ADVISORY PRACTICE OPINIONS
Role of RN in Psychiatric-Mental Health Nursing, Psychotherapy, and Counseling
KBN has received a letter expressing concern that registered nurses (RNs) who provide psychotherapy may not be educationally prepared to perform this act a stated in Advisory Opinion Statement (AOS) #85-13, Psychiatric-Mental Health Nursing By RNs. An excerpt of the opinion follows:
The performance of psychotherapy (individual, group and family therapies) is within the scope of practice of the RN who is educationally prepared at the masters degree level in psychiatric-mental health nursing. It is also within the scope of practice of this RN to assume independent responsibility for a primary therapist role.
It is within the scope of RN practice for the RN who is not prepared at the master's degree level to participate and assist in psychotherapy with a qualified primary therapist. The performance of other nursing care functions, including but not limited to, counseling (individual, group and family counseling) and management of the therapeutic milieu, are within the scope of RN practice.
RNs who perform psychiatric-mental health nursing functions should be educationally prepared and clinically competent in psychiatric-mental health nursing, and should have documented evidence of completion of education that provides clinical practice and demonstrated competency in the performance of psychiatric-mental health nursing functions.
RNs who perform psychiatric-mental health nursing functions should perform these functions according to accepted standards of practice.
The full text of the advisory opinion statement, which contains definitions of psychotherapy and counseling, is on the KBN website.
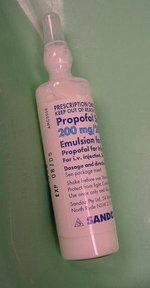
Role of RN in the Administration of Diprivan/ Propofol for Procedural Sedation
The Board reaffirmed Advisory Opinion Statement #95-32, Intravenous Administration of Medications for Conscious/Moderate Sedation by Nurses. A copy may be obtained from the KBN website.
In addition, following review of the statutes governing nursing practice, and the product information on Diprivan Injection, it was the advisory opinion of the Board that Diprivan may be administered by a qualified registered nurse as described in the "warnings" section of the product information, which states:
* For sedation of intubated, mechanically ventilated adult patients in the intensive care unit Diprivan Injection should be administered only by persons skilled in the management of critically ill patients and trained in cardiovascular resuscitation and airway management.
* For general anesthesia or monitored anesthesia care Diprivan Injection should be administered only by persons trained in the administration of general anesthesia and not involved in the conduct of the surgical/diagnostic procedure. Patients should be continuously monitored for maintenance of a patient airway, artificial ventilation, and oxygen enrichment and circulatory resuscitation must be immediately available.
A registered nurse qualified by education, experience and current clinical competency may administer Diprivan Injection, as prescribed, for sedation of intubated, mechanically ventilated patients in critical care settings (including aero medical advanced emergency service units). An ARNP, designated nurse anesthetist, may administer Diprivan Injection for general anesthesia or monitored anesthesia care.
The administration of Diprivan Injection for procedural sedation is not within the scope of RN practice, but is within the scope of the ARNP designated nurse anesthetist. If Diprivan is administered for procedural sedation purposes by a physician, then the qualified RN may monitor and assess the patient, and report findings to the on-site physician who administered the drug. The physician should be available throughout the procedure and during the post procedural monitoring period. The patient should be monitored according to accepted standards of practice.
The Board is continuing to study the role of ARNPs (non-nurse anesthetists) in the administration of Diprivan for sedation purposes.
Role of RN in the Administration of Etomidate During Rapid Sequence Intubation (RSI) in the Hospital Settings
It was the advisory opinion of the Board that the administration of Etomidate, as prescribed, for RSI is within the scope of RN practice when:
1. The administration of the medication is performed under the direct supervision/ presence of the physician, or advanced registered nurse practitioner, designated nurse anesthetist, who is performing the intubation.
2. The nurse is educationally prepared and currently clinically competent to perform the act in a safe, competent manner. Documentation of the nurse's educational preparation and demonstrated clinical competence is maintained.
3. The procedure is performed, and the patient is monitored, according to accepted standards of practice for RSI.
The Board has previously issued an opinion on the role of the RN in the administration of Etomidate during RSI in aero medical settings, which may be obtained upon request.
Role of RN in the Administration of Ketamine Hvdrochloride for Procedural Sedation and Analgesia (PSA)
The Board accepted a definition of "procedural sedation and analgesia" (PSA) as follows: A technique of administering sedatives or dissociative agents (such as Ketamine Hydrochloride) with or without analgesics to induce a state that allows the patient to tolerate unpleasant procedures while maintaining cardiorespiratory function. Procedural sedation and analgesia is intended to result in a depressed level of consciousness but one that allows the patient to maintain airway control independently and continuously. Specifically, the drugs, doses, and techniques used are not likely to produce a loss of protective airway reflexes." (Krause, Baruch, MD, "Management of Acute Pain and Anxiety In Children Undergoing Procedures In the Emergency Department," Pediatric Emergency Care. Vol. 17, No. 2, p 117.)
It was the advisory opinion of the Board that both the administration of Ketamine Hydrochloride, as prescribed, for PSA and the monitoring of patients receiving Ketamine Hydrochloride for PSA were within the scope of RN practice when:
1. A physician, or qualified ARNP, is readily available throughout the procedure and during the post procedural monitoring period.
2. The nurse is educationally prepared and currently clinically competent to perform the act in a safe, effective manner. Documentation of the nurse's educational preparation and demonstrated clinical competence is maintained.
3. The monitoring of the patient is according to accepted standards of PSA.
Should you have questions or need additional information about any of the advisory practice opinions, contact Bernadette Sutherland, Nursing Practice Consultant, at 800-305-2042, Ext 231, or 502-329-7007. You may also visit the KBN website at http://kbn.ky.gov.
Copyright Kentucky Nurses Association Apr-Jun 2004
Provided by ProQuest Information and Learning Company. All rights Reserved