Invasive haemodynamic monitoring should be considered when hypotension fails to respond to empirical treatments
We present a potentially fatal case of diltiazem overdose caused by inappropriate self treatment. We highlight the clinical features of diltiazem overdose, relevant haemodynamic findings, and treatment options.
Case report
A 54 year old white man presented with nausea, dizziness, and collapse after an episode of severe angina 10 hours previously. He had been free of pain for 8 hours but was bradycardic and hypotensive and had severe pulmonary oedema. He had no features suggestive of ongoing infection. Maintenance treatment for his angina was bisoprolol 5 mg once daily, slow release diltiazem 180 mg twice daily, isosorbide mononitrate 40 mg three times a day, nicorandil 10 mg twice daily, frusemide 40 mg once daily, simvastatin 20 mg once daily, fluoxetine 40 mg once daily, and aspirin 75 mg once daily. He was known to have severe triple vessel coronary artery disease and poor left ventricular function. Electrocardiography indicated a sinus bradycardia with new first degree heart block (PR interval 300 milliseconds), pre-existing left bundle branch block, and no new changes in the ST segments or T waves suggestive of an acute myocardial infarction.[1] Despite treatment for cardiogenic shock with intravenous dopamine, dobutamine, and diuretics, he developed acidosis, anuria, type 1 respiratory failure, and persistent hypotension. As there was no electrocardiographic or enzymatic evidence of myocardial infarction, he was transferred to Papworth Hospital for consideration of coronary artery bypass grafting as treatment for presumed ischaemic left ventricular dysfunction. On arrival, a carefully elicited history showed that his angina had resolved eight hours before his initial admission after self treatment with six 180 mg slow release diltiazem tablets at the onset of his symptoms. In the past he had successfully treated himself with four 40 mg isosorbide mononitrate tablets in a similar situation. Invasive haemodynamic monitoring with a Swan-Ganz catheter was instituted, and an intra-aortic balloon pump was inserted percutaneously by way of the right femoral artery. The table shows the results of measuring several haemodynamic variables. The history, clinical findings (inappropriate sinus bradycardia, newly developed first degree heart block), and haemodynamic data (profound vasodilation, with a normal cardiac index despite underlying poor left ventricular function and in the absence of sepsis or liver disease) suggested a diltiazem overdose. He was started on noradrenaline, titrated against the systemic vascular resistance obtained from haemodynamic monitoring. His renal, respiratory, and cardiac problems recovered to baseline levels over the next 48 hours, with normalisation of the PR interval. He was successfully weaned from all inotropic support, and the intra-aortic balloon pump was removed. His liver function test results remained normal throughout, and blood cultures gave negative results. He was transferred back to his referring hospital. Diltiazem overdose was confirmed seven weeks later. The serum concentration of diltiazem 23 hours after ingestion was 1230 ng/ml (therapeutic range 40-160 ng/ml).
Discussion
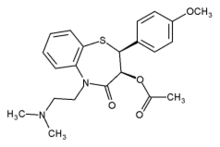
Diltiazem is a calcium channel antagonist, which causes vasodilation and has negative chronotropic, dromotropic, and inotropic properties.[2] Reports of diltiazem overdose are rare but well documented.[2-9] The diagnosis of diltiazem overdose is based on clinical features affecting the central nervous system (for example, confusion, lethargy, coma, respiratory arrest), gastrointestinal system (nausea, vomiting), cardiovascular system (hypotension, bradycardias, and a variety of differing degrees of heart block), and respiratory system (non-cardiogenic pulmonary oedema).[2 3] Metabolic effects include hyperglycaemia and lactic acidosis.[2 3] The haemodynamic features in diltiazem overdose are a low systemic vascular resistance in the presence of good cardiac output.[4 5] Serum diltiazem concentrations will confirm the diagnosis, but the assay is neither readily nor rapidly available.[4] The treatment for diltiazem overdose is essentially supportive, although early haemoperfusion with intravenous calcium and charcoal may have some beneficial effect.[2-9]
Many patients associate a single drug with a single therapeutic action. They are often unaware of any of its other potential actions. Our patient perceived his drug to be predominantly for the relief of angina. This perception was reinforced after his initial self treatment with a large quantity of isosorbide mononitrate. He was indirectly aware of the coronary vasodilation that nitrates can cause but was unaware of the drug's effects on systemic vasodilation. It is likely that nitrate tolerance was the only factor that prevented his admission with hypotension on that occasion. Subsequently, the significance of the amount of diltiazem was not appreciated by the patient nor shown in a cursory drug history. Inevitably the patient's failure to respond to treatment was ascribed to insufficient treatment rather than inappropriate treatment by the admitting team.
Two lessons can be learnt from this case. Firstly, an adequate drug history should include not just the list of drugs prescribed for a patient but also the patient's compliance with them--that is, whether insufficient or excessive quantities of prescribed drugs are being taken. A more detailed drug history might have led to the earlier institution of appropriate treatment and avoided the development of potentially fatal multiple organ failure. Secondly, the earlier use of haemodynamic monitoring would have increased the suspicion of a diagnosis other than ischaemic left ventricular dysfunction. Haemodynamic monitoring by Swan-Ganz catheterisation is a widely available tool.[10] It is especially useful in hypotensive patients when the cause of haemodynamic compromise is uncertain, in certain cases of pulmonary oedema associated with hypotension, and, as in this patient, when the response to treatment is poor.[10] Confirmation of the diagnosis by measurement of haemodynamic variables prevented inappropriate, extremely high risk surgery being performed.
We thank the staff at Papworth Hospital and Dr M Satchithananda for their help in preparing this document.
Funding: DKS is supported by a fellowship grant from the Garfield Weston Trust.
Contributors: All the authors were involved in the routine day to day care of the patient, conceived the idea for the article, and reviewed and rewrote the manuscript. DKS was responsible for collating the references and writing the article; he will act as guarantor for the paper.
Competing interests: None declared.
[1] Sgarbossa EB, Pinski SL, Barbagelata A, Underwood DA, Gates KB, Topol EJ, et al. The GUSTO-1 investigators. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. N Engl J Med 1996;334:481-7.
[2] Pearigen DP, Benowitz NL. Poisoning due to calcium antagonists: experience with verapmnil, diltiazem and nifedipine. Drug Safety 1991;6:408-30.
[3] Lip GYH, Ferner RE. Poisoning with anti-hypertensive drugs: calcium antagonists. J Hum Hypertens 1995;9:155-61.
[4] Williamson MK, Dunham GD. Plasma concentrations of diltiazem and desacetyldiltiazem in an overdose situation. Ann Pharmacother 1996;30: 698-11.
[5] Proano L, Chiang WK, Wang RY. Calcium channel blocker overdose. Am J Emerg Med 1995; 13:444-50.
[6] Kenny J. Treating overdose with calcium channel blockers. BMJ 1994;30:992-3.
[7] Erickson FC, Ling LJ, Grande GA, Anderson DL. Diltiazem overdose: case report and review. J Emerg Med 1991;9:357456.
[8] Roberts D, Honcharik N, Sitar DS, Tenenbein M. Diltiazem overdose: pharmacokinetics of diltiazem and its metabolizes and effect of multiple dose charcoal therapy. Clin Toxicol 1991;29:45-52.
[9] Melanson P, Shih RD, DeRoos F. Intra-aortic balloon counterpulsation in calcium channel blocker overdose. Vet Hum Toxicol 1993;35:345.
[10] Bayliss J, Norell M, Ryan A, Thurston M, Sutton GC. Bedside haemodynamic monitoring: experience in a general hospital. BMJ 1983;287:187-90.
(13 December 1999)
Papworth Hospital, Papworth Everard, Cambridge CB3 8RE
D K Satchithananda specialist registrar
D L Stone consultant cardiologist
A Chauhan senior registrar
A J Ritchie consultant cardiothoracic surgeon
Correspondence to: D K Satchithananda dargoi.satchi@ excite.com.uk
BMJ 2000;321:160-1
COPYRIGHT 2000 British Medical Association
COPYRIGHT 2000 Gale Group