The Quality Standards Subcommittee of the American Academy of Neurology has released a report on postherpetic neuralgia treatment. "Practice Parameter: Treatment of Postherpetic Neuralgia" appears in the September 2004 issue of Neurology and is available online at http://www.aan.org.
Acute herpetic neuralgia is characterized as burning, aching, electric-shock--like pain, or unbearable itching in association with the outbreak of a herpes zoster rash. The pain is associated with dysesthesias, paresthesias, hyperalgesia, hyperesthesia, and allodynia (production of pain by innocuous stimuli). The pain may precede the onset of the herpetic rash and, rarely, herpetic neuralgia can occur without the development of a rash.
Postherpetic neuralgia, persistence of the pain of herpes zoster more than three months after resolution of the rash, is relatively common, affecting 10 to 15 percent of those with herpes zoster. Zoster-associated pain is used to describe the continuum of pain from acute herpes zoster to the development of postherpetic neuralgia. The time interval used in the clinical case definition of postherpetic neuralgia varies in the literature from one to six months after resolution of the rash. The incidence of postherpetic neuralgia increases with age. The duration of postherpetic neuralgia is highly variable.
Administration of antiviral agents within 72 hours of the onset of herpes zoster can reduce the intensity and duration of acute illness, and can prevent postherpetic neuralgia, as may the use of amitriptyline. Efforts at prevention of herpes zoster and postherpetic neuralgia are important in that 40 to 50 percent of those with postherpetic neuralgia do not respond to any treatment. The practice parameter focused on which treatments provide benefit in terms of decreased pain and improved quality of life. Among the findings and key recommendations are the following:
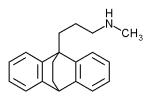
* Tricyclic antidepressants (amitriptyline, nortriptyline, desipramine, and maprotiline), gabapentin, pregabalin, opioids, and topical lidocaine patches are effective and should be used in the treatment of postherpetic neuralgia. There is limited evidence to support the use of nortriptyline over amitriptyline and the data are insufficient to recommend one opioid over another. Amitriptyline has significant cardiac effects in elderly patients when compared with nortriptyline and desipramine.
* Aspirin in cream may be effective in the relief of pain in patients with postherpetic neuralgia but the magnitude of benefit is low, as with capsaicin.
* In countries where preservative-free intrathecal methylprednisolone is available, it may be considered in the treatment of postherpetic neuralgia.
* Acupuncture, benzydamine cream, dextromethorphan, indomethacin, epidural methylprednisolone, epidural morphine sulfate, iontophoresis of vincristine, lorazepam, vitamin E, and zimelidine are not of benefit.
* The efficacies of carbamazepine, nicardipine, biperiden, chlorprothixene, ketamine, He:Ne laser irradiation, intralesional triamcinolone, cryocautery, topical piroxicam, extract of Ganoderma lucidum, dorsal root entry zone lesions, and stellate ganglion block are unproven in the treatment of postherpetic neuralgia.
* There is insufficient evidence at this time to make any recommendations on the long-term effects of these treatments.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group