Migraine symptoms improve in up to 70% of women during pregnancy. But in 4%-8% of women, migraines worsen, and as many as 16% of all migraine cases during pregnancy may be new onset.
A 2002 review identified drugs or drug classes used for preventing migraine attacks (N. Engl. J. Med. 2002;346:257-70), including four drugs available in the United States that were considered well-accepted treatments or had proved to be effective: metoprolol, propranolol, amitriptyline, and valproate. Verapamil (Calan, Isoptin) and selective serotonin-reuptake inhibitors (SSRIs) were also widely used, but the reviewers concluded that there was poor evidence of benefit. Gabapentin (Neurontin) and topiramate (Topamax) were considered promising for migraine prophylaxis.
Of these agents, only amitriptyline, verapamil, and low-dose propranolol (30-40 mg/day) have enough data to be classified as low risk during pregnancy. Higher doses of propranolol may cause intrauterine growth retardation (IUGR) and other fetal/neonatal toxicity. Based on the drug class (antihistamine and calcium channel blocker), flunarizine is probably compatible with pregnancy. Gabapentin and topiramate should be avoided in the first trimester because of inadequate human data. Valproate causes neural tube defects and other structural anomalies if used in the first trimester, and use of metoprolol during the second and third trimesters is associated with an increased risk of IUGR. SSRI use in the third trimester may cause newborn toxicity, and methysergide and other ergot alkaloids are contraindicated in pregnancy.
Other migraine drugs include acetaminophen (alone, or in combination with caffeine and butalbital, aspirin and caffeine, or isometheptene and dichloralphenazone): NSAIDs, including aspirin; chlorpromazine (Thorazine); dimenhydrinate (Dramamine); diphenhydramine (Benadryl); morphine; meperidine; intranasal butorphanol (Stadol); and corticosteroids.
Others are dihydroergotamine (Migranal, D.H.E. 45), ergotamine (Ergomar) (alone or in combination with caffeine, or caffeine-belladonna-pentobarbital), intranasal lidocaine, and selective serotonin receptor agonists, also called triptans.
Combination products with butalbital are not recommended because in studies, the butalbital component did not increase efficacy. Acetaminophen, caffeine, dimenhydrinate, diphenhydramine, narcotic analgesics, lidocaine, and butorphanol are of very low risk in pregnancy. However, frequent, prolonged use of narcotic analgesics may result in maternal and fetal addiction.
Several therapeutic agents can cause developmental toxicity. NSAIDs, including aspirin, have been associated with miscarriage when used around the time of conception, and exposure in the third trimester is tied to premature closure of the ductus arteriosus with the risk of persistent pulmonary hypertension of the newborn.
Aspirin causes irreversible inhibition of platelet function and other clotting disorders, so its use near term may result in enhanced maternal blood loss at delivery and an increase in the incidence of intracranial hemorrhage in premature or low-birthweight infants. Cortico steroid use in the first trimester is tied to a low risk of oral clefts. Ergot alkaloid preparations are contraindicated in pregnancy because of their dose-related developmental toxicity and oxytocic properties.
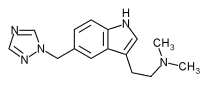
Seven triptans indicated for the short-term treatment of migraine with or without aura are available: sumatriptan (Imitrex), almotriptan (Axert), eletriptan (Relpax), frovatriptan (Frova), naratriptan (Amerge), rizatriptan (Maxalt), and zolmitriptan (Zomig). Triptans do not appear to be major teratogens in humans, but more data are needed.
In animal studies at doses or systemic exposures 10 times the human dose, triptans caused developmental toxicity. Human data are only available for naratriptan, sumatriptan, and rizatriptan. About 500 women have been prospectively enrolled since early 2004, about 90% with first-trimester exposure. Except for a small cluster of five ventricular septal defects, there was no consistent pattern of defects to suggest a common cause.
Other than ergot drugs (contraindicated) and amitriptyline (concern for long-term neurotoxicity), antimigraine agents appear to be compatible with breast-feeding. There are few or no data available for gabapentin and topiramate. Ergot alkaloids may inhibit lactation; high doses have been associated with toxicity in nursing infants (vomiting, diarrhea, and convulsions). The effect of triptans on a nursing infant is unknown, but the small amount of drug in milk does not appear to represent a risk.
BY. GERALD G. BRIGGS, B. PHARM.
MR. BRIGGS is pharmacist clinical specialist, Women's Hospital, Long Beach Memorial Medical Center; clinical professor of pharmacy, University of California, San Francisco; and adjunct professor of pharmacy, University of Southern California, Los Angeles. He is also coauthor of the "Drugs in Pregnancy and Lactation."
COPYRIGHT 2005 International Medical News Group
COPYRIGHT 2005 Gale Group