Monitoring nitrous oxide trace concentrations
Ambulatory Surgery
May 2005
The risks associated with chronic exposure to volatile anesthetic gases have not been established. Long-term occupational exposures to trace concentrations of volatile anesthetic gases, including nitrous oxide ([N.sub.2]O), however, are believed to have adverse health effects on exposed individuals. Such adverse effects include a potential for change in production of DNA precursors, spontaneous abortions, and impaired fertility.
Most countries have established guidelines for safe exposure limits based on a time-weighted average (TWA) during an eight-hour period. In the United States, the National Institute for Occupational Safety and Health (NIOSH) has set the limit at 25 parts per million (ppm) compared to a 100 ppm limit for [N.sub.2]O in most European countries. The purpose of this blinded study was to evaluate variations in [N.sub.2]O concentrations in an ambulatory center during routine anesthesia. (1)
Monitoring was conducted at an ambulatory center in Sweden. Trace [N.sub.2]O concentration monitors were placed on the top front of the anesthesia machines in two randomly selected ORs in the ambulatory center. The monitor used is a small, commercially available device with an infrared gas sensor. Sampling is done through gas diffusion, and the monitor can detect chronic and acute leaks by providing both instantaneous and cumulative TWA of [N.sub.2]O concentrations in ppm with an updating time of about 20 seconds.
All personnel were unaware of the monitoring, and anesthesia personnel followed departmental routines, including coadministration of propofol and fentanyl, two to four minutes of preoxygenation with a face mask, use of a laryngeal mask, and use of semiclosed anesthesia circuits. At the end of the procedure, they did not remove the laryngeal mask until the patient was awake enough to exhibit discomfort from the mask. The ORs had ordinary climate ventilation with approximately 25 air changes per hour, and all the anesthesia machines were connected to a standard scavenging system.
Findings. Thirty-seven ambulatory surgery sessions were monitored. Incidents with unnecessarily high peak and daylong averages of [N.sub.2]O concentrations were observed, including a session in which the exhaust system was not turned on and a session in which an ordinary mask was used instead of a laryngeal mask. Five (13.5%) of the TWAs for [N.sub.2]O concentrations were greater than the NIOSH threshold of 25 ppm (ie, 26 ppm, 40 ppm, 58 ppm, 79 ppm, 85 ppm). Peak levels reached 2,000 ppm. Eleven recordings showed peak levels above 100 ppm, three of which were above 500 ppm. The mean TWA for all 37 recordings was below 25 ppm (range 1 ppm to 85 ppm).
Clinical implications. This study revealed that the more conservative limit of 25 ppm generally is not difficult to achieve in the ambulatory setting, but sessions with unnecessarily high [N.sub.2]O concentrations can occur. Additionally, the study showed that the monitor detected technical errors and provided a way to maintain a high index of awareness for optimal gas hygiene. Perioperative managers should consider evaluating a monitoring device for use in their facilities.
Hand washing versus hand rubbing with alcohol-based products
Journal of Hospital Infection
May 2005
It is universally accepted that hand washing is the single most important procedure in preventing the transmission of infections in health care settings. Health care workers compliance with hand washing using soap and water as measured in observational studies, however, has been below 50% in both European and US hospitals. The introduction of a hand rubbing technique using alcohol-based, waterless, hand hygiene products has been shown to improve compliance in both intensive care and nonintensive care units, and alcohol-based, waterless products have been demonstrated to be more efficacious than soap in reducing the total microbiological count on the hands of health care workers during clinical situations. Little is known, however, about the respective efficacy of hand washing and hand rubbing with alcohol-based products on transient flora on health care workers hands. The objectives of this study were to evaluate the comparative microbiological efficacy of hand washing and hand rubbing in different categories of health care workers in different settings with particular emphasis on transient flora and to assess predisposing factors for hand contamination after patient care in everyday practice. (2)
During a six-month period (ie, November 2002 to April 2003) 50 health care workers, including nurses, physicians, physiotherapists, and radiology technicians, at a university hospital in Paris were randomly assigned, using a crossover design, to perform hand washing with unmedicated soap or hand rubbing with an alcohol-based, waterless, hand hygiene agent after a health care procedure. Hand washing with unmedicated soap was considered to be satisfactory if both hands were washed together for 30 [+ or -] 5 seconds, rinsed under running water, and then dried with a paper towel. The hand rubbing procedure was considered to be satisfactory if 2 mL to 3 mL of the product was applied to both hands, and all surfaces of the hands were rubbed together until dry.
Two hand hygiene procedures performed by each health care worker immediately after patient care were observed on the same day by one of two infection control technicians. Information recorded included
* the health care worker's gender and job title,
* the ward location,
* the type of health care procedure, and
* whether gloves were worn.
Before and after each hand hygiene procedure, imprints of the health care workers' palms and fingertips were taken and sent for colony counts and identification of transient flora. Common statistical techniques, including t tests, Wilcoxon nonparametric test, the McNemar test, and multivariate techniques were used to analyze the data.
Findings. The mean number of colony forming units (CFU) before hand hygiene procedures was 87 for palms (95% confidence interval [CI] 68-111) and 85 for fingertips (95% CI 67-108). Multivariate analysis revealed that working in a medical ward rather than an intensive care unit was significantly associated with increased hand contamination for palms and fingertips (P = .03 and P = .02, respectively). The use of gloves during a procedure was associated with significantly less hand contamination after patient care and before hand washing or hand rubbing (mean CFU 46 per five fingertips, 95% CI 31-67, P = .02)
Hand rubbing with the alcohol-based product was performed more rigorously than hand washing (P < .0001). The rate of transient flora identification was 18% in the hand washing group versus 12% in the hand rubbing group before hand hygiene procedures and 4% and 0%, respectively, after hand hygiene procedures.
Clinical implications. The results of this study indicate that hand rubbing with a waterless, alcohol-based hand hygiene product is more effective than hand washing with unmedicated soap for decontaminating the hands of health care workers after contact with patients and the patient's environment. Careful use of gloves also may reduce microbiological contamination of the hands. Perioperative managers should consider providing alcohol-based, waterless, hand hygiene products in all ORs.
Preventing emetic events after dental surgery
Journal of Clinical Anesthesia
May 2005
Dental surgery performed with general anesthesia is associated with a high incidence of postoperative nausea and vomiting (PONV), which can result in prolonged hospitalization and fluid and electrolyte imbalance. Consequently, the use of prophylactic antiemetics after dental surgery is justified. Most of the currently used antiemetics, such as antihistamines, butyrophenones, and dopamine receptor antagonists, however, occasionally have been reported to cause undesirable adverse effects, such as excessive sedation, hypotension, dry mouth, dysphoria, hallucinations, and extrapyramidal symptoms. Additionally, the use of serotonin receptor antagonists (eg, ondansetron) can be costly.
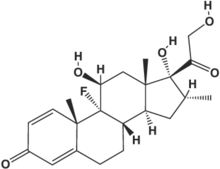
Recently, dexamethasone, which has been used effectively as an antiemetic in patients receiving chemotherapy for cancer, has been found to have a prophylactic effect on PONV in patients undergoing gynecological surgery, laparoscopic cholecystectomy, thyroidectomy, and pediatric tonsillectomy. The purpose of this prospective, randomized, double-blind, placebo-controlled study was to assess the antiemetic and analgesic effects of dexamethasone in the prevention of PONV after dental surgery. (3)
One hundred twenty patients (ie, 45 men, 75 women) ages 17 to 48 years undergoing dental surgery under general anesthesia at a hospital in Tokyo were randomly assigned to one of four groups (n = 30 patients per group). Group I received a placebo, group II received 4 mg dexamethasone, group III received 8 mg dexamethasone, and group IV received 16 mg dexamethasone intravenously at the end of surgery. The placebo and the different doses of dexamethasone were prepared by personnel who were not involved in the study and dispensed in identical syringes.
All patients had an American Society of Anesthesiologists classification of I or II. The dental procedure was completed on all the patients using the same general anesthetic technique. Postoperatively, 50 mg diclofenac was administered rectally to patients who complained of intolerable pain. All episodes of emetic symptoms during the first 24 hours after anesthesia were recorded. Nausea was defined as the subjectively unpleasant sensation associated with awareness of the urge to vomit. Severity of nausea was graded on a 10-point scale in which zero = no nausea and 10 = severe nausea. Retching was defined as the labored, spasmodic, rhythmic contraction of the respiratory muscles without expulsion of gastric contents, and vomiting was defined as the forceful expulsion of gastric contents from the mouth. Common statistical techniques including chi square analysis, t tests, Mann-Whitney U test, and analysis of variance were used to analyze differences between the groups.
Findings. The rate of patients who were emesis-free was significantly higher in the groups that received 8 mg and 16 mg dexamethasone compared to the group that received the placebo (P < .05). Ninety percent of the patients in the 16 mg dexamethasone group were emesis-free during the first 24 hours after anesthesia compared to 83% in the 8 mg dexamethasone group, 63% in the 4 mg dexamethasone group, and 60% in the placebo group. Additionally, the severity of nausea was significantly less in patients receiving 8 mg and 16 mg dexamethasone than in those receiving 4 mg dexamethasone or placebo (P < .05). The need for diclofenac for intolerable pain was significantly lower in patients in the 8 mg and 16 mg dexamethasone groups compared to the placebo and 4 mg dexamethasone groups (P < .05). No clinically important adverse events caused by the study medications were observed in any of the groups.
Clinical implications. The results of this study suggest that use of 8 mg prophylactic dexamethasone is a safe and cost-effective strategy for preventing PONV and managing postoperative pain after dental surgery. Perioperative managers in the United States should consider conducting a cost analysis between the use of 8 mg dexamethasone and serotonin receptor antagonists (eg, ondansetron) as prophylaxis against PONV after dental surgery.
Using liposomal lidocaine to reduce procedural pain in children
Canadian Medical Association Journal
June 2005
Painful medical procedures, including IV cannulation, routinely are performed on children for diagnostic and therapeutic reasons. Pain resulting from these procedures has both short-term and long-term consequences. Short-term consequences may include lack of cooperation by the child, unsuccessful procedure attempts, repeated attempts, additional pain, and increased procedure time. Long-term consequences may include the development of a conditioned anxiety response and an increased pain perception that can persist into adulthood and result in avoidance of medical care.
Local anesthetics can reduce the pain of cannulation; however, most preparations are not feasible for routine use. Lidocaine-prilocaine 5% cream, the gold standard for skin anesthesia, requires a 60-minute application time and may cause vasoconstriction, and a subcutaneous injection of lidocaine is associated with an extra painful puncture. Liposomal lidocaine 4% cream recently became available in Canada as an analgesic for reducing pain from venipuncture and IV cannulation. Its advantages include having a short onset action (ie, 30 minutes); being needle-free; having minimal vasoactive properties; and not being associated with methemoglobinemia, a systemic side effect of lidocaine-prilocaine. The aim of this randomized, prospective study was to determine the success rate of cannulation, analgesic effectiveness, and safety when liposomal lidocaine cream is used before IV cannulation in children. (4)
Patients aged one month to 17 years at a children's hospital emergency room in Canada who required a peripheral IV cannula between June 2003 and February 2004 (N = 142) were randomly assigned to one of two groups. Group I (n = 69) received liposomal lidocaine cream and group II (n = 73) received a placebo cream. The creams and tubes were visually identical. At two sites where cannulation was to be attempted, each patient received 1g of either liposomal lidocaine cream or the placebo. The sites were covered with an occlusive transparent dressing for 30 minutes. After 25 minutes, the child's baseline pain score was determined using a faces pain scale. The cream was removed 30 minutes after application, and the skin reaction was recorded.
Before inserting the cannula, the nurse rated the expected level of difficulty for cannulation on a five-point scale that ranged from extremely easy to extremely difficult. Successful cannulation was recorded when the skin was breached only once, and the IV line remained in place for at least five minutes. A failure was recorded if a second puncture was required or if a site other than one of the two chosen sites was cannulated. The number of attempts and the duration of the procedure were recorded. Pain scores were obtained again after the first attempt, and pain during cannulation was calculated as the pain score after the first cannulation attempt minus the baseline score. Common statistical procedures including chi-square analysis, t test, and logistic and linear regression techniques were used to compare the differences between the groups.
Findings. There were no significant differences in baseline characteristics between the two groups. The incidence of transient skin reactions was the same in both groups. The cannulation success rate was significantly higher (74% versus 55%, P = .03) and the total procedure time was shorter (6.7 minutes versus 8.5 minutes, P = .04) in the group that received liposomal lidocaine than in the group that received the placebo. Use of liposomal lidocaine was associated with a lower likelihood of cannulation failure compared to placebo (odds ratio 0.38, 95% CI 0.18-0.8). Children five years old and older who received liposomal lidocaine reported less pain than those who received the placebo (P = .01). Parents and research assistants also reported less pain among children who received liposoreal lidocaine (P > .001).
Clinical implications. In this study, liposomal lidocaine was associated with a 35% higher cannulation success rate, a 21% shorter overall procedure time, and less pain. Given these results, the relative ease of administration, and findings of only minor dermal changes, perioperative nurses should consider evaluating the use of liposomal lidocaine cream before IV cannulation in children when it becomes available in the United States.
This information is intended for general use only. The clinical implications are specific to the abstracted article only. Individuals intending to put these findings into practice are strongly encouraged to review the original article to determine its applicability to their setting.
NOTES
(1.) R E Anderson, G Barr, J G Jakobsson, "Operating room nitrous oxide trace concentrations: A clinical study in ambulatory surgery," Ambulatory Surgery 12 (May 2005) 23-26.
(2.) G Kac et al, "Microbiological evaluation of two hand hygiene procedures achieved by healthcare workers during routine patient care: A randomized study," The Journal of Hospital Infection 60 (May 2005) 32-39.
(3.) M Numazaki, Y Fujii, "Reduction of postoperative emetic episodes and analgesic requirements with dexamethasone in patients scheduled for dental surgery," Journal of Clinical Anesthesia 17 (May 2005) 182-186.
(4.) A Taddio et al, "Liposomal lidocaine to improve procedural success rates and reduce procedural pain among children: A randomized control trial," Canadian Medical Association Journal 172 (June 21, 2005) 1691-1695.
GEORGE ALLEN RN, PHD, CNOR, CIC DIRECTOR OF INFECTION CONTROL DOWNSTATE MEDICAL CENTER BROOKLYN, NY
COPYRIGHT 2005 Association of Operating Room Nurses, Inc.
COPYRIGHT 2005 Gale Group