criticalcare
Help relieve your patient's pain and teach her how to prevent or minimize future flare-ups.
Migraine affects nearly 28 million Americans, mostly women. Yet according to experts, migraine is underdiagnosed and undertreated. Many patients come to the emergency department (ED) with headache pain thats already out of control. In this article, I'll describe migraine pathophysiology and treatment and discuss how you can help your patient prevent and treat flare-ups.
Oh, my aching head
Migraine is a complex event, not just the result of vasodilation. A triggering event sets off a cascade of neurotransmitter releases, including calcitonin-- gene-related peptide, neurokinin A, and substance P. These activate serotonin receptors, causing a sterile inflammation of the surrounding trigeminal neurons and vasodilation. Eventually, pain sensations arise from stimulation of the thalamus and trigeminal nucleus caudalis. Autonomic stimulation causes nausea and vomiting, and involvement of the occipital area is thought to cause photophobia and phonophobia.
Migraines can be triggered by physical and emotional stressors. Physical triggers include illness, too little or too much sleep, missing meals, bright or flickering lights, strong odors, weather or seasonal changes, and hormonal changes, particularly sudden drops in estrogen. Foods may also trigger migraine, although patients may overestimate food's role in causing migraine. Offending foods include many pickled, fermented, or preserved foods such as salami, cheese, or freshly baked breads. Caffeine withdrawal, caffeinated drinks, alcoholic beverages, fruits, nuts, and chocolate have also been implicated.
Migraines have five distinct stages: the prodrome, aura (some migraines have no aura), headache phase, termination phase, and postdrome.
The prodrome may occur hours to days before head pain starts. Up to 60% of patients have a prodrome, which often includes food cravings, mood alterations, heightened sensory perception, excessive yawning, or muscle tightness. Although many different symptoms can occur in the prodrome, each patient tends to have individually consistent symptoms.
During the prodrome, hypothalamic changes occur under dopaminergic influences. Patients who crave certain foods during this time may blame these foods as triggers when the craving is actually part of the prodrome and not a triggering event.
Aura occurs in about 20% of migraines. Although it usually precedes head pain, it may occur with the onset of pain. Its commonly associated with visual effects such as scotoma (blind spot), diplopia, and fortification spectra (zigzag lines). Flashing lights, which may occur in the peripheral vision, are usually hemianopic (the patient experiences blindness in half of the field of vision) and are often associated with a nearby blank area, which may correlate with the way that neurochemicals spread through the brain. Other signs and symptoms of aura include transient focal neurologic events, such as hemiplegia, aphasia, or vertigo.
Auras usually wax and wane within an hour. Symptoms lasting over an hour should be considered a potential ischemic attack.
Head pain during the headache phase develops over several hours and lasts 24 to 72 hours in adults if untreated, but it may last less than 4 hours in children and adolescents. Pain may be unilateral or bilateral. Often described as throbbing or pounding, its aggravated by activity. Associated symptoms such as nausea, vomiting, mood swings, muscle pain, and diarrhea may occur or intensify. Patients often seek a dark, quiet room during this phase to avoid light and sound.
During the termination phase, head pain generally resolves over several hours.
Many patients report feeling wiped out during the postdrome, which includes feelings of fatigue, irritability, muscle pain, and sleepiness and can linger for a few days.
Assessing your patient
When a patient arrives in the ED with severe migraine pain, your first step in providing care is to take an appropriate history. Migraine is a familial disease: Up to 80% of patients have a positive family history for migraine. Because many patients haven't been diagnosed, be sure to ask your patient about family episodes of "sick" headaches or headaches requiring bed rest. (Patients may not seek help for migraines unless they become weary of symptoms, fear a serious condition such as a brain tumor, or can't control the pain with over-the-counter [OTC] medications.)
Remember to ask your patient specifically about her use of OTC medications and foods and products containing caffeine, as these may lead to rebound headache. Also ask about a history of allergies or food sensitivities, sleep and meal patterns, menstrual periods, and pregnancy history. Assessing the level of disability from headache, any change in headache patterns, frequency, and medication use during headaches can help guide therapy aimed at aborting headaches and reducing frequency and severity.
Consider other causes of severe head pain. Lab tests such as a complete blood cell count, thyroid stimulating hormone level, and erythrocyte sedimentation rate help to rule out metabolic and inflammatory causes of headache such as hyperthyroidism, anemia, and temporal arteritis.
To rule out tumors, meningitis, and subarachnoid hemorrhage, you may need to prepare your patient for diagnostic studies such as computed tomography and lumbar puncture. Patients who require more extensive diagnostic workups include those who are having their first severe headache after age 50; have onset of a new or different type of headache; are having the worst headache they've experienced; have headaches that are getting progressively worse over time; have onset of headache with sneezing, sexual activity, coughing, or other exertion; have impaired neurologic signs such as ataxia or meningeal irritation; or have other abnormal signs or symptoms such as fever, hypertension, stiff neck, or papilledema.
Treating migraine
How a patients migraine is treated depends on the level of disability associated with the specific headache episode. Therapy consists of abortive and preventive treatments. (See Tailoring Migraine Treatment.)
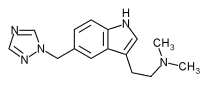
Abortive therapy-cerebral vasoconstrictor agents and analgesics-is used to decrease migraine severity and duration. The triptans are the most commonly used cerebral vasoconstrictor agents; others include ergotamine and dihydroergotamine. Analgesics, the second arm of abortive therapy, include butorphanol (Stadol), Fiorinal (butalbital with aspirin and caffeine), Midrin (isometheptene mucate, dichloralphenazone, and acetaminophen), and nonsteroidal anti-inflammatory drugs. Opioids sometimes are used if the patients pain can't be managed by nonopioid medications.
Effective nonpharmaceutical treatments include rest in a dark and quiet room and ice packs on the head or neck.
Preventive medication may be used to reduce headache frequency to a tolerable level, or about a 50% decrease in frequency. Five medications show clear evidence of effectively preventing migraine: amitriptyline (Elavil), propranolol (Inderal), timolol (Blocadren), divalproex sodium (Depakote), and methysergide (Sansert). However, many other medications are used to prevent migraine, including the beta-blocker atenolol, and calcium channel blockers such as verapamil.
Tricyclic antidepressants such as amitriptyline not only prevent headache recurrence, but also treat concomitant depression, which is a common comorbid condition. Selective serotonin reuptake inhibitors such as paroxetine (Paxil) and fluvoxamine (Luvox) can be used in patients who also use abortive medications such as triptans without fear of serotonin excess syndrome because these medications appear to affect a different subset of serotonin receptors.
Valproic acid reduces migraine occurrence, but serious adverse effects such as clotting abnormalities, liver dysfunction, and pancreatitis limit its use. Women of childbearing potential shouldn't get pregnant while using the drug because of the risk of birth defects. An alternative is gabapentin (Neurontin), which is well tolerated and prevents both headache and neuropathic pain.
Women who suffer from migraines related to the sudden drop in estrogen at the beginning of their menstrual cycle often benefit from the addition of an estrogen patch as their cycle begins. Prophylactic rizatriptan (Maxalt) or naratriptan (Amerge), taken 2 to 3 days before and then during menses, has been used with some success.
Alternative therapies such as magnesium, riboflavin, and botulinum toxic type A (Botox) injections are being studied for use in migraines. Studies have shown that smoking cessation is effective in reducing migraine, and relaxation and biofeedback techniques are also effective for some people.
Some patients may ingest feverfew, an herbal supplement, to relieve migraine, but this may cause stomatitis. St. John's wort, another herbal supplement, may be effective because of its effect on monoamine oxidase, but it shouldn't be used in patients taking triptans to treat acute migraine episodes because it speeds up blood clearance of triptans.
Taking charge
Because of the risk of serious drug interactions, teach patients to inform their primary care provider about all medications they take, including OTC drugs and herbal or dietary supplements. Also encourage your patient to take charge of her condition by making a follow-up appointment with a primary provider or specialist, who may suggest that she keep a headache diary to identify possible triggers and make lifestyle modifications to minimize the frequency and severity of recurrences.
SELECTED REFERENCES
Cady, R., and Dodick, D.: "Diagnosis and Treatment of Migraine," Mayo Clinic Proceedings. 77(3):255-261, March 2002.
Lofland, J., et al.: "Cost-Effectiveness and Cost-Benefit of Sumatriptan in Patients with Migraine," Mayo Clinic Proceedings. 76(11):1093-1101, November 2001.
Moloney, M., et al.: "Caring for the Woman with Migraine Headaches," Dimensions of Critical Care Nursing. 20(4):17-25, July/August 2001.
SELECTED WEB SITES
American Council for Headache Education: http://www.achenet.orgy/your Migraine Awareness Group: http//www.migraines.org
Last accessed on April 9, 2003.
BY KATHY KOLB-LUCAS, RN, CFNP, MSN
Kathy Kolb-Lucas is a family nurse practitioner with a background in primary care. She manages an anticoagulation clinic that she developed at Feather River Hospital in Paradise, Calif.
Copyright Springhouse Corporation May 2003
Provided by ProQuest Information and Learning Company. All rights Reserved