Primary dysmenorrhea, which is defined as painful menses in women with normal pelvic anatomy, usually begins during adolescence. It is characterized by crampy pelvic pain beginning shortly before or at the onset of menses and lasting one to three days. Dysmenorrhea also may be secondary to pelvic organ pathology.
The prevalence of dysmenorrhea is highest in adolescent women, with estimates ranging from 20 to 90 percent, depending on the measurement method used. (1-3) About 15 percent of adolescent girls report severe dysmenorrhea, (1,4) and it is the leading cause of recurrent short-term school absenteeism in adolescent girls in the United States. (2,5) A longitudinal study (6) of a representative cohort of Swedish women found a prevalence of dysmenorrhea of 90 percent in women 19 years of age and 67 percent in women 24 years of age. Ten percent of the 24-year-olds reported pain that interfered with daily function. Most adolescents self-medicate with over-the-counter medicines, and few consult a physician about dysmenorrhea. (1-3)
Pathogenesis
Dysmenorrhea is thought to be caused by the release of prostaglandins in the menstrual fluid, which causes uterine contractions and pain. Vasopressin also may play a role by pain. increasing uterine contractility and causing ischemic pain as a result of vasoconstriction. Elevated vasopressin levels have been reported in women with primary dysmenorrhea.
The relationship between endometriosis and dysmenorrhea is not clear. Endometriosis may be asymptomatic, or it may be associated with pelvic pain that is not limited to the menstrual period and the low anterior pelvis. In one study (7) of women undergoing elective sterilization, no difference was found in the prevalence of dysmenorrhea in women with and women without an incidental finding of endometriosis. However, an observational study (8) of women undergoing laparoscopy for infertility supported a relationship between dysmenorrhea and the severity of endometriosis.
Risk Factors
Young age and nulliparity are associated with dysmenorrhea. (4,9) However, one longitudinal study (6) found that age was not a risk factor after controlling for parity and other factors, and that dysmenorrhea improved after childbirth. Heavy menstrual flow is associated with dysmenorrhea. (4,5,9) Table 1 lists risk factors for dysmenorrhea.
Behavioral risk factors are of interest because of the potential to intervene. Several observational studies (6,10,11) have found an association between smoking and dysmenorrhea. In women 14 to 20 years of age, attempts to lose weight are associated with increased menstrual pain independent of body mass index. (12) However, the evidence of an association between overweight and dysmenorrhea is inconsistent. (4,6,10) Other behaviors such as physical activity and alcohol consumption have not been associated consistently with dysmenorrhea. (10,11)
Mental health problems are another potentially modifiable risk factor. Depression, anxiety, and disruption of social support networks have been associated with menstrual pain. (13) An association between poor self-rated overall health and dysmenorrhea has been noted, (9) but socioeconomic status is not associated consistently with dysmenorrhea. (5,9) Although there has been concern that tubal sterilization may be a risk factor for dysmenorrhea, a cross-sectional study (14) found no difference in menstrual pain in women with and women without tubal sterilization.
Diagnosis
In most patients who present with menstrual pain, empiric therapy may be prescribed with the presumptive diagnosis of primary dysmenorrhea, based on a typical history of low anterior pelvic pain beginning in adolescence and associated specifically with menstrual periods. A history that is inconsistent and/or physical findings of a pelvic mass, abnormal vaginal discharge, or pelvic tenderness that is not limited to the time of the menstrual period suggest a diagnosis of secondary dysmenorrhea. It is appropriate to perform only an abdominal examination in young adolescents with a typical history who have never been sexually active. A pelvic examination should be performed in females who have been sexually active to screen for sexually transmitted diseases such as chlamydial infection.
When the history and physical examination suggest other pelvic pathology, the evaluation should follow accordingly, usually with pelvic ultrasonography as the initial diagnostic test to rule out anatomic abnormalities such as mass lesions. In patients with severe dysmenorrhea that is unresponsive to initial treatment, ultrasonography is useful to detect ovarian cysts and endometriomas. (15) It also has reasonably good ability to detect advanced stage 3 or 4 endometriosis; its concordance with surgical staging is 84 percent. 16 Sonovaginography (i.e., transvaginal ultrasonography with saline infusion of the uterus) appears to be better than transvaginal sonography alone in diagnosing rectovaginal endometriosis. (17) Magnetic resonance imaging is limited in its ability to diagnose endometriosis (sensitivity, 69 percent; specificity, 75 percent). (18) The reference standard test for diagnosis and staging of endometriosis is laparoscopy or laparotomy with biopsy. It should be considered when first-line therapies are ineffective and dysmenorrhea causes functional impairment.
Therapy
Table 2 (19-32) lists therapies for dysmenorrhea and the strength of evidence to support their efficacy. Many of the standard treatments have not been well studied. The recommendations reflect a balance between the available evidence and an assessment of benefit, harm, and cost. Table 3 provides dosing and cost information for prescription drugs used in the treatment of dysmenorrhea.
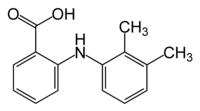
NSAIDS
Nonsteroidal anti-inflammatory drugs (NSAIDs) are the best-established initial therapy for dysmenorrhea. (19) They have a direct analgesic effect through inhibition of prostaglandin synthesis, and they decrease the volume of menstrual flow. These effects probably are common to all NSAIDs. Two meta-analyses (33,34) of randomized controlled trials (RCTs) of NSAIDs and acetaminophen found that all of the NSAIDs studied (i.e., ibuprofen [Motrin], naproxen [Naprosyn], mefenamic acid [Ponstel], and aspirin) were effective in treating women with dysmenorrhea, and all of the NSAIDs were more effective than acetaminophen. (19) Small studies (22,23) of cyclooxygenase-2 inhibitors have shown efficacy similar to that of NSAIDs in the treatment of dysmenorrhea. NSAIDs may be most effective when therapy is started before the onset of menstrual pain and flow, although therapy need not be continued after the end of the flow.
ORAL CONTRACEPTIVE PILLS
Treatment of dysmenorrhea is a well-accepted off-label use for oral contraceptive pills (OCPs). The proposed mechanism of action is reduced prostaglandin release during menstruation. Consistent observational data support a beneficial effect from oral contraceptives in the treatment of dysmenorrhea, and in one exploratory RCT (35) of women who took desogestrel-containing OCPs, these women had less containing pain during menses than women who received placebo. An observational study (36) of dysmenorrhea severity in women who used different forms of contraception showed lower mean scores in users of monophasic formulations compared with triphasics. However, a Cochrane review (37) found insufficient evidence from RCTs to draw conclusions about the effectiveness of OCPs in treating dysmenorrhea.
OTHER HORMONAL METHODS
Several other off-label methods exist for treating dysmenorrhea with hormonal contraceptives. Most women who receive depo-medroxyprogesterone acetate (Depo-Provera) are amenorrheic within the first year of use. Similarly, extended-cycle use of OCPs (i.e., usually taking OCPs for 12 weeks followed by one week off) leads to less-frequent menstrual periods. In a retrospective review, (38) 21 percent of women who chose extended-cycle regimens did so primarily for treatment of dysmenorrhea. Observational data (39) from users of the levonorgestrel intrauterine device (Mirena) showed a decrease in prevalence of dysmenorrhea from 60 percent before use of the device to 29 percent after 36 months of use.
A novel treatment approach is intravaginal administration of standard OCPs (i.e., 30 mcg of ethinyl estradiol and 150 mg of levonorgestrel daily); an RCT (27) of 150 women found fewer systemic side effects and less dysmenorrhea with the intravaginal approach (21 percent with intravaginal use versus 44 percent with standard oral administration; number needed to treat, 4; P < .001). Contraceptive patches appear to be less effective than OCPs taken orally in treating women with dysmenorrhea. (40)
OTHER PHARMACOLOGIC TREATMENTS
Several medications that induce uterine relaxation have been proposed for treatment of dysmenorrhea. In one RCT, (41) it was found that glyceryl trinitrate is less effective than diclofenac and is associated with a high incidence of headache. Early uncontrolled pilot studies (28,30) of oral nifedipine and intravenous terbutaline showed promise, but further study on these drugs is needed.
Treatment to suppress the menstrual cycle with danazol (Danocrine) or leuprolide acetate (Lupron) may be considered, rarely, in refractory cases. These are expensive therapies with significant side effects; they usually are reserved for treatment of conditions other than primary dysmenorrhea, such as endometriosis and chronic pelvic pain that is not limited to the time of the menstrual period.
LIFESTYLE MODIFICATION
Few studies have examined the effect of lifestyle-modification interventions in the management of dysmenorrhea. One cross-over study (26) of a low-fat vegetarian diet versus placebo pill showed decreased duration and intensity of dysmenorrhea in women in the intervention group. Although some studies have reported a benefit with exercise, the effect is questionable because participants were not blinded to the study hypothesis. (19) Smoking cessation has not been studied as an intervention to manage dysmenorrhea.
Complementary and Alternative Medicines
SUPPLEMENTS
Thiamine at a dosage of 100 mg daily was found to be effective in treating dysmenorrhea in a double-blind RCT of more than 500 East Indian women aged 12 to 21 years with moderate to severe symptoms. (19) It is unclear whether thiamine would be effective in U.S. women, whose diet may be quite different from that of Indian women. A single RCT of vitamin E found that 2,500 IU taken daily for five days starting two days before menstruation was more effective than placebo in treating dysmenorrhea. (19) A small RCT24 of omega-3 polyunsaturated fatty acids found that 2 g daily of a fish oil supplement significantly reduced pain compared with placebo. High intake of fish n-3 fatty acid also was associated with less average symptom severity in an observational study of Danish women. (42)
HERBAL REMEDIES
The Japanese herbal remedy toki-shakuyakusan (TSS) has been shown in an RCT to be better than placebo in the treatment of women with dysmenorrhea. (19) Because this product is not regulated, the ingredients and effectiveness may vary among formulations. It does not appear to suppress fertility or ovulation. There are insufficient data to evaluate other herbal products. (19)
PHYSICAL TREATMENTS
Limited evidence from RCTs suggests that acupuncture and acupressure are effective in treating dysmenorrhea. In a study (20) study of acupuncture versus sham acupuncture, 91 percent of patients in the treatment group had pain relief compared with 36 percent of control patients. Patients in the treatment group had a 41 percent reduction in use of pain medication, while no difference was noted in control patients. (20) A study (21) study of acupressure at a point on the hand found pain relief similar to that in patients who took ibuprofen and better than that in patients who received sham acupressure. A study (43) study of acupressure underwear was inconclusive because of lack of blinding. of blinding.
A single small study (44) study of transcutaneous electric nerve stimulation (TENS) suggested that TENS is more effective in treating dysmenorrhea than a sham procedure, with 42 percent of women reporting good to excellent pain relief with TENS compared with 3 percent of control patients. However, a systematic review (45) review found insufficient evidence to determine if TENS is effective. In a study (46) study of a topical heated patch compared with low-dose ibuprofen (i.e., 400 mg three times daily) and placebo, the heated patch was as effective as ibuprofen.
A well-designed study (31) study of spinal manipulative therapy versus a sham procedure showed similar pain relief in both groups. In addition, a systematic review (32) of spinal manipulation in the treatment of dysmenorrhea concluded that there is no evidence to suggest effectiveness.
Surgical Therapies
In rare instances, a surgical approach may be considered for women with severe, refractory dysmenorrhea. Refractory dysmenorrhea is an accepted indication for hysterectomy. Laparoscopic uterine nerve ablation (LUNA) and presacral neurectomy also have been used in refractory cases. Observational data (47) show show that at one year after the procedure, pain relief persisted in 82 percent of women having presacral neurectomy and in only 51 percent having LUNA. Information about long-term outcomes is relatively lacking. A Cochrane meta-analysis (29) of surgical interruption of pelvic nerve pathways as a treatment for dysmenorrhea concluded that evidence was insufficient to recommend the procedure, regardless of the cause of the dysmenorrhea.
Approach to the Patient
NSAIDs are the initial therapy of choice in patients with presumptive primary dysmenorrhea. Because all NSAIDs are equal in efficacy, agent selection should be guided by cost, convenience, and patient preference, with ibuprofen or naproxen being a good choice for most patients. If hormonal contraception is desired, monophasic OCPs and depo-medroxyprogesterone acetate also may be considered. If relief is insufficient, the physician may consider prolonged-cycle OCP use or intravaginal use of OCPs.
In women who do not desire hormonal contraception, topical heat; TSS; thiamine, vitamin E, or fish oil supplements; a low-fat vegetarian diet; and acupressure are relatively simple and inexpensive alternatives that can be used alone or in combination. If dysmenorrhea is not controlled with any of these approaches, pelvic ultrasonography should be performed and referral for laparoscopy should be considered to rule out secondary causes of dysmenorrhea. (48,49) In severe refractory primary dysmenorrhea, additional safe alternatives for women who want to conceive are (in order of clinical preference) TENS, acupuncture, nifedipine (Procardia), and terbutaline (Bricanyl). Otherwise, danazol or leuprolide may be considered and, rarely, hysterectomy.
Therapies on the Horizon
Several of the therapeutic approaches discussed in this article deserve further study before we can say definitively whether they are effective. Two options may become available in the near future: (1) a vasopressin-receptor antagonist is being tested. Because vasopressin appears to be involved in the pathogenesis of dysmenorrhea, vasopressin-receptor antagonists are theoretically useful. However, studies (50-53) to date have not shown consistent evidence of efficacy. And (2) a frameless levonorgestrel IUD has been introduced in Europe, where it is being used in the management of primary and secondary dysmenorrhea. (54) The frameless device decreases menstrual flow and provides contraceptive efficacy similar to that of currently available IUDs.
REFERENCES
(1.) Davis AR, Westhoff CL. Primary dysmenorrhea in adolescent girls and treatment with oral contraceptives. J Pediatr Adolesc Gynecol 2001;14:3-8.
(2.) Banikarim C, Chacko MR, Kelder SH. Prevalence and impact of dysmenorrhea on Hispanic female adolescents. Arch Pediatr Adolesc Med 2000;154:1226-9.
(3.) Strinic T, Bukovic D, Pavelic L, Fajdic J, Herman I, Stipic I, et al. Anthropological and clinical characteristics in adolescent women with dysmenorrhea. Coll Antropol 2003;27:707-11.
(4.) Andersch B, Milsom I. An epidemiologic study of young women with dysmenorrhea. Am J Obstet Gynecol 1982;144:655-60.
(5.) Klein JR, Litt IF. Epidemiology of adolescent dysmenorrhea. Pediatrics 1981;68:661-4.
(6.) Sundell G, Milsom I, Andersch B. Factors influencing the prevalence and severity of dysmenorrhoea in young women. Br J Obstet Gynaecol 1990;97:588-94.
(7.) Moen MH, Stokstad T. A long-term follow-up study of women with asymptomatic endometriosis diagnosed incidentally at sterilization. Fertil Steril 2002;78:773-6.
(8.) Momoeda M, Taketani Y, Terakawa N, Hoshiai H, Tanaka K, Tsutsumi O, et al. Is endometriosis really associated with pain? Gynecol Obstet Invest 2002;54(suppl 1):18-21.
(9.) Teperi J, Rimpela M. Menstrual pain, health and behaviour in girls. Soc Sci Med 1989;29:163-9.
(10.) Harlow SD, Park M. A longitudinal study of risk factors for the occurrence, duration and severity of menstrual cramps in a cohort of college women [published erratum appears in Br J Obstet Gynaecol 1997;104:386]. Br J Obstet Gynaecol 1996;103:1134-42.
(11.) Parazzini F, Tozzi L, Mezzopane R, Luchini L, Marchini M, Fedele L. Cigarette smoking, alcohol consumption, and risk of primary dysmenorrhea. Epidemiology 1994;5:469-72.
(12.) Montero P, Bernis C, Fernandez V, Castro S. Influence of body mass index and slimming habits on menstrual pain and cycle irregularity. J Biosoc Sci 1996;28:315-23.
(13.) Alonso C, Coe CL. Disruptions of social relationships accentuate the association between emotional distress and menstrual pain in young women. Health Psychol 2001;20:411-6.
(14.) Harlow BL, Missmer SA, Cramer DW, Barbieri RL. Does tubal sterilization influence the subsequent risk of menorrhagia or dysmenorrhea? Fertil Steril 2002;77:754-60.
(15.) Moore J, Copley S, Morris J, Lindsell D, Golding S, Kennedy S. A systematic review of the accuracy of ultrasound in the diagnosis of endometriosis. Ultrasound Obstet Gynecol 2002;20:630-4.
(16.) Exacoustos C, Zupi E, Carusotti C, Rinaldo D, Marconi D, Lanzi G, et al. Staging of pelvic endometriosis: role of sonographic appearance in determining extension of disease and modulating surgical approach. J Am Assoc Gynecol Laparosc 2003;10:378-82.
(17.) Dessole S, Farina M, Rubattu G, Cosmi E, Ambrosini G, Nardelli GB. Sonovaginography is a new technique for assessing rectovaginal endometriosis. Fertil Steril 2003;79:1023-7.
(18.) Stratton P, Winkel C, Premkumar A, Chow C, Wilson J, Hearns-Stokes R, et al. Diagnostic accuracy of laparoscopy, magnetic resonance imaging, and histopathologic examination for the detection of endometriosis. Fertil Steril 2003;79:1078-85.
(19.) Proctor M, Farquhar C. Dysmenorrhoea. Clin Evid 2002;(7):1639-53.
(20.) Helms JM. Acupuncture for the management of primary dysmenorrhea. Obstet Gynecol 1987;69:51-6.
(21.) Pouresmail Z, Ibrahimzadeh R. Effects of acupressure and ibuprofen on the severity of primary dysmenorrhea. J Tradit Chin Med 2002;22:205-10.
(22.) Barnard ND, Scialli AR, Hurlock D, Bertron P. Diet and sex-hormone binding globulin, dysmenorrhea, and premenstrual symptoms. Obstet Gynecol 2000;95:245-50.
(23.) Daniels SE, Talwalker S, Torri S, Snabes MC, Recker DP, Verburg KM. Valdecoxib, a cyclooxygenase-2-specific inhibitor, is effective in treating primary dysmenorrhea. Obstet Gynecol 2002;100:350-8.
(24.) Harel Z, Biro FM, Kottenhahn RK, Rosenthal SL. Supplementation with omega-3 polyunsaturated fatty acids in the management of dysmenorrhea in adolescents. Am J Obstet Gynecol 1996;174:1335-8.
(25.) Jensen JT. Noncontraceptive applications of the levonorgestrel intrauterine system. Curr Womens Health Rep 2002;2:417-22.
(26.) Malmstrom K, Kotey P, Cichanowitz N, Daniels S, Desjardins PJ. Analgesic efficacy of etoricoxib in primary dysmenorrhea: results of a randomized, controlled trial. Gynecol Obstet Invest 2003;56:65-9.
(27.) Ziaei S, Rajaei L, Faghihzadeh S, Lamyian M. Comparative study and evaluation of side effects of low-dose contraceptive pills administered by the oral and vaginal route. Contraception 2002;65:329-31.
(28.) Andersson KE, Ulmsten U. Effects of nifedipine on myometrial activity and lower abdominal pain in women with primary dysmenorrhoea. Br J Obstet Gynaecol 1978;85:142-8.
(29.) Proctor ML, Farquhar CM, Sinclair OJ, Johnson NP. Surgical interruption of pelvic nerve pathways for primary and secondary dysmenorrhoea. Cochrane Database Syst Rev 2004(3):CD001896.
(30.) Akerlund M, Andersson KE, Ingemarsson I. Effects of terbutaline on myometrial activity, uterine blood flow, and lower abdominal pain in women with primary dysmenorrhoea. Br J Obstet Gynaecol 1976;83:673-8.
(31.) Hondras MA, Long CR, Brennan PC. Spinal manipulative therapy versus a low force mimic maneuver for women with primary dysmenorrhea: a randomized, observer-blinded, clinical trial. Pain 1999;81:105-14.
(32.) Proctor M, Hing W, Johnson T, Murphy P. Spinal manipulation for primary and secondary dysmenorrhoea. Cochrane Database Syst Rev 2004(3):CD002119.
(33.) Zhang WY, Li Wan Po A. Efficacy of minor analgesics in primary dysmenorrhoea: a systematic review. Br J Obstet Gynaecol 1998;105:780-9.
(34.) Weaver AL. Rofecoxib: clinical pharmacology and clinical experience. Clin Ther 2001;23:1323-38.
(35.) Hendrix SL, Alexander NJ. Primary dysmenorrhea treatment with a desogestrel-containing low-dose oral contraceptive. Contraception 2002;66:393-9.
(36.) Milsom I, Sundell G, Andersch B. The influence of different combined oral contraceptives on the prevalence and severity of dysmenorrhea. Contraception 1990;42:497506.
(37.) Proctor ML, Roberts H, Farquhar CM. Combined oral contraceptive pill (OCP) as treatment for primary dysmenorrhoea. Cochrane Database Syst Rev 2001(3): CD002120.
(38.) Sulak PJ, Kuehl TJ, Ortiz M, Shull BL. Acceptance of altering the standard 21-day/7-day oral contraceptive regimen to delay menses and reduce hormone withdrawal symptoms. Am J Obstet Gynecol 2002;186:1142-9.
(39.) Baldaszti E, Wimmer-Puchinger B, Loschke K. Acceptability of the long-term contraceptive levonorgestrelreleasing intrauterine system (Mirena): a 3-year followup study. Contraception 2003;67:87-91.
(40.) Audet MC, Moreau M, Koltun WD, Waldbaum AS, Shangold G, Fisher AC, et al. Evaluation of contraceptive efficacy and cycle control of a transdermal contraceptive patch vs an oral contraceptive: a randomized controlled trial. JAMA 2001;285:2347-54.
(41.) Facchinetti F, Sgarbi L, Piccinini F, Volpe A. A comparison of glyceryl trinitrate with diclofenac for the treatment of primary dysmenorrhea: an open, randomized, cross-over trial. Gynecol Endocrino 2002;16:39-43.
(42.) Deutch B. Menstrual pain in Danish women correlated with low n-3 polyunsaturated fatty acid intake. Eur J Clin Nutr 1995;49:508-16.
(43.) Taylor D, Miaskowski C, Kohn J. A randomized clinical trial of the effectiveness of an acupressure device (Relief Brief) for managing symptoms of dysmenorrhea. J Altern Complement Med 2002;8:357-70.
(44.) Dawood MY, Ramos J. Transcutaneous electrical nerve stimulation (TENS) for the treatment of primary dysmenorrhea: a randomized crossover comparison with placebo TENS and ibuprofen. Obstet Gynecol 1990;75:656-60.
(45.) Proctor ML, Smith CA, Farquhar CM, Stones RW. Transcutaneous electrical nerve stimulation and acupuncture for primary dysmenorrhoea. Cochrane Database Syst Rev 2002;(3):CD002123.
(46.) Akin MD, Weingand KW, Hengehold DA, Goodale MB, Hinkle RT, Smith RP. Continuous low-level topical heat in the treatment of dysmenorrhea. Obstet Gynecol 2001;97:343-9.
(47.) Chen FP, Chang SD, Chu KK, Soong YK. Comparison of laparoscopic presacral neurectomy and laparoscopic uterine nerve ablation for primary dysmenorrhea. J Reprod Med 1996;41:463-6.
(48.) Eskenazi B, Warner M, Bonsignore L, Olive D, Samuels S, Vercellini P. Validation study of nonsurgical diagnosis of endometriosis. Fertil Steril 2001;76:929-35.
(49.) Frackiewicz EJ. Endometriosis: an overview of the disease and its treatment. J Am Pharm Assoc (Wash) 2000;40:645-57.
(50.) Akerlund M. Can primary dysmenorrhea be alleviated by a vasopressin antagonist? Results of a pilot study. Acta Obstet Gynecol Scand 1987;66:459-61.
(51.) Brouard R, Bossmar T, Fournie-Lloret D, Chassard D, Akerlund M. Effect of SR49059, and orally active V1a vasopressin receptor antagonist, in the prevention of dysmenorrhoea. BJOG 2000;107:614-9.
(52.) Paranjape SB, Thibonnier M. Development and therapeutic indications of orally-active non-peptide vasopressin receptor antagonists. Expert Opin Investig Drugs 2001;10:825-34.
(53.) Valentin L, Sladkevicius P, Kindahl H, Broeders A, Marsal K, Melin P. Effects of a vasopressin antagonist on women with dysmenorrhea. Gynecol Obstet Invest 2000;50:170-7.
(54.) Wildemeersch D, Schacht E, Wildemeersch P. Treatment of primary and secondary dysmenorrhea with a novel 'frameless' intrauterine levonorgestrel-releasing drug delivery system: a pilot study. Eur J Contracept Reprod Health Care 2001;6:192-8.
LINDA FRENCH, M.D., is associate professor and associate chair for clinical services in the Department of Family Practice at Michigan State University College of Human Medicine, East Lansing. Dr. French received her medical degree from Austral University Faculty of Medicine in Valdivia, Chile, and completed a family medicine residency at Oakwood Hospital and Medical Center in Dearborn, Mich. She also completed primary care faculty development and research training fellowships at Michigan State University.
Address correspondence to Linda French, M.D., Department of Family Practice, Address correspondence to Linda French, M.D., Department of Family Practice, College of Human Medicine, Michigan State University, B101 Clinical Center, East Lansing, MI 48824 (e-mail: Linda.French@hi.msu.edu). Reprints are not available from the author. from the author.
* Patient information: A handout on dysmenorrhea, written by the author of this article, is provided on page 292. EB CME This clinical content conforms to AAFP criteria for evidence-based continuing medical education (EB CME). EB CME is clinical content presented with practice recommendations supported by evidence that has been systematically reviewed by an AAFP-approved source.
The author indicates that she does not have any conflicts of interest. Sources of funding: none reported.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group