Over the last 15 yr, the World Health Assembly has passed several resolutions calling for the control, elimination or even eradication of diseases caused by worms. These include lymphatic filariasis, the soil-transmitted helminthiases, schistosomiasis, dracunculiasis and onchocerciasis. But as Lancet said recently, 'worm control rarely makes the headlines - worms are just not sexy'1.
Why are worm infections so neglected? Certainly not because they are rare. We recently estimated that Ascaris lumbricoides (or the common roundworm) infects 1.2 billion individuals worldwide; Trichuris trichiura infects about 800 million; and the hookworms (Necator americanus and Ancylostoma duodenale) about 750 million2. The estimates for infections in India, based on extensive surveys carried out by the National Institute for Communicable Diseases, Delhi were 140, 73 and 71 millions, respectively. Global estimates for lymphatic filarial infections (largely caused by Wuchereria bancrofti and Brugia malayi) are about 120 million, and India alone was estimated to account for about 38 per cent of the total disease burden worldwide3. Perhaps their very ubiquity makes people in endemic areas assume that worms are an inevitable part of life.
There are other reasons that could explain why worm infections are so often ignored. The mechanisms of disease transmission are such that they are confined to developing countries with tropical and sub-tropical climates. The same mechanisms ensure that infections are most prevalent amongst the poorest people in these countries. For example, transmission of roundworm, whipworm and hookworm requires a warm wet environment to ensure survival of eggs or larvae in soil that is contaminated with human faeces. Filarial worms are mostly transmitted by Culex mosquitoes that breed in stagnant pools of water contaminated with organic matter. Such conditions inevitably exist in poor urban and rural communities in developing countries.
Worm infections are rarely fatal. Severe morbidity (e.g., acute intestinal obstruction due to roundworm, severe anaemia in hookworm infection, gross elephantiasis or hydrocoele due to lymphatic filariasis) is seen in only a small proportion of those infected; the greater proportion remains asymptomatic or suffers from only mild disease. Parasitic worms have evolved with their human hosts over thousands of years, and as successful parasites, do not kill their hosts. They cause chronic infections, which seem to evoke little protective immunity; re-infection is very common in endemic areas. However, some individuals build up very heavy worm burdens with time, and these intensely infected persons are the ones that suffer the severe consequences of infection.
Disentangling the milder effects of worm infections from all the other factors that cause ill health among the poor in developing countries has been difficult. Take roundworm, for example, they are large worms (growing up to 30-40 cm in size), and their natural habitat is the small intestine, where most nutrients are digested and absorbed. It is therefore logical to assume that roundworms would cause malnutrition in children, who have the highest age prevalence and intensity of infection. However, infected children are usually from poor families that do not have enough to eat, and suffer from many other infections as well. Thus, indisputable evidence that roundworms cause growth retardation came only in the 1990s, when the availability of highly effective anthelmintics made it possible to compare the growth of large numbers of children before and after elimination of infection4. It is now estimated that for children aged 5-14 yr in low-income countries, intestinal worms account for 11-12 per cent of the total disease burden (their single largest contributor to disease), and are linked to the loss of 20 per cent of disability adjusted life-years1.
Similarly, we now have evidence that anaemia, vitamin A deficiency, poor intellectual development, impaired cognitive function are all sequelae of chronic infection with soil-transmitted intestinal helminths4. Hookworm infections in particular, aggravate maternal anaemia, and reduce labour productivity of adults5. Lymphatic filarial infections, even those that seem asymptomatic, are invariably accompanied by some degree of damage to the lymphatics6. Even though these are not dramatic, life-threatening consequences, the sheer numbers of people affected by even mild consequences, make it imperative that transmission is controlled.
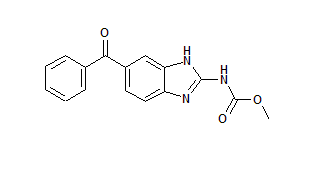
Now, at the beginning of a new century and a new millenium, we have the means of controlling these infections. Highly effective anthelmintics lie at the core of control programmes directed against four of the five groups of helminth infections mentioned at the beginning of this article (the exception being dracunculiasis). The benzimidazoles, mebendazole and albendazole, have a broad spectrum of activity against all the soil-transmitted helminths. Albendazole is also effective in suppressing microfilaraemia in lymphatic filariasis, and is recommended for use with diethylcarbamazine (DEC) or ivermectin for filariasis control. Ivermectin was widely used in the very successful Onchocerciasis Control Programme in West Africa. Praziquantel is the drug of choice for schistosomiasis control.
Using drugs that simply kill off the worms in the human host, but do not prevent re-infection may seem futile when re-infection is almost inevitable in endemic areas. But treatment can be repeated because we know that these drugs are safe, some of them even in pregnancy7. The safety margin is so high that they can be administered without first confirming infection status, which is a particular advantage, because laboratory diagnosis costs much more than drug treatment. Thus, anthelmintics are not just drugs for the treatment of infected individuals. When a large majority of an endemic community takes them at the same time, anthelmintics become very good tools for controlling the spread of disease. The efficacy of single-dose regimens further adds to their attractiveness for mass chemotherapy. There are no major concerns regarding the development of drug resistance because all these worms have an adult life span of one or more years, unlike bacteria or protozoa, which have a generation time of only a few hours or days.
The WHO now recommends twice- or thrice-yearly treatments in areas with a very high (above 70%) prevalence of soil-transmitted helminth infections, or annual treatment if prevalence is over 50 per cent. Because school aged children have the highest prevalence and the heaviest infections (thus contributing most to environmental contamination), school-based control programmes can be very cost-effective when resources are limited8. The Global Programme for the Elimination of Lymphatic Filariasis recommends the annual treatment of entire endemic populations at risk of filarial infection, with a combination of albendazole and DEC or ivermectin. The combination of DEC and albendazole is recommended by WHO for mass drug administration for elimination of lymphatic filariasis in its South East Asia region. It is hoped that five rounds of such mass drug administration programmes will eliminate the disease as a public health problem, and perhaps even interrupt transmission9.
Affordability is another compelling reason why developing countries like India should not overlook this opportunity to improve the health of its poorest citizens. Both mebendazole and albendazole only cost about US$0.02 per treatment for a school-aged child1, while the per capita cost of one round of mass drug administration for lymphatic filariasis has been calculated to be about US$0.05 in India10. The drugs are also heat stable, require no cold chain for delivery, and have a shelf life of up to four years, allowing bulk purchase or donation. With its flourishing pharmaceutical industry, India has the capacity to produce all its drug requirements locally, without encountering the problems of patents.
The benefits of controlling these infections go beyond simply eliminating unwanted worms. Deworming in childhood leads to improvements in intellectual development that will in turn impact on income during adulthood. It has been calculated that an investment of as little as US$3.50 per child on helminth control translates to an extra year of schooling gained. School-based deworming programmes improve school enrollment rates for girls, along with drop-out and retention rates. Adding albendazole to micronutrient supplements in pregnancy reduces the incidence of severe anaemia, and improves birthweight and infant survival in hookworm endemic areas'. In the case of lymphatic filariasis, preventing chronic disease through controlling transmission has been calculated to save an average of 58.2 working days per year per infected person10. When treatment costs are added to the wages earned on these working days, the total annual economic saving is US$ 40.81 per year per person, with a lifetime saving of US$449.1. All this in return for US$ 8.40, the total estimated cost of preventing one case of chronic disease through a mass drug administration programme. The question that we need to ask ourselves is not whether we can afford worm control programmes, but whether we can afford not to control these infections.
Health care professionals have two major roles. Firstly, policy-makers and administrators must actively push for control programmes wherever these infections are endemic. National Ministries of Health should take steps to develop a national plan of action for control and prevention of soil-transmitted helminths. The first national workshop was held in New Delhi, India in January 2004. Once such programmes are in place, all those with direct patient contact must encourage members of the public to take the anthelmintics when offered, because like immunization programmes, their ultimate success depends on the extent of coverage.
References
1. Thinking beyond deworming. Lancet 2004; 364 : 1993-4.
2. de Silva N, Brooker S, Hotez P, Montresor A, Engels D, Savioli L. Soil-transmitted helminth infections: updating the global picture. Trend Parasitol 2003; 19 : 547-51.
3. Michael E, Bundy DAP, Grenfell BT. Re-assessing the global prevalence and distribution of lymphatic filariasis. Parasitology 1996; 112 : 409-28.
4. Stephenson LS, Latham MC, Ottesen EA. Malnutrition and parasitic helminth infections. Parasitology 2000; 121 (Suppl): S23-8.
5. Hotez PJ, Brooker S, Bethony JM, Bottazzi ME, Loukas A, Xiao SH. Current concepts: hookworm infection. N Engl J Med 2004; 351 : 799-807.
6. Lammie PJ, Cuenco KT, Punkosdy GA. The pathogenesis of filarial lymphedema: is it the worm or is it the host? Ann NY Acad Sci 2002; 979 : 131-42.
7. de Silva NR, Sirisena JLGJ, Gunasekera DPS, Ismail MM, de Silva HJ. Effect of mebendazole therapy during pregnancy on birth outcome. Lancet 1999; 353 : 1145-9.
8. Prevention and control of schistosomiasis and soil-transmitted helminthiasis. Report of a WHO Expert Committee. WHO Tech Rep Ser no.912. Geneva: World Health Organization; 2002.
9. Molyneux D. Lymphatic filariasis (Elephantiasis) elimination: a public health success and development opportunity. Filaria J 2003; 2:13.
10. Ramaiah KD, Das PK. Mass drug administration to eliminate lymphatic filariasis in India. Trends Parasitol 2004; 20: 499-502.
Nilanthi de Suva
Professor of Parasitology
Faculty of Medicine
University of Kelaniya
P.O. Box 6, Ragama, Sri Lanka
e-mail: nrdes@sltnet.1k
Copyright Indian Council of Medical Research Jul 2005
Provided by ProQuest Information and Learning Company. All rights Reserved