Hurler-Scheie syndromes and for patients with Scheie syndrome who have moderate to severe symptoms. The drug improves pulmonary function and walking capacity and reduces liver size and urinary glycosaminoglycan concentrations.
Laronidase is supplied as single-use vials containing 2.9 mg of the drug in 5 ml of solution. This solution must be diluted with 0.1% albumin (human) in 0.9% sodium chloride injection. Administer the reconstituted drug I.V over 3 to 4 hours once a week, as directed. Consult the product insert for details about reconstituting the drug, calculating the dosage, and titrating the infusion rate.
Store the vials in the refrigerator. Before use, let the vial reach room temperature, but don't heat or microwave it. Prepare the drug using polyvinyl chloride (PVC) containers and administer it with a PVC infusion set equipped with an in-line, low-protein-binding 0.2-micrometer filter. Don't use a filter needle to draw up the dose and avoid excessively agitating the solution during handling or administration.
Give the reconstituted solution immediately if possible or store it in a refrigerator. No more than 36 hours should elapse between preparation and completion of administration.
Adverse reactions to laronidase include infusion-related reactions (flushing, fever, headache, and rash), upper respiratory tract infection, injection-site reaction, paresthesia, and hyperreflexia. To prevent or minimize transfusion reactions, premedicate the patient with an antipyretic and an antihistamine. The frequency of transfusion reactions tends to decrease with continued use of the drug.
If the patient develops a hypersensitivity reaction, slow or stop the infusion or administer additional antihistamines. If he has a severe reaction, stop therapy and initiate appropriate therapy. However, use epinephrine with caution because of the prevalence of heart disease in patients with MPS I. The frequency of transfusion reactions decreases with continued use of the drug.
Laronidase is supplied through a restricted distribution program by TheraCom and Accredo Health. Because of the small number of patients who are candidates for the treatment, a registry program has been established to evaluate its long-term performance. Information is available at 1-800-745-4447 or http:// www.mpsiregistry.com.
CE Test
New drugs04, part 1
Instructions:
* Read the article beginning on page 56.
* Take the test, recording your answers in the test answers section (Section B) of the CE enrollment form. Each question has only one correct answer.
* Complete registration information (Section A) and course evaluation (Section C).
* Mail completed test with registration fee to: Lippincott Williams & Wilkins, CE Dept., 16th Floor, 345 Hudson St., New York, NY 10014.
* Within 3 to 4 weeks after your CE enrollment form is received, you will be notified of your test results.
* If you pass, you will receive a certificate of earned contact hours and an answer key. If you fail, you have the option of taking the test again at no additional cost.
* A passing score for this test is 30 correct answers.
* Need CE STAT? Visit http://www.nursingcenter.com for immediate results, other CE activities, and your personalized CE planner tool.
* No Internet access? Call 1-800-933-6525, ext. 331 or ext. 332, for other rush service options.
* Questions? Contact Lippincott Williams & Wilkins: 212- 886-1331 or 212-886-1332.
Registration Deadline: February 28, 2006
Provider Accreditation:
This Continuing Nursing Education (CNE) activity for 3.0 contact hours and 3.0 pharmacology contact hours is provided by Lippincott Williams & Wilkins, which is accredited as a provider of continuing education in nursing by the American Nurses Credentialing Center's Commission on Accreditation and by the American Association of Critical-Care Nurses (AACN 11696, CERP Category O). This activity is also provider approved by the California Board of Registered Nursing, Provider Number CEP 11749 for 3.0 contact hours and 3.0 pharmacology contact hours. LWW is also an approved provider of CNE in Alabama, Florida, and Iowa and holds the following provider numbers: AL #ABNP0114, FL #FBN2454, IA #75. All of its home study activities are classified for Texas nursing continuing education requirements as Type I.
Your certificate is valid in all states. This means that your certificate of earned contact hours is valid no matter where you live.
Payment and Discounts:
* The registration fee for this test is $19.95.
* If you take two or more tests in any nursing journal published by LWW and send in your CE enrollment forms together, you may deduct $0.75 from the price of each test.
* We offer special discounts for as few as six tests and institutional bulk discounts for multiple tests. Call 1-800-933-6525, ext. 332, for more information.
* Common adverse reactions are italicized throughout this article.
SELECTED REFERENCES
Drug Facts and Comparisons. St. Louis, Mo., Facts and Comparisons, Inc., 2004.
Nursing2004 Drug Handbook. Springhouse, Pa., Lippincott Williams & Wilkins, 2004.
Physicians' Desk Reference, 58th edition. Montvale, N.J., Medical Economics, 2004.
BY DANIEL A. HUSSAR, PHD
Remington Professor of Pharmacy
Philadelphia College of Pharmacy * University of the Sciences in Philadelphia, Pa.
Copyright Springhouse Corporation Feb 2004
Provided by ProQuest Information and Learning Company. All rights Reserved