Keywords: Chinese medicine, electroacupuncture, depression, maprotiline
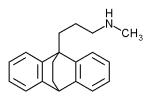
Maprotiline is an antidepressant which was first introduced in 1974. It is no longer used very much in the US due to newer, more effective antidepressants, but its use is still common in some other countries. It is thought that this drug works by slowly restoring the neurotransmitter norepinephrine to normal levels in the brain. Some benefit from this drug may be observed in the first 1-2 weeks. However, adequate response may require 4-6 weeks or longer of continual use. Possible natural, expected, and unavoidable drug actions include drowsiness, blurred vision, dry mouth, constipation, and impaired urination. Mild adverse reactions may include allergic reactions, insomnia, nervousness, heart palpitation, tremors, nausea, vomiting, acid indigestion, and diarrhea. Serious adverse reactions may include anxiety, confusion, hallucinations, and liver toxicity with jaundice. Generally, long-term use should not exceed six months without evaluation regarding the need for continuation of this drug.
Since long term use is not suggested for maprotiline, other, safer methods of treating clinically depressed patients without potential adverse reactions are useful and acupuncture has much to offer in this regard. In issue #6, 2002 of the Zhong Yi Za Zhi (Journal of Chinese Medicine), Han Gui, Li Xiao-hong, Luo He-chun, et at. published an article titled, "A Clinical Audit of the Treatment of 30 Cases of Depression with Electroacupuncture." This article appeared on pages 428-430 of that journal. In this study, electroacupuncture was compared to maprotiline for effectiveness and safety. Aprecis of that study is given below.
Cohort description:
Altogether, there were 61 patients in this study, 25 males and 36 females aged 18-56 years, with a median age of 35.41 [+ or -] 12.63 years. These patients had suffered from depression for two months to 15 years, with a mean duration of 40.94 [+ or -] 50.24 months. All these patients were seen as out-patients at the Beijing University Mental Health Institute and all met ICD-b and CCMD-2R criteria for depression. In each patient's case, the Hamilton Depression Scale rating was equal to or in excess of 20 points and the Self-rating Depression Scale was equal to or above 53 points. These 61 patients were divided into two groups. Thirty patients were assigned to the treatment group and 31 patients were assigned to the comparison group. (Initially, there were 31 patients in the treatment group and 35 in the comparison group, but one patient in the treatment group committed suicide and four patients in the comparison group dropped out due to unacceptable adverse reactions to maprotiline.) In terms of Chinese medica l pattern discrimination, there were nine cases of liver depression-spleen vacuity, 13 cases of heart-spleen dual vacuity, and eight cases of liver-kidney yin vacuity in the treatment group. In the comparison group, there were 10 cases of liver depression-spleen vacuity, 14 cases of heart-spleen dual vacuity, and seven cases of liver-kidney yin vacuity. Therefore, in terms of sex, age, disease severity, and disease duration, there were no significant statistical differences between these two groups. (P >0.05)
Treatment method:
Members of the treatment group all received electroacupuncture at Bai Hui (GV 20) and Yin Tang (M-HN-3). Patients exhibiting a pattern of liver depression-spleen vacuity also received electroacupuncture at Yang Ling Quan (GB 34) and San Yin Jiao (Sp 6). Those manifesting a heart-spleen dual vacuity also received electroacupuncture at Nei Guan (Per 6) and San Yin Jiao (Sp 6), while those exhibiting a liver-kidney yin vacuity pattern also received electroacupuncture at Tai Xi (Ki 3) and San Yin Jiao (Sp 6). Electroacupuncture was performed with fine needles and a WQ-6F machine and the degree of stimulation was whatever the patient could bear. One treatment was given per day with each treatment lasting 45 minutes. Six treatments were administered per week with a one day rest each week. Six weeks equaled one course of treatment.
Members of the comparison group received 75-250mg of maprotiline per day, with a mean administration of 174.22 + 46.44mg per day. They also received treatment for six weeks.
Treatment outcomes:
Cure was defined as disappearance of psychiatric symptoms and a reduction in Hamilton Depression Rating Scale of eight points. Marked effect was defined as basic disappearance of psychiatric symptoms and a reduction in Hamilton Depression Rating Scale of 50% or more. Some effect was defined as decrease in psychiatric symptoms and a decrease in Hamilton Depression Rating Scale of 35-50%. No effect meant that reductions in Hamilton Depression Rating Scale were less than 25%. Based on these criteria, 12 cases (40%) in the treatment group were judged cured, 11 (3 6.7%) got a marked effect, six (2 0%) got some effect, and one (3.3%) got no effect, for a total amelioration rate of 96.7%. In the comparison group treated with maprotiline, 14 cases (45.2%) were cured, nine (29%) got a marked effect, five (16.1%) got some effect, and three (9.7%) got no effect. Therefore, the total amelioration rate in this group was 90.3%. Thus there was no marked difference in effectiveness between this electroacupuncture protocol an d maprotiline. (P >0.05). However, there was a significant difference in the decrease of the cumulative scores of Chinese medical symptoms between these two groups, with a greater decrease in the treatment group than the comparison group. (P <0.05) Side effects from treatment were also rated according to the Asberg Scale, and the score of the treatment group was superior to that of the comparison group. Mean plasma cortisol and endothelin decreased significantly from before to after treatment in both groups, basically returning to normal. Therefore, this study suggests that electroacupuncture is just as effective as maprotiline for the treatment of depression but has far fewer side effects.
Being able to significantly improve symptoms of clinical depression without the expected side effects of drug therapy is, in my opinion, a notable result and more studies of this nature should be pursued by clinicians in the West.
For more information on the Chinese medical treatment of depression, see Bob Flaws & James Lake's Chinese Medical Psychiatry available from Blue Poppy Press.
COPYRIGHT 2003 The Townsend Letter Group
COPYRIGHT 2003 Gale Group