ABSTRACT
For individuals with spinal cord injuries (SCI) there are numerous unique medical conditions that exist involving cardiovascular/autonomic systems, pain, depression, spasticity, heterotopic ossification, and bowel/bladder dysfunction. In this article the physiological basis of such conditions and focus on the pharmacological agents used in the management and treatment of these conditions will be reviewed. The basic mechanisms of action and major adverse effects will be discussed.
INTRODUCTION
The incidence of spinal cord injury (SCI) in the United States is approximately 11,000 injuries per year with a prevalence between 180,000-230,000 persons.1 As a consequence of SCI, many functions of the body are disrupted and require intervention to regulate and maintain physiologic function. Clinicians practicing with this population require knowledge of the pharmacological agents used in the treatment of complications due to SCI. In this article an overview of pharmacological agents used in the treatment of pain, depression, spasticity, bowel and bladder abnormalities, and cardiovascular and autonomic dysfunction associated with SCI is presented. The paper is organized by system dysfunction with specific disorders and their management.
CARDIOVASCULAR AND AUTONOMIC DYSFUNCTION
Immediately following SCI, patients may develop neurogenic spinal shock. Spinal shock is a transient depression of cord function below the level of injury characterized by hypotension, bradycardia, and hypothermia. Following its resolution, a variety of cardiovascular and autonomic dysfunctions may ensue.
Autonomic Dysreflexia
Autonomic dysreflexia (AD) is an unopposed sympathetic discharge causing an increase in blood pressure.2 Autonomic dysreflexia is usually seen in patients with injuries at T6 or above with an incidence thought to be from 48% to 85%.3 It is caused by a strong or noxious stimulus (distended bladder, fecal impaction, or pressure ulcer) below the level of the injury. Higher central nervous system centers are unable to modulate the sympathetic response because of the injury to the spinal cord. Patients will present with hypertension, pounding headache, flushing above the level of the lesion, and anxiety. Bradycardia is often seen as a compensatory response since the carotid baroreceptors, sensing the acute hypertension, send inhibitory impulses to the sympathetic system. Occasionally, patients will have silent AD and be completely asymptomatic.4
In those patients with acute AD, prompt action is required to prevent potential end organ damage (cerebral hemorrhage, seizures, myocardial infarction, etc.). The basis of treatment is to remove the underlying noxious stimulus. To manage the situation, first sit the patient upright and attempt to identify the cause. Loosen all clothing and equipment and begin to inspect for urinary distension produced by a blocked catheter. Urinary distension is the most common cause of AD. If no catheter is present, the patient must be catheterized. If symptoms do not resolve, further inspection for a cause must be conducted. An undetected fracture, fecal impaction, pressure ulcers, and tight clothing are other causes of AD. Once the noxious stimulus is found and treated, the symptoms tend to resolve quickly. However, if there is no change in symptoms, pharmacological intervention is necessary to reduce blood pressure.5 Nitroglycerin paste is a rapidly acting vasodilator that can be easily applied and then removed when the symptoms normalize. Nifedipine is another commonly used pharmacological agent that reduces vascular tone by blocking calcium channels in smooth vascular muscle. It should be mentioned that with the administration of antihypertensive medications a rapid swing of blood pressure may occur in the other direction resulting in hypotension.
Orthostatic Hypotension
Orthostatic hypotension is a decrease in blood pressure as a person transitions from a supine to a sitting or standing position. This occurs due to the lack of muscle tone and pumping action that assists venous return to the heart, as well as abnormal autonomic function. Symptoms include dizziness, lightheadedness, and syncope. While it is more likely to occur in those with injuries above T6 and complete injuries, the true incidence is unknown.2 This condition is treated initially with compensatory strategies (ace wraps and abdominal binders) and tends to resolve as muscle tone improves. If orthostatic hypotension continues to be problematic, pharmacological options are available.
Midodrine hydrochloride is a vasoconstrictor that acts by stimulating alpha adrenergic receptors in blood vessels and can be used to help with symptomatic orthostatic hypotension.6 Fludrocortisone, a mineralocorticoid, has also been used to help retain salt and maintain intravascular volume.7 Salt tablets are used fur a similar purpose. Side effects of these medications include the development of hypertension, especially in those who are susceptible to AD, and lower extremity edema.
Deep Venous Thrombosis
Deep venous thrombosis (DVT) occurs in 47% to 100% of those with SCI with the highest incidence in the first 2 weeks postinjury.8 Paralysis of the lower extremities along with potential damage to the blood vessel walls due to trauma and the development of a hypercoagulable state all contribute to the development of this condition. These are referred to as Virchow's triad for the development of thrombosis.9 The potentially life threatening pulmonary embolism is the most serious complication along with persistent lower extremity swelling and clot propagation.
Prophylaxis and treatment of DVT is done primarily with anticoagulant medications. These include heparin sulfate, low molecular weight heparin, and warfarin (Coumadin). Heparin and related compounds act primarily at antithrombin III in the coagulation cascades to inhibit thrombin; whereas warfarin acts to inhibit the production of vitamin K dependent clotting factors.10 The main complication of these medications is an increased risk of bleeding, especially as treatment doses increase. Patients and therapists should both be aware of the increased likelihood of bleeding and signs and symptoms of excessive blood loss (fatigue, hypotension, tachycardia, and cool, clammy skin).
PAIN IN SPINAL CORD INJURY
Pain is noted in approximately two-thirds of patients with spinal cord injuries and may hinder their ability to meet functional goals.11 In studies investigating pain in people with SCI it has been found that 23% to 37% of patients would trade the possibility of bladder, bowel, and sexual function in return for pain relief.12 Pain is more commonly found when the injury is secondary to gunshot wounds or when the injury is due to violence.13 There has also been a strong inter-relationship between spasticity and pain, as well as a link between depression and pain.14 There is no definitive correlation between the completeness of injury and frequency of pain in the patient with SCI, and pain is less frequently found in patients that are more physically active.
There are a number of medications and interventions available for the spinal cord injured patient who has pain. Much of the treatment depends on the type of pain. Pain may be musculoskeletal, neuropathic, or visceral with the treatment. However, practitioners are often challenged in the management of pain as many times it falls within more than one of these classifications.
Musculoskeletal Pain
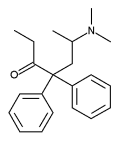
Following spinal cord injury there is frequently severe and acute pain related to the initial trauma. As a result of this pain the patient may not be able to tolerate therapies. Narcotics are often an option early in the course of injury. Examples of these medications (brand name in parenthesis) are as follows: codeine, propoxyphene (Darvon), hydrocodone (Vicodin), oxycodone (Roxicodone, Oxycontin-CR), morphine (MS Contin, Oramorph SR), hydromorphone (Dilaudid), meperidine (Demerol), methadone (Dolophine), and fentanyl (Duragesic).
Narcotic medications work as analogues to the endogenous opioids of the central nervous system (CNS) and act as agonists in at least 3 receptors (mu, kappa, & delta). The physiological effect is aimed at inhibiting the pain impulse to higher centers within the CNS and also at altering the individual's response to the pain.15 All of these medications share a similar side effect profile. Common side effects include constipation, sedation, respiratory depression, urinary retention, and the possibility of dependency.Tolerance may also develop with long-term use.15
Over time, the pain from acute trauma subsides and the SCI patient is slowly weaned from the stronger narcotics to milder medications. Tramadol (Ultram) is a common 'stepdown' medication. Tramadol has been shown to have a dual action. It acts partially as an opioid agonist, however to a much lesser degree and also as a monoaminc uptake inhibitor.15 Side effects are milder than for the stronger opioids, however this medication does lower seizure threshold.
Muscle spasms are another source of pain after SCI. When these spasms cause pain, muscle relaxants are used. A positive aspect of these medications is that they may decrease the need for narcotics.16 However, these medications commonly cause sedation and may slow progress in the rehabilitation setting and should be used only when physical modalities are either contraindicated or ineffective. A list of some muscle relaxants derived from the benzodiazepine family are as follows: Carisprodol (Soma), Chlorzoxazone (Paraflex), Cyclobenzaprine (Flexeril), Diazepam (Valium), Metaxalone (Skelaxin), Methocarbamol (Robaxin), Orphenadrine (Norflex).
Nonsteroidal anti-inflammatory drugs (NSAIDs) are another class of medications frequently used to manage musculoskeletal pain. The NSAIDs act to inhibit the enzyme cyclooxygenase, which is responsible for the production of pain mediating substances, prostaglandins, and thromboxanes. These compounds are involved in many functions within the body including the mediation of pain, inflammation, fever, anti-platelet effects, gastric mucosal health, and renal homeostasis. All of these medications share a similar side effect profile. Gastric complications (upset stomach, GI bleed) as well as kidney and liver problems may result from use of these medications. Also, there is some concern that the healing potential of bone may be reduced with the use of NSAIDS.17 Nonsteroidal anti-inflammatory drugs commonly used in the rehabilitation medicine setting are aspirin, ibuprofen (Motrin), naproxen (Naprosyn), indomethacin (Indocin), and ketorolac (Toradol). Recently, the development of a new class of NSAIDs has been developed. These medications are similar to other NSAIDs but act specifically at the cyclooxygenase-2 (COX-2) subtype. This enzyme has been shown to selectively inhibit the pathway that is directed primarily at the prostaglandins that gencrate pain and inflammation and thus have a much better gastrointestinal tolerability.18 Examples of these medications are Celecoxib (Celebrex), Refecoxib (Vioxx), and Meloxicam (Mobic).
The treatment of pain is as much an art as it is a science. Therefore, there is no one 'cocktail' that can help treat every patient's pain. Rather, the clinician and patient work in conjunction to find the appropriate regimen of medications to help treat pain.
Neuropathic Pain
The first line pharmacological agent used to treat neuropathic pain is the anti-epileptic drug (AED), Gabapentin (Neurontin). Gabapentin structurally looks very similar to the GARA neurotransmitter however it does not interact with the GABA receptor. Actually the precise mechanism of Gabapentin is not known.19 Carbamazepine (Tegretol), another AED, has also been efficacious in the treatment of neuropathic pain. Carbamazepine acts to block the conductance of sodium channels.20 Its most significant side effects include bone marrow suppression and an elevation of liver enzymes so these parameters must be monitored periodically. Anti-epileptic drugs, like narcotics and muscle relaxants, also produce sedation that can interfere with rehabilitation.
In addition to AEDs, tricyclic antidepressants (TCAs) have been used to decrease neuropathic pain. Examples of these medications include amitriptyline (Elavil), doxepin (Sincquan), and nortriptyline (Pamelor). The exact mechanism of pain control is not known; however, their mechanism of action is to inhibit the reuptake of the neurotransmitters serotonin and norepinephrine.20 These medications have anticholinergic side effects that include dry mouth, constipation, and urinary retention. The TCA medications also result in sedation (which sometimes may aid in sleep), alteration of heart rhythm and in some cases may increase spasticity.21
2Sometimes more invasive procedures are required to treat pain in SCI. Details of such interventions are beyond the scope of this article but examples are intrathecal medications (see article by Ibrahim et al in this issue), dorsal root ablation, spinal cord stimulators, and deep brain stimulation.
DEPRESSION
The incidence of depression in SCI varies in different studies, but it is generally thought to be about 25% for men and 47% for females.22 The suicide rate in spinal cord injured patients is anywhere from 2 to 6 times the rate in the able bodied population.23 Although one would think that the more severely injured (ie, ASIA A and B) would be more likely to commit suicide, a recent study actually showed the rate higher for patients with ASIA C and D injuries.24
Depression can have considerable negative effects on the patient with SCI. It has been associated with decreased functional gains and has been found to correlate with increased urinary tract infections, pressure ulcers, and medical expenses.25 Some overall risk factors for depression in the spinal cord injured patient are as follows: personal or family history of depression, chronic pain, female gender, poor social support network, other life stresses, medical problems, and substance/alcohol abuse. Specific to SCI, complete injury with coexistent traumatic brain injury are risk factors for depression.26 Certain medications such as steroids, histamine-2 blockers, and alpha-2 agonists can also contribute to depression.
Counseling by the psychologist plays an important role in most acute rehabilitation settings. While counseling is important and sometimes helpful for the patient's depression, pharmacological treatment also may be necessary. Medications treating depression most commonly facilitate the transmission of the neurotransmitters serotonin and/or norepinephrine and include venlafaxine (Effexor), sertraline (Zoloft), fluoxctine (Prozac) and mirtazapine (Remeron). Numerous options are available for the treatment of depression and all have a side effect profile of varying degrees of sedation and anticliolinergic effects such as blurred vision, dry mouth, and constipation (see Schleifer and Patel in this issue).27
SPASTICITY
Spasticity is defined as a motor disorder that is characterized by a velocity-dependent increase in tonic stretch reflexes with exaggerated tendon jerks, resulting from hyperexcitability of the stretch reflex.28 The incidence of Spasticity in the spinal cord injured patient was found to be 67%, with 37% requiring treatment by the time of discharge from rehabilitation. These figures increase to 78% and 49% respectively, by the time of the first annual follow up visit.29
It is not always necessary to treat Spasticity as sometimes it may actually be of benefit to the patient. Spasticity should only be treated if it interferes with function, has the potential to cause contractures, negatively affect seating in a wheelchair, or cause significant pain. Pharmacological treatment of Spasticity may also unmask underlying weakness in muscles and thus make some functional tasks more difficult.
Spasticity may be exacerbated by other noxious stimuli. Examples of these include urinary tract infections (UTI), bladder stones, bowel impaction, skin breakdown, heterotopic ossification, fractures, DVT, and abdominal pathology. Treatment of these conditions will often allow the spasticity to abate or return to the baseline and thus they are important to recognize. If spasticity abruptly increases and no obvious cause is identified, further investigation by a physician is warranted.
Use of medications in the treatment of spasticity requires careful titration of drugs to achieve the correct balance of tone and side effects. Baclofen is a first line agent for spasticity of spinal origin. It works as a GAHA (gamma-amino-butyric acid, an inhibitory neurotransmitter) agonist and binds prcsynaptically at the GABA^sub b^ receptor.30 Baclofen has been found to decrease flexor spasms, increase range of motion, and decrease tone. Potential side effects of Baclofen that may be problematic during physical therapy are sedation, fatigue, weakness, nausea, dizziness, paresthesias, and hallucinations. One must be careful when discontinuing baclofen as it needs be weaned slowly. If this medication is stopped abruptly, patients have been reported to have seizures, visual disturbances, and hallucinations.31
Benzodiazepines are also used to treat spasticity. Like Baclofen, these medications enhance the affect of the inhibitory neurotransmitter GABA by binding presynaptically at the GABAa receptor.30 The primary medication used in this class is diazepam (Valium). Side effects with this medication that may negatively affect therapy include sedation, hypotension, and depression. The sedative side effects may interfere with the ability of the patient to stay awake and participate in therapies and therefore doses should be started low and advanced slowly. In addition, this class of medication should not be used in a spinal cord injured patient with a concomitant brain injury because they have been Ibund to inhibit new learning and memory recovery.32
The class of medications known as alpha 2-adrenergic agonists has also been used to treat spasticity. Examples of these medications include clonidine (Catapress) and tizanidine (Zanaflex). These agents bind to presynaptic alpha-2 receptors in the dorsal horn of the spinal cord and result in a decrease of polysynaptic reflexes by decreasing the release of excitatory neurotransmitters and facilitation of inhibitory neurotransmitters.33 As with the benzodiazepines, these medications can cause fatigue and hypotension (clonidine is also used as an anti-hypertensive agent). Bradycardia is also a side effect seen with clonidine, and to a lesser extent, tizanidine. Therefore, attention must be paid to vital signs during physical therapy for patients on these medications.
Dantrolene sodium (Dantrium) is an agent that is used to reduce spasticity by acting directly on the muscle.This medication works by preventing calcium from being released from the sarcoplasmic reticulum and thus preventing muscle contraction.34 Sedation is less problematic with dantrolene than with benzodiazepines and the alpha-adrenergic agonists. However, liver toxicity is a concern with dantrolene and frequent monitoring of the liver transaminases need to be conducted.
Intrathecal baclofen pumps are designed to locally administer, using a catheter, into the spinal cord, a small dose of the drug, thus limiting systemic side effects. The catheter is tunneled to the spine at the L4-L5 level and the tip is threaded up to the L1 level. Implantation of the pump into the abdomen is performed only after the patient passes a baclofen screening protocol confirming that the medication is effective at reducing tone. Complications associated with the pump include infection and dislodgement, kinking, or blockage of the catheter. Pump malfunction may be associated with either baclofen overdose or withdrawal. Signs of overdose include sedation, confusion, hypotonia, respiratory depression, and even coma. Signs of withdrawal include increased tone, hyperthermia, puritis, agitation, and hallucinations. Intrathecal baclofen is more effective at reducing lower extremity tone than upper extremity spasticity due to the location of the catheter. Frequent evaluation of tone by both the physician and therapist is important in determining dose. Modalities such as ultrasound, electrical stimulation or any other deep heat treatment are contraindicated over the pump site or catheter tubing."
Nerve blocks with injections of phenol or absolute alcohol have been used to help spasticity. These techniques generally destroy the axon of the nerve and thus directly remove nerve impulses to muscles. The length of the effect of this medication is variable depending on the technique but can last up to several years. Ten percent of patients receiving phenol injections end up with disabling paresthesias.33
Botulinum toxin is another medication that has been used to reduce spasticity. The medication is injected directly into the muscle. It acts at the presynaptic nerve terminal and prevents the release of acetylcholine at the neuromuseular junction, essentially paralyzing the muscle. In general, the onset of action for botulinum toxin is 4 to 7 days with a peak at about 2 weeks and a length of effect from 3 to 6 months. The advantage of injecting botox directly into the spastic region, is that systemic side effects (ie, sedation seen in benzodiazepines and baclofen) are avoided.33
HETEROTOPIC OSSIFICATION
Heterotopic ossification (HO) is the formation of true bone in ectopic sites, usually around joints. The incidence in SCI is approximately 50% with about 20% experiencing significant loss in ROM.35 Heterotopic ossification usually develops within 1 to 4 months after injury; however, late occurrence has also been noted.36 The hip is the most common place of presentation of HO but it may also be present in any joint below the level of the injury.35
Clinical presentation of HO includes fever, edema, warmth, and decreased range of motion (ROM) around a specific joint. The presentation may be similar to other serious conditions such as DVT, infection, or fracture so the presence of these diagnoses must be ruled out.
There is no definitive treatment for HO; the goals of management include maintaining functional ROM and limiting the formation of ectopic bone as much as possible. Careful ROM exercises a mainstay in the management of HO, appear to be beneficial in maintaining range of motion and does not accelerate the formation of ectopic bone.37 Etidronate (Didronel), a bisphosphonate, is the only FDA approved medication in the treatment of HO. Etidronate blocks the late phase of bone mineralization but has no effect on the early stage of osteoid production.38 Common side effects present in 10% to 20% of patients are mostly gastrointestinal (ie, esophagitis, abdominal pain, nausea, and vomiting).39 It is unclear what effect etidronate has on bone healing. Other treatments of HO include the use of NSAIDs, radiation, and surgery.
BLADDER DYSFUNCTION IN SPINAL CORD INJURY
Bladder dysfunction is another common problem for individuals with SCI. Complications from a neurogenic bladder may include urinary tract infections (UTI), kidney stones, and renal damage. In addition maintenance of urinary continence is important for social integration. Autonomic dysreflexia is also a significant side effect of an over distended bladder and is an important factor in deciding which methods of bladder drainage will be used.40
In a healthy individual, voiding is under volitional control and activated primarily by the autonomic nervous system. The sacral micturition center in the conus medullaris portion of the spinal cord is the parasympathetic nucleus that regulates the bladder detrusor muscle to contract and promote voiding. The neurotransmitter used in the parasympathetic nervous system is acetylcholine and its primary effect is to stimulate the bladder detrusor to contract and thus empty the bladder. In contrast, the sympathetic nervous system with its adrenergic receptors exits the spinal cord at the low thoracic and upper lumbar regions. Its primary neurotransmitter is norepinephrine and its main function is to promote storage of urine. There are alpha-receptors located in the internal sphincter which, when stimulated, contract to prevent leakage of urine from the bladder. In addition, beta-receptors are present throughout the detrusor muscle and when activated, produce relaxation of the bladder to promote storage. With SCI, there is limited or absent volitional input to these centers to control voiding. Under most conditions however, they will continue to act under reflex control and will often act in an uncoordinated fashion.41
There are 2 general patterns of bladder dysfunction for individuals with SCI. Those with suprasacral injuries will have detrusor hyperreflexia. These patients will have unopposed detrusor contractions with small volume bladders and incontinence. Those with cauda equina syndrome will have a flaccid areflexic bladder. These patients will have large capacity bladders with little to no capability of producing voluntary bladder contractions. Each individual will undergo a urodynamic study to determine the specific type of bladder dysfunction and aid in determination of appropriate and effective methods of bladder drainage. Common methods of bladder drainage include intermittent catheterization (IC), reflex voiding with a condom catheter (useful for men only), indwelling Foley/suprapubic catheter, or surgical bladder augmentation. The type of bladder dysfunction, upper extremity function, availability of assistance, and secondary medical conditions determine the specific method of urinary drainage. In addition, there are numerous medications available to help maintain bladder health and continence. The medications which are often used for long-term management, their mode of action, and side effect profiles are discussed below.
Anticholinergics
This class of medication is probably the most commonly used for bladder dysfunction caused by SCI. These medications are used primarily in those who have detrusor hyperreflexia to relax the bladder detrusor muscle. They act by blocking the acetylcholine receptors within the bladder detrusor muscle and thus prevent uninhibited bladder contractions and allow the bladder to hold a larger volume of urine, and therefore help prevent unwanted episodes of incontinence.40 Medications in this class include: oxybutynin (Ditropan), tolteridine (Detrol), and propanthelene.
The side effect profiles of these medications include dry mouth, constipation, pupillary dilatation and blurred vision, drowsiness, and tachycardia.40 Some longer acting formulations of oxybutynin and tolterodine have been developed to lessen the anticholinergic side effects (particularly the dry mouth) and allow the medications to be taken once daily. It should also be said that the dry mouth induced by anticholinergic medications might stimulate the patients to drink more to counteract this side effect. By increasing fluid intake, the SCI patient will then make increased urine volume and potentially cause more detrusor hyperreflexia and incontinence. Thus it is important to determine the correct balance of anticholinergic medication and fluid restriction that works best for each individual. Some tricyclic antidepressants may also be used to inhibit bladder contractions, as they also possess anticholinergic effects.42
Alpha adrenergic blockers
Those who use reflex voiding for their method of bladder drainage may benefit from the addition of alpha-adrenergic blockers. These agents have shown significant improvement in bladder emptying by decreasing the residual urine volume.43 They work by relaxing the smooth muscle sphincter at the base of the bladder and thus lessen the force required by the bladder muscle to empty. Some common medications in this class include tamsulosin (Flomax), terazosin (Hytrin), doxazosin (Cardura), and prazosin (Minipress).
The main side effect of these medications is hypotension as alpha receptors also exist within the blood vessel walls. These effects may be desirable if the patient also has hypertension. However, most people with SCI tend to have a baseline low blood pressure (systolic blood pressure
BOWEL DYSFUNCTION IN SCI
Many individuals with SCI consider bowel dysfunction is considered a major life-limiting problem.44 The loss of voluntary control and the fear of having a bowel accident in public often will prevent people from participation in social activities. In addition, it is always important to consider constipation and/or fecal impaction as a cause of autonomic dysreflexia.
Bowel programs in SCI are designed to train the bowel to empty at regular and predictable times. In general, patients who have sustained a SCI demonstrate 2 types of neurogenic bowel patterns. An 'upper motor neuron' bowel describes the loss of voluntary control but retention of reflex activity (bulbocavernosus and other sacral reflexes). A 'lower motor neuron' bowel (usually from a cauda equina injury) lacks voluntary control as well as reflexive control and responds less successfully to bowel programs. The bowel program is designed to use the intact reflexes (if present) along with a combination of diet and pharmacological agents to achieve an effective, predictable program.45
There are 4 main categories of medications used in the treatment of the neurogenic bowel: stool softeners, bulkforming agents, stimulants, and contact irritants. Many of these can be started initially after the injury and gradually be discontinued. Others may be used occasionally when problems develop.
Stool Softeners
Individuals with SCI may need some help to keep their stools soft and formed. Docusate sodium (Colace) is a stool softener that can be taken orally. It acts by emulsifying fats within the GI tract and decreases the amount of water reabsorbed back into the circulation through the large intestine.45 It is important that these medications be taken with plenty of water to maintain adequate hydration. Obvious side effects of stool softeners are loose and runny stools contributing to incontinence. It is necessary to titrate the dose to find the correct balance between hard and loose stools.
Bulk Formers
Bulk-forming agents act within the colon to increase water absorption back into the body and thus increase the bulk of the stool. This is often helpful when the stools are loose and runny. Adequate fluid intake is also necessary to prevent impaction or obstruction45 and excessive use may lead to diarrhea. Common bulk forming agents include psyllium, calcium polycarbophil, and methylcellulose. These preparations are available in a variety of commercial preparations.
Stimulants
Stimulants are used in bowel programs to enhance peristalsis by stimulation of the enteric nervous system. Senna is one commonly used stimulant preparation. It is taken orally 6 to 12 hours prior to the designated elimination time. Side effects include cramping, and long-term use can lead to a cathartic colon (decreased effectiveness over time) or melanosis coli.46 Stimulants typically do not work well in the 'lower motor neuron' type injury.
Contact Irritants
Contact irritants act to directly irritate the bowel wall and thus directly induce peristalsis.47 These agents can be taken by mouth, suppository, or in enema preparations. As with stimulants, they tend not to work with 'lower motor neuron' type injuries. Common agents include bisacodyl (Dulcolax, Magic Bullet,Therevac, Fleets) and glycerin suppositories. Side effects tend to be local irritation in those with some sensation. Oral preparations can also lead to cramping and are usually taken 6 to 12 prior to desired program. Suppositories or enemas can take from 15 minutes to 2 hours prior to the elimination time depending on the preparation.
Laxatives
Laxatives may be useful to help clean out the bowels. Sodium, potassium, and magnesium salts (ie, magnesium citrate or Milk of Magnesia) act by drawing fluid into the colon to stimulate peristalsis.45 Other laxatives are metabolized within the intestine (GoLytely, Miralax, Lactulose) and also draw fluid into the colon. Laxatives are not typically the primary agent used in a bowel program and tend to be used only when there is significant constipation. Enemas can also be used in an as needed basis as well.
CONCLUSION
Spinal cord injury was once thought of as 'an ailment not to be treated.' Today, survival of SCI has increased and patients are living longer. As a result more emphasis has been placed on treating the complications that arise from SCI. Pharmacological interventions have played a crucial role in the positive outcomes of those with SCI. These agents are very useful, but they must be used with an understanding of their mechanisms and side effects.
REFERENCES
1 National Spinal Cord Injury Statistical Center Statistics at a Glance. Available at: http://www.spinalcord.uab. edu. Accessed May 1, 2001.
2 Teasell RW, Arnold JM, Krassioulkov A. Cardiovascular consequences of loss of supraspinal control of the sympathetic nervous system after spinal cord injury. Arch Phys Med Rehabil 2000;81(4):506-516.
3 Braddom RL, Rocco JF. Autonomic dysreflexia: a survey of current treatment. Am J Phys Med Rehabil. 1991;70:234-241.
4 Linsenmeyer TA, Campagnolo DI, Chou IH. Silent autonomic dysreflexia during voiding in men with spinal cord injuries. J Urol. 1996;155:519-522.
5 Clinical Practice Guidelines:Acute management of autonomic dysreflexia. J Spinal Cord Med. 1997;20:284-318.
6 Barber DB, Rogers SJ, Fredrickson MD, et al. Midodrine hydrochloride and the treatment of orthostatic hypotension in tetraplegia: two cases and a review of the literature. Spinal Cord. 2000;38:109-111.
7 Campagnolo DI, Merli G. Autonomic and cardiovascular complications of spinal cord injury. In: Kirshblum S, Campagnolo DI, DeLisa JA, eds. Spinal Cord Medicine. Philadelphia, Pa: Lippincott; 2002:123-134.
8 Merli G, Herbison, G, Ditunno J, et al. Deep venous thrombosis: prophylaxis in acute spinal cord injured subjects. Arch Phys Med Rehabil. 1988;69:66l-664.
9 Virchow R. Neurer fall von todlichen: emboli der lungenaterie. Arch Pathol Anat. 1856;10:225-228.
10 Harker LA. Antithrombotic therapy. In: Goldman L, Bennett JC, eds. Cecil's Textbook of Medicine. 21st ed. Philadelphia, Pa: WB Saunders; 2000:1021-1028.
11 Yezierski RP, Pain following spinal cord injury: the clinical problem and experimental studies. Pain. 1996;68:185-194.
12 Bonica, Introduction: semantic, epidemiologic, and educational issues. In: casey KL, ed. Pain and Cenral Nervous System Sisease, The Central Pain Syndromes, New York, NY: Raven Press; 1991.
13 Richards JS, Stover SL, Jaworski T. Effect of bullet removal on subsequent pain in persons with spinal cord injury secondary to gunshot wound. J Neurosurg. 1990;73:401-404.
14 Fenellosa P, Pallares J, Cervera J, et al. Chronic pain in the spinal cord injured: statistical approach and pharmacological treatment. Paraplegia. 1993;31:722-729.
15 Stitik TP, Klecz R, Zafonte RO, et al. Pharmacotherapy of disability. In: DeLisa JA, Gans BM, ed. Rehabilitation Medicine: Principles and Practice. 3rd ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 1998:789-828.
16 Cioni B, Meglio M, Pentimalli L, et al. Spinal cord stimulation in the treatment of paraplegic pain. J Pain Symptom Manage. 1995;82(l):35-39.
17 Chesnut C, Baylink D, Doyle H, et al. Salmon-calcitonin nasal spray prevents vertebral fractures in established ostcoporosis. Further interim trials of the "PROOF" study. ECO Abstract, OP INT. 1998:813.
18 Hawkins C, Hanks GW. The gastroduodenal toxicity of nonsteroidal anti-inflammatory drugs: a review of the literature. J Pain Symptom Manage. 2000;20:140-151.
19 Tai Q, Kirshblum S, Chen B, et al. Gabapentin in the treatment of neuropathic pain after spinal cord injury: a prospective, randomized, double-blind, crossover trial. J Spinal Cord Med. 2002;25(2) 100-105.
20 Sandford PR, Lindblom LB, Haddox JD. Amitriptyline and carbamazepime in the treatment of dysesthetic pain in spinal cord injury. Arch Phys Med Rehabil. 1992;73(3):300-301.
21 Anghene P, van Houdenkove B. Antidepressant-induced analgesia in chronic non-malignant pain: a metaanalysis of 39 placebo controlled studies. Headache. 1994;34:44-49.
22 Fuhrer MJ, Rintala DH, Hart KA, Clearman R,Young ME. Depressive symptomatology in persons with spinal cord injury who reside in the community, Arcb Phys Med Rahabil. 1993;74:255-260.
23 Heinemann AW Spinal cord injury. In: Goreczny AJ, ed. Handbook of Health and Rehabilitation Psychology. New York, NY: Plenum Press; 1995:341-360.
24 Hartkopp A, Bronnum-Hansen H, Seidensclinur AM, Biering-Sorensen F. Suicide in a spinal cord injured population: its relation to functional status. Arch Phys Med Rehabil. 1998;79:1356-1361.
25 Consortium for Spinal Cord Medicine, Depression Following Spinal Cord Injury: A clinical practice guideline for primary care physicians. Paralyzed Veterans of America. August, 1998.
26 Fichtenbaum J, Kirshblum S. Psychologic adaptation to spinal cord injury. In: Kirshblum S, Campagnolo DI, DeLisa JA, eds. Spinal Cord Medicine. Philadelphia, Pa: Lippincott; 2002:299-311.
27 Consortium for Spinal Cord Medicine. Depresion Following Spinal Cord Injury: A Clinical Practice Guideline for Primary Care Physicians. New York, NY: Paralyzed Veterans of America; 1998.
28 Lance JW. Symposium synopsis. In: Feldman RG, Young RR, Koella WP, eds. Spasticity: Disordered Motor Control. Chicago, Ill: Mosby Year Book; 1980:17-24.
29 Maynard FM, Karunas R, Waring WW. Epidemiology of spasticity following traumatic spinal cord injury. Arch Phys Med Rehabil. 1990;71:566-569.
30 Kirshblum S. Treatment alternatives for spinal cord injury related spasticity. J Spinal Cord Med. 1999;22(3):199-217.
31 Rivas DA, Chancellor MB, Hill K, et al. Neurological manifestations of baclofen withdrawal. J Urol. 1993;150(6):1903-1905.
32 Zafonte RD, Elovic E. Dual diagnosis: traumatic brain injury in a person with spinal cord injury. In: Kirshblum S, Campagnolo DI, DeLisa JA, eds. Spinal Cord Medeicine. Philadelphia, Pa: Lippincott; 2002:261-274.
33 Priebe MM, Goetz LL, Wuermser LA. Spasticity following spinal cord injury. In: Kirshblum S, Campagnolo DI, DeLisa JA, eds. Spinal Cord Medicine. Philadelphia, Pa: Lippincott Williams & Wilkins; 2002:221-233.
34 Herman R, Mayer N, Mecomber SA. The pharmacophysiology of dantrolene sodium. Am J Phys Med 1972;51:296-311.
35 Banovac K, Gonzalez E Evaluation and management of heterotopic ossification in patients with spinal cord injury. Spinal Cord. 1997;35:158-162.
36 Garland DE.A clinical perspective on common forms of acquired heterotopic ossification. Clin Orthop Related Res 1991;263:13-29.
37 Stover SL, Hataway CJ, Zeiger HE. Heterotopic ossification in spinal cord-injured patients. Arch Phys Med Rehabil. 1975;56:199-204.
38 Francis MD, Russell RGG, Fleisch H. Disphosphonates inhibit formation of calcium phosphate crystals in vitro and pathological calcification in vivo. Science. 1969; 165:1964-1966.
39 Stover SL, Hahn HR, Miller JM. Disodium etidronate in the prevention of heterotopic ossification following spinal cord injury (preliminary report). Paraplegia. 1976;14:146-156.
40 Wyndale JJ. Pharmacothcrapy for urinary bladder dysfunction in spinal cord injury patients, Paraplegia. 1990;28:146-150.
41 Linsenmeyer TA. Neurogenic bladder following spinal cord injury. In: Kirshblum S, Campagnolo DI, DeLisa JA, eds. Spinal Cord Medicine. Philadelphia, Pa: Lippincott; 2002:181-206.
42 Baldessarini RJ. Drugs and the treatment of psychiatric disorders. In: Gilman AG, Rail TW Nies AS, et al, eds. Goodman and Gilman's The Pharmacological Basis of Therapeutics. 8th ed. New York, NY: Pergamon Press; 1990;383-35.
43 Scott MB, Morrow JW. Phenoxybenzamine in neurogenic bladder dysfunction after spinal cord injury: I. Voiding Dysfunction. J Urol. 1978;119:480-482.
44 Stone JM, Nino-Murcia M, Wolfe VA, et al. Chronic gastrointestinal problems in spinal cord injury patients: a prospective analysis. Am J Gastroenterology. 1990;85:1114-1119.
45 Chen D, Nussbaum SB. Gastrointestinal disorders. In: Kirshblum S, Campagnolo DI, DeLisa JA, eds. Spinal Cord Medicine. Philadelphia, Pa: Lippincott; 2002:155-163.
46 Gattuso JM, Kamm MA. Adverse effects of drugs used in the management of constipation and diarrhea. Drug Saf. 1994;10:47-65.
47 House JG, Stiens SA. Pharmacologically initiated defecation of persons with spinal cord injury: effectiveness of three agents. Arch Phys Med Rehabil. 1997;78:1062-1065.
William Scelza, MD1
Matthew Shatzer, DO1
1Fellows, Spinal Cord Injury Medicine, The Kessler Institute for Rehabilitation/UMDNJ New Jersey Medical School, West Orange, New Jersey (wsclexa@umich.edu)
Copyright Neurology Report Sep 2003
Provided by ProQuest Information and Learning Company. All rights Reserved