Although cerebrospinal fluid (CSF) cultures become sterile within 24 to 48 hours after the initiation of appropriate antibiotic therapy for meningitis, neurologic sequelae and mortality rates remain high. Animal studies have demonstrated that antibiotic-induced bacterial lysis leads to inflammation, which may produce unfavorable outcomes. The use of corticosteroids in the treatment of acute bacterial meningitis has been widely investigated in children, but not in adults. Researchers de Gans and van de Beek present data from a multicenter European trial of dexamethasone in adults with bacterial meningitis.
Patients were enrolled in the study if they were at least 17 years of age and had suspected meningitis and bacteria in CSF on Gram stain or a CSF leukocyte count of more than 1,000 per [mm.sup.3] (1 3 [10.sup.9] per L). Patients who had received any antibiotic therapy in the previous 48 hours were excluded from the study.
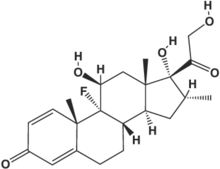
A total of 301 subjects were randomized to receive intravenous dexamethasone in a dosage of 10 mg every six hours for four days (n = 157) or placebo (n = 144). The first steroid dose was given 15 to 20 minutes before or with the first dose of antibiotic. Favorable outcomes were defined as a score of 5 on the Glasgow Outcome Scale, and mild or no disability (the patient is able to return to work or school) at follow-up examination by the patient's physician eight weeks after randomization. Early withdrawal from the assigned treatment or loss of follow-up occurred in 29 patients. The authors used the last available observation scores on these patients and included them in the final data analysis.
Bacterial meningitis was confirmed by CSF culture in 78 percent of patients and was the presumptive diagnosis in the remainder, based on the clinical presentation and at least one of the following individual CSF findings that is predictive of bacterial meningitis: low glucose level, low glucose ratio, elevated protein level, a white blood cell count greater than 2,000 per [mm.sup.3] (2 3 [10.sup.9] per L), or a neutrophil count of greater than 1,180 per [mm.sup.3] (1.18 3 [10.sup.9] per L). Streptococcus pneumoniae was the most common bacterial pathogen (35.8 percent), followed by Neisseria meningitidis (32.2 percent), negative CSF culture (21.6 percent), and other bacteria (9.6 percent).
The overall likelihood of an unfavorable outcome (death or neurologic sequelae) was significantly reduced in patients receiving dexamethasone compared with those receiving placebo (15 percent versus 25 percent, respectively). Subanalysis revealed that this risk reduction was caused exclusively by the steroid benefit in patients with pneumococcal meningitis. Among these patients, 26 percent in the dexamethasone group had an unfavorable outcome compared with 52 percent of those in the placebo group. The risk of death from pneumococcal infection was 34 percent in patients who received placebo compared with 14 percent in patients who received dexamethasone, a statistically significant difference. Dexamethasone use did not significantly reduce the risk of death in those with meningitis caused by other agents. While there was a trend toward fewer focal neurologic deficits in patients receiving dexamethasone (13 percent versus 20 percent with placebo), this trend was not statistically significant.
No adverse effects were significantly associated with the use of dexamethasone. Neither gastrointestinal bleeding nor hyperglycemia was significantly more common in patients receiving dexamethasone.
The authors concluded that early treatment with intravenous dexamethasone in adult patients with bacterial meningitis decreased the overall risk of an unfavorable outcome, especially in those with pneumococcal meningitis.
EDITOR'S NOTE: Widespread vaccination has almost completely eradicated Haemophilus influenzae meningitis in children; as a result, bacterial meningitis is now more common in adults than in children, and the most common pathogen is a Pneumococcus. Steroid use for adult meningitis is a simple, risk-free, and inexpensive intervention that substantially reduced mortality in the subgroup of patients with pneumococcal infection in this study. An accompanying editorial by Tunkel and Scheld emphasizes the necessity of timing the steroid dose correctly. To maximize its anti-inflammatory effect, dexamethasone should be given before, or no more than shortly after, the first antibiotic dose. These authors also note that in patients with penicillin-resistant Pneumococcus, vancomycin dosages should be increased, because the reduced inflammation caused by steroid use inhibits the blood-brain barrier penetrance of this antibiotic.--B.Z.
COPYRIGHT 2003 American Academy of Family Physicians
COPYRIGHT 2003 Gale Group