During December 13-19, 2004, Togo, a West African nation with a population of approximately 5 million, conducted the first-ever nationwide distribution of insecticide-treated bednets (ITNs) for prevention of malaria. A supplemental immunization activity (SIA), conducted as part of Togo's measles mortality reduction strategy and targeting all children aged 9-59 months, was used as an opportunity to distribute ITNs, oral poliovirus vaccine (OPV), and the anti-helminthic medication, mebendazole. The campaign aimed to achieve >95% coverage among the 866,725 children aged 9-59 months with measles vaccine, OPV, one ITN, and one tablet of mebendazole. This report describes the planning, implementation, and results of this campaign, with emphasis on ITN distribution. The findings demonstrate the feasibility of integrating delivery of these services in a campaign setting.
During 1995-2001, Togo experienced an annual average of 2,648 reported measles cases and 15 reported measles deaths; after the 2001 nationwide measles SIA that initiated Togo's measles mortality reduction activities, reported measles cases declined to 358 in 2002 and to 296 in 2003, while reported measles deaths declined to one and zero, respectively (unpublished data, Ministry of Health [MOH] of Togo, 2004). Malaria, endemic throughout Togo, accounted for approximately one quarter to one third of all deaths in Togolese children aged <5 years in 2003 (unpublished data, MOH, 2005); however, a morbidity survey in September 2004 revealed that only 0.4% of children in this age group slept under an ITN during the previous night (unpublished data, MOH, 2005). Although Togo's most recent wild poliovirus (WPV) case occurred in 2003, WPV circulation remains endemic in two West African countries, Niger and Nigeria (1). Soil-transmitted helminth infection is prevalent in West Africa, with children aged 2-5 years among those at greatest risk (2).
An Interagency Coordination Committee (ICC) for the MOH Expanded Program for Immunization (EPI) approved the campaign plan, mobilized resources, monitored campaign preparations, and disbursed funds. A National Steering Committee under ICC oversaw three groups: 1) the Technical Working Group, which prepared guidelines, reporting forms, and evaluation tools; 2) the Logistics Working Group, which prepared the plan for procuring and distributing vaccines, injection materials, ITNs, and mebendazole tablets and developed the waste-management plan; and 3) the Social Mobilization Working Group, which developed the communications and social mobilization plan and materials.
International partner organizations under the Measles Initiative * and local agencies, such as the Togolese Red Cross, provided funding and consultants to support campaign planning, implementation, and evaluation. Donor campaign contributions came to nearly USD $6 million, with approximately $5.3 million covering vaccine, mebendazole, ITNs, and supplies; $0.7 million covered operational costs, and these costs did not include MOH inputs, such as staff and vehicles. This translates to approximately USD $6.92 per child.
The government established 565 fixed posts and 628 outreach posts and 146 mobile teams. Each fixed post, serving at least 300 children daily and staffed by two vaccinators and two volunteers, was organized as follows: 1) a volunteer tallied eligible children and distributed campaign cards; 2) a vaccinator administered the measles injection; 3) a second vaccinator administered OPV and mebendazole; and 4) a volunteer provided an ITN for each child and documented services provided on each child's card. Outreach teams included one vaccinator and two volunteers, and mobile teams included one vaccinator and one volunteer. Supervisors used checklists to monitor the quality of services. Thirty-two incinerators for destruction of used injection equipment were rehabilitated to supplement the 140 existing ones; 99% of filled safety boxes were incinerated, and the rest were burned in pits. No severe adverse events were reported.
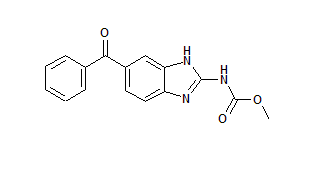
One month after the campaign, a probability-based survey of 2,599 children aged 9-59 months from 142 enumeration areas [dagger] and six districts was conducted. The results indicated that coverage for eligible children was 93.1% (95% confidence interval [CI] = 90.8%-95.4%) for measles vaccine, 93.7% (CI = 91.4%-96.1%) for OPV, 90.8% (CI = 88.1%-93.4%) for an ITN, and 92.7% (CI = 90.3%-95.1%) for mebendazole (Figure).
[FIGURE OMITTED]
Household ownership of ITNs increased from 8.0% (CI = 5.7%-10.2%) to 62.5% (CI = 58.3%-66.6%) before and after the campaign, respectively; however, only 43.5% (CI = 38.4%-48.7%) of children aged <5 years had slept under an ITN on the night before the survey (unpublished data, MOH, 2005).
Editorial Note: The December 2004 National Integrated Child Health campaign in Togo was the first of its kind to distribute free ITNs nationwide in conjunction with a national immunization campaign. To reach Roll Back Malaria (RBM) [section] goals in Africa and achieve national expansion of malaria prevention interventions, the World Health Organization and UNICEF recommend free distribution of ITNs to children and pregnant women (3). Previously, rapid district-level expansion of ITN distribution was achieved during an SIA in one district of Ghana (4) and five districts of Zambia (5). Similar to previous efforts, the campaign in Togo achieved a substantial increase in ITN ownership without compromising delivery of the other child health interventions provided during the campaign, specifically measles and polio vaccination and anti-helminth treatment. Successful national expansion of malaria prevention activities is crucial if control efforts are to succeed in reducing the burden of disease in Africa. The Togo campaign increased household ownership of at least one ITN from 8.0% to 62.5%. Coverage for all four interventions was >90% for eligible children in the campaign, and levels were similar among households at all economic levels (6).
The overall goal of the campaign was to reduce morbidity and mortality in young children in Togo by achieving high coverage for all services provided in the campaign. Community-based trials in Western Kenya demonstrated that two of the key determinants of ITN effectiveness were level of coverage and percentage of persons properly using the bednet each night. When high coverage and appropriate ITN use were achieved in Kenya, a country similar to Togo with intense perennial malaria transmission, both malaria morbidity in children aged <3 years (7) and all-cause mortality in children aged 1-11 months (8) were reduced. Although ITN coverage increased substantially in all regions after the Togo campaign, a coverage survey conducted 1 month after the campaign demonstrated considerable regional variation in ITN use (30.9%72.9%) (unpublished data, MOH, 2005). This result is not unexpected, given that the survey was conducted in the hot and dry low-transmission season and use of ITNs tends to be lower when temperatures are high and mosquito populations are low (9). Nevertheless, the variable usage rate underscores the need for postcampaign efforts in Togo to encourage proper nighttime use of ITNs because these variable rates of use occurred despite precampaign social mobilization efforts by MOH and the Togolese Red Cross. A multidisciplinary evaluation of the impact of the campaign is being conducted, including pre- and postcampaign morbidity studies during the high malaria-transmission season and health-facility-based surveillance.
Although successful, the campaign faced some challenges. First, a unified message was not communicated clearly to the health posts regarding a one-net-per-household or one-net-per-child strategy. Fear of shortages prompted health posts in one region to switch from the MOH-recommended one-net-per-child policy to a one-net-per-household policy.
Second, the age group targeted for the campaign was optimal for a follow-up measles SIA but not for the other health interventions provided. Children aged <9 months are especially vulnerable to malaria, and a recent study in Togo revealed that the burden of malaria-related anemia and parasitemia was substantial in this age group (unpublished data, MOH, 2005). Polio vaccinations also are administered to children aged <9 months; however this age group was not targeted in the campaign. Finally, administration of mebendazole tablets was problematic; children aged <2 years, in particular, had difficulty swallowing or chewing the tablets, and efforts to break up tablets in water and administer directly were time-consuming (10).
Because ITNs are bulky and have intrinsic commercial value, skepticism persists about the ability of African nations to incorporate the distribution of free bednets into immunization campaigns. Nonetheless, the Togo campaign was successful at increasing both ownership and use of ITNs, even with approximately 130,000 ITNs arriving in port only days before the campaign began. Several factors contributed to the success of the campaign, including a committed MOH, strong support from a global partnership and nongovernmental entities such as the Togolese Red Cross, effective coordination of the global partnership's inputs through ICC, and use of an ICC-approved campaign plan to mobilize resources and oversee campaign implementation. The Togolese experience illustrates how using a mass immunization campaign as a platform to deliver other health services can achieve high (>90%) coverage for all interventions and attract donors in resource-poor countries at the national level. The Togo national campaign and the district-level campaigns in Ghana and Zambia have demonstrated that integrating ITN distribution with an immunization campaign enables quick and equitable distribution of ITNs, a key malaria-control tool, to populations at high risk. The Measles Initiative anticipates that as many as 12 African countries will incorporate ITN distribution into their measles immunization campaigns at the national or subnational levels during 2005 and 2006. Nonetheless, continued efforts are needed to encourage use of ITNs.
* The Measles Initiative is a long-term commitment to control measles deaths in Africa by vaccinating 200 million children through both mass and follow-up campaigns in up to 36 sub-Saharan African countries by 2006. Partner agencies leading the initiative are the American Red Cross, Canadian International Development Agency, CDC, United Nations Children's Fund (UNICEF), United Nations Foundation, and the World Health Organization. Other partners contributing to the Togo campaign under MOH guidance included Becton Dickinson; Canadian Red Cross; Church of Jesus Christ of Latter-Day Saints; DHL; Freedom from Hunger; Geneva University; Global Fund for AIDS, Tuberculosis, and Malaria; International Federation of Red Cross and Red Crescent Societies; Joint United Nations Program on HIV/MDS; Nestle; Liverpool School of Tropical Medicine; London School of Hygiene and Tropical Medicine; New Zealand Red Cross Society; Norwegian Agency for Development Cooperation; Norwegian Red Cross; Plan Togo; Population Services International; Reliance Industries; Right to Play; Roll Back Malaria; Rotary International; Sanofi-Synthelab; Togolese Red Cross; Unilever; United Nations Development Program; U.S. Agency for International Development; U.S. Peace Corps; and Vestergaard Frandsen.
[dagger] Sampling areas defined by the Togo Ministry of Statistics for census purposes.
[section] The RBM partnership was launched in 1998 by the World Health Organization, UNICEF, the United Nations Development Programme, and the World Bank to provide a coordinated global approach to fighting malaria. The overall goal of the partnership is to halve malaria mortality by 2010 and again by 2015. Since its launch, the RBM partnership has grown rapidly and now consists of various partners, including malaria-endemic countries, their bilateral and multilateral development partners, nongovernmental and community-based organizations, foundations, and research and academic institutions.
References
(1.) CDC. Progress toward interruption of wild poliovirus transmission-worldwide, January 2004-March 2005. MMWR 2005;54:408-12.
(2.) World Health Organization, United Nations Children's Fund. Prevention and control of schistosomiasis and soil-transmitted helminthiasis. Geneva, Switzerland: World Health Organization; 2004.
(3.) World Health Organization, United Nations Children's Fund. Joint statement: malaria control and immunization: a sound partnership with great potential. Geneva, Switzerland: World Health Organization; 2004.
(4.) Grabowsky M, Nobiya T, Ahun M, et al. Distributing insecticide-treated bednets during measles vaccination: a low-cost means of achieving high and equitable coverage. Bull WHO 2005;83:195-201.
(5.) Grabowsky M, Farrell N, Hawley W, et al. Distribution of insecticide-treated bednets during a measles vaccination campaign achieves high, rapid, and equitable coverage at low cost. Trop Med Int Health 2005; 10: 1-10 (in press).
(6.) Gwatkin D, Johnson K, Wagstaff A, et al. Socio-economic differences in health, nutrition, and population in Togo. Washington, DC: World Bank; 2000. Available at http://wwwl.worldbank.org/prem/poverty/health/data/togo/togo.pdf.
(7.) Hawley W, Phillips-Howard P, ter Kuile E et al. Community-wide effects of permethrin-treated bed nets on child mortality and malaria morbidity in Western Kenya. Am J Trop Med Hyg 2003;68:121-7.
(8.) Eisele T, Lindblade K, Wannemuehler K, et al. Effect of sustained insecticide-treated bed net use on all-cause child mortality in and area of intense perennial malaria transmission in Western Kenya. Am J Trop Med Hyg 2005;73:149-56.
(9.) Alaii J, Hawley W, Kolczak M, et al. Factors affecting use of permethrin-treated bed nets during a randomized controlled trial in Western Kenya. Am J Trop Med Hyg 2003;68:137-41.
(10.) World Health Organization. Report of the Third Global Meeting of the Partners for Parasite Control. Deworming for health and development. Geneva, Switzerland: World Health Organization; 2005. Available at http://whqlibdoc.who.int/hq/2005/who_cds_cpe_pvc_2005.14.pdf.
Reported by: V Takpa, MD, K Morgah, MD, Togo Ministry of Health; P Gbedonou, MD, Togo Country Office, World Health Organization, Lome, Togo. Regional Office for Africa, World Health Organization, Harare, Zimbabwe. Div of Parasitic Diseases, National Center for Infectious Diseases; Global Immunization Div, National Immunization Program; M Eliades, MD, EIS Officer, CDC.
COPYRIGHT 2005 U.S. Government Printing Office
COPYRIGHT 2005 Gale Group