Results of a Controlled Study
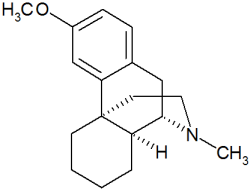
Background: Dextromethorphan (DM), the d-isomer of the codeine analog levorphanol, is an active ingredient present in a variety of cough and cold remedies. Recently, data generated from a study in chick embryos were extrapolated to suggest that pregnant women should not use this drug because of the risk of birth defects. We conducted a controlled study of pregnant women who used DM, to examine the possible teratogenic risk in humans.
Materials and methods: We followed up women who used DM and had been counseled by the Motherisk Program during their pregnancy. A control group of women was matched for age, smoking, alcohol use, and disease state (upper respiratory tract infection, not treated with DM).
Results: We were able to ascertain pregnancy outcome in 184 women. There were 172 live births, 10 spontaneous abortions, 1 therapeutic abortion, and 1 stillbirth. One hundred twenty-eight of the women used the drug during the first trimester of pregnancy. There were three major malformations (2.3%) among the babies of women who used DM in the first trimester, seven minor malformations, and the mean ([+ or -] SD) birth weight was 3,381 [+ or -] 670 g. In the control group, there were 174 live births, 8 spontaneous abortions, and 2 therapeutic abortions. There were five major malformations, one of which was a chromosomal abnormality (2.8%), eight minor malformations, and the mean birth weight was 3,446 [+ or -] 571 g.
Conclusion: This study fails to show that DM use during pregnancy increases the rates of major malformations above the expected baseline rate of 1% to 3%. (CHEST 2001; 119:466-469)
Key words: birth defects; dextromethorphan; pregnancy
Abbreviation: DM = dextromethorphan
Dextromethorphan (DM) is the d-isomer of the codeine analog levorphanol, an antitussive that is an active ingredient in a variety of over-the-counter cough and cold medications. It is a synthetic, nonnarcotic, centrally acting cough suppressant that is available either alone (eg, as lozenges or oral solution) or in combination with a large number of other compounds used for upper respiratory tract infections.[1]
No information is available on the placental transfer of DM. Its molecular weight (about 271), however, is low enough that transfer to the fetus probably occurs. Animal reproductive studies have not been conducted with DM. In an in ovo study[2] examining the effects of DM on chick embryos, the authors hypothesized that N-methyl-D-aspartate receptor antagonists, such as ethanol and DM, induce neural crest (craniofacial and cardiac septal defects) and neural tube defects. They also cited published evidence that during early development, the receptors blocked by DM in the chick embryos are analogous to receptors in other species and therefore concluded that the drug would also block these receptors, resulting in similar malformations in humans.[2]
In humans, the only published studies[3] to date are from the Collaborative Perinatal Project, which monitored 50,282 mother-child pairs, 300 of whom used DM during the first trimester. There was no increase above the baseline rate of 1% to 3% for major malformations and no increase in the relative risk for any specific malformation.[3] A surveillance study,[4] which linked automated pharmacy records and the outcome of pregnancies in 59 women who were assumed to have used DM sometime in the first trimester of their pregnancy, documented one malformation in this group. These data have formed the widely accepted view that DM is probably safe to use during pregnancy, and this information has been included in several reviews.[5-9]
A study[2] in chick embryos concluded that women should not use DM during pregnancy. These data, although very limited in terms of their applicability, to humans, received wide publicity, causing high levels of anxiety among pregnant women and their health-care professionals.[10]
The Motherisk Program at The Hospital for Sick Children is a counseling service for pregnant and lactating women and their health professionals. Following the publication of the results of the chick embryo study in the newspapers, we received many calls from women who were pregnant, had used DM, read the article, and became quite concerned. Because of the paucity of studies specifically examining DM, we carried out the present study to provide additional evidence-based information on pregnancy outcome following gestational exposure to this drug.
MATERIALS AND METHODS
Between 1995 and 1998, [is greater than] 100,000 women and/or their health professionals were counseled by the Motherisk Program. For the purpose of this study, we attempted to follow up all the women who had been counseled on the use of DM and to ascertain the outcomes of their pregnancies. During the initial interview, while they were pregnant, history of drug exposure and pregnancy was taken, as well as other medical details of interest, with the aid of a structured questionnaire. Exposure history included medical indication for drug use, dosage, frequency of administration, and timing of exposure, as well as data such as maternal demographics and obstetric history. At follow-up, the women were questioned regarding the course of their pregnancy, the health of their child, and the specific details of their exposure to DM and any other drugs or other possible exposures during their pregnancy. Outcomes were confirmed by sending a letter to the child's primary-care physician who corroborated the mother's information.
The primary outcome of interest was the rate of major malformations. Major malformations were defined by the presence of any anomaly that has an adverse effect on either the function or the social acceptability of the individual.[11] Secondary outcomes included spontaneous or therapeutic abortions, live birth or stillbirth, minor anomalies, and birth weight. Exposure was defined as occurring during organogenesis if the drug was consumed between the 4th week and 14th week of gestation.
Each woman exposed to DM was matched to a woman who also had an upper respiratory infection and had inquired about the safety of either DM or echinacea, but subsequently did not use either of them, or women who had been exposed to clarithromycin, an antibiotic considered safe for use during pregnancy.[12] The women were also matched by maternal age ([+ or -] 2 years) and cigarette and alcohol consumption during their pregnancy. To assess the possibility of a selection bias, women lost to follow-up were compared with those successfully followed up for maternal age, gestational age, parity, previous spontaneous and therapeutic abortions, and cigarette and alcohol consumption, and were found to be similar. Outcomes of interest were compared between the study and control groups with the Mann-Whitney or [chi square] test whenever appropriate. The protocol was approved by the Research Ethics Board of our hospital.
RESULTS
We were able to ascertain the outcomes of 184 pregnancies exposed to DM, of which 128 exposures occurred in the first trimester of pregnancy. The characteristics of the women lost to follow-up were not different from the women successfully enrolled in the study. Sixty percent of the women used DM in combination with other cough and cold products. Fifty percent of the women reported using other medications during their pregnancy, all of which are known to be nonteratogenic. Many of the women did not remember the exact amount taken, so we classified the range of doses as low, medium, and high (Table 1).
(*) tsp = teaspoon.
In the study group, there were a total of 172 live births, 10 spontaneous abortions (5.4%), 1 therapeutic abortion, and 1 stillbirth. There were six babies born with major malformations; however, one was a chromosomal abnormality and two were born to women who used DM during the second and third trimester, so the actual number of babies with major malformations of women who used DM in the first trimester was three (2.3%). There were 10 minor malformations, of which seven women were exposed to DM in the first trimester and the mean ([+ or -] SD) birth weight was 3,381 [+ or -] 670 g.
In the control group, there were 174 live births, 8 spontaneous abortions (4.3%), 2 therapeutic abortions, and no stillbirths. There were five major malformations, one of which was also a chromosomal abnormality (2.2%), eight minor malformations, and the mean birth weight was 3,446 [+ or -] 571 g (Table 2).
(*) Data are presented as No. unless otherwise indicated.
There were no significant differences in the maternal characteristics or outcome measures between the groups.
DISCUSSION
Although DM has been on the market for many years, this is the first controlled study to specifically examine this particular cough medicine for its safety during pregnancy. The rates of malformations in the DM and the control groups were comparable, with no specific pattern of defects emerging in either group. Of particular interest, there were no cases of neural tube defects in the study group, as was suggested by the in ovo study.[2]
The inappropriate extrapolation from the chick embryo model to humans and the subsequent publicity in the lay press caused many women and their health professionals undue alarm. In fact, one woman in our study group reported that the Toronto Star article with the headline "Pregnant women urged to shun cough remedies" was posted in her doctor's office.[10]
It is crucial to examine the relevance of the teratogenicity in a chick embryo in humans. Animal studies can but do not always predict whether a drug will be teratogenic in humans; the main role of animal studies is to understand the mechanisms of teratogenicity. When thalidomide was first tested on rats and mice, it did not produce birth defects.[13] Conversely, some drugs have been found to be teratogenic in animals, but were not in clinically relevant doses in humans.[5,12] Today, when new drugs are screened for teratogenicity, three different animal models are required for testing.[5] Consequently, it can happen quite frequently that when certain drugs are tested on different animal species, birth defects will occur, such as in the DM study.[2]
The situation is much more complex when in ovo or other in vitro methods are used. As delineated by Polifka and Shepard,[14] Brent,[15] and Holmes,[16] in vitro studies cannot be used to identify a human teratogen, due to an absence of normal absorption, distribution and metabolism, the excessive dose used, the very short duration of the in vivo experiment, and the lack of epidemiologic evidence for human teratogenicity.
There are several limitations to this study. It is a known fact that DM is metabolized by cytochrome P450, with 1 in 10 of the population deficient in the enzyme, resulting in the ingestion of DM in some women leading to higher plasma levels. However, we do not really believe this is important, because dosage does not appear to be crucial.
Another limitation is we cannot define the exact amount of DM used; however, we do know that the dose of DM in over-the-counter preparations is either 15 mg or 30 mg per dose.
Finally, the biggest limitation is the sample size, as is always the case in these types of studies in pregnant women. For obvious reasons, women are not going to volunteer to participate in a study if they are asked to take a drug to investigate if it causes birth defects. These are women who were either unaware they were pregnant, or were suffering from such a bad cough that they took the drug regardless. This sample size has an 80% power to detect a 3.5-fold increase in the rate of malformations, with an ct of 0.05 and a 95% confidence interval.
In summary, our study of 184 women who were exposed to DM during their pregnancy (128 exposures in the first trimester) did not reveal an increase in the rates of major malformations above the baseline rate of 1% to 3%.
These results suggest that the use of DM in fregnancy does not pose a risk to the fetus; however, because of the size of this study, we are unable to rule out an increased risk for rare malformations.
ACKNOWLEDGMENT: We thank Linda Goldberg, Iona Lalkin, Diana Zimmer, Melissa Kerns, Bailey Tabak, Jillian Murphy, Sherri O'Neill, and Tillie Chiu for assistance in data collection.
REFERENCES
[1] Compendium of nonprescription products. 5th ed. Ottawa, Ontario, Canada: Canadian Pharmacists Association, 1998; 167
[2] Andalaro V, Monaghan D, Rosenquist T. Dextromethorphan and other N-methyl-d-aspartate receptor antagonists are teratogenic in the avian embryo model. Pediatr Res 1998; 43:1-7
[3] Heinonen OP, Slone D, Shapiro S. Birth defects and drugs in pregnancy. Littleton, MA: Publishing Sciences Group, 1997
[4] Aselton P, Jick H, Milunsky A, et al. First trimester drug use and congenital disorders. Obstet Gynecol 1985; 65:451-455
[5] Koren G, Pastusak A, Ito S. Drugs in pregnancy. N Engl J Med 1998; 338:1128-1137
[6] Berglund F, Flodh H, Lundborg P. Drug use during pregnancy and breastfeeding: a classification system for drug information. Acta Obstet Gynecol Scand Suppl 1984; 126: 1-55
[7] Management of asthma during pregnancy: report of the working group on asthma and pregnancy; executive summary. J Allergy Clin Immunol 1994; 93:139-162
[8] Rayburn WF. OTC drugs and pregnancy. Perinatol Neonatol 1984; 8:21-27
[9] Onnis A, Grella P. The biochemical effects of drugs in pregnancy (vol. 2). West Sussex, England: Ellis Horwood Limited, 1984; 62-63
[10] Pregnant women urged to shun cough remedies. The Toronto Star. January 17, 1998:A10
[11] Marden PM, Smith DW, McDonald MJ. Congenital anomalies in newborn infants, including minor variations. J Pediatr 1964; 64:357-371
[12] Einarson A, Phillips E, Mawji F. A prospective multicentre study of clarithromycin in pregnancy. Am J Perinatol 1998; 15:523-525
[13] Newman CGH. Clinical aspects of thalidomide embryopathy: a continuing preoccupation. Teratology 1985; 32: 133-144
[14] Polifka JE. Shepard TH. The teratogenicity of N-methyl-D-aspartate (NMDA) receptor antagonists [letter]. Pediatr Res 1998; 44:415
[15] Brent RL. The teratogenicity of N-methyl-D-aspartate (NMDA) receptor antagonists [letter]. Pediatr Res 1998; 44:415-417
[16] Holmes B. Exposures in pregnancy that are harmful to the fetus i.e. human teratogens. Pediatr Res 1999; 45:286-287
(*) From the Motherisk Program, Division of Clinical Pharmacology The Hospital for Sick Children, University Of Toronto, Ontario, Canada.
Supported by a collaboration of the following companies: W. K. Buckley Limited; McNeil Consumer Products Company; Novartis Consumer Health Canada, Inc.; Warner Lambert Consumer Healthcare; and Whitehall-Robins, Inc.
Manuscript received December 8, 1999; revision accepted June 15, 2000.
Correspondence to: Adrienne Einarson, The Motherisk Program, Division of Clinical Pharmacology, The Hospital for Sick Children, 555 University Ave, Toronto, M5G 1X8, Ontario, Canada; e-mail: einarson@sickkids.on.ca
COPYRIGHT 2001 American College of Chest Physicians
COPYRIGHT 2001 Gale Group