Study objectives: Methadone, a long-acting [micro]-opioid agonist, is an effective treatment for heroin addiction. Our previous data show that 6 of 10 methadone maintenance treatment (MMT) patients had central sleep apnea (CSA). This study aims to confirm these results and to investigate the pathogenesis of the CSA.
Methods: Twenty-five male and 25 female MMT patients and 20 age-, sex-, and body mass index (BMI)-matched normal subjects were tested with polysomnography, blood toxicology, and ventilatory responses to hypoxia and hypereapnia. Resting cardiorespiratory tests were performed in the MMT group
Results: MMT patients and normal subjects were 35 [+ or -] 9 years old (mean [+ or -] SD), and BMI values were 27 [+ or -] 6 kg/[m.sup.2] and 27 [+ or -] 5 kg/[m.sup.2], respectively. Thirty percent of MMT patients had a central apnea index (CAI) > 5, and 20% had a CAI > 10. All normal subjects had a CAI < 1, and no difference was found in obstructive apnea-hypopnea index between the two groups. Methadone blood concentration was the only significant variable (t = 2.33, p = 0.025) associated with CAI and explains 12% of the variance. Awake PaC[O.sub.2], antidepressant use, reduced ventilatory response to hypercapnia, and widened awake alveolar-arterial oxygen pressure gradient together explain a further 17% of the CAI variance.
Conclusions: Thirty percent of stable MMT patients have CSA, a minority of which can be explained by blood methadone concentration. Other physiologic variables may also play a role in the pathogenesis of CSA in MMT patients, and further research is indicated in this area.
Key words: central sleep apnea; hypercapnic ventilatory response; hypoxic ventilatory response; methadone
Abbreviations: ABG = arterial blood gas; AHI = apnea/hypopnea index; BMI = body mass index; CAI = central apnea index; CSA = central sleep apnea. ESS = Epworth sleepiness scale; FAC[O.sub.2] = expired fractional concentration of carbon dioxide; HCVR = hypercapnic ventilatory response; HVR = hypoxic ventilatory response; ISAM = illicit substance-abusing mother; MMT = methadone maintenance treatment. OSAHI = obstructive sleep apnea/hypopnea index; P(A-a)[O.sub.2] = alveolar-arterial oxygen pressure difference; PB =periodic breathing; [DELTA]PETC[O.sub.2] = narrowing of the proximity of eupneic and apneic end-tidal PC[O.sub.2] threshold; PtcC[O.sub.2] = transcutaneous PaC[O.sub.2]; PvC[O.sub.2] = tension of carbon dioxide in the mixed venous blood when saturated with oxygen; REM = rapid eye movement; RR = respiratory rate; SDB = sleep-disordered breathing; SIDS = sudden infant death syndrome; Sp[O.sub.2] = oxygen saturation by pulse oximetry; TST = total sleep time; VE = minute ventilation; VT = tidal volume
**********
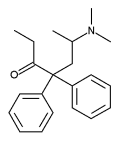
Methadone, a long-acting [micro]-opioid agonist, has been recognized as the best treatment for heroin addiction. (1,2) In 1998, > 140,000 patients were receiving methadone maintenance treatment (MMT) in the United States, and in Australia 30,000 were receiving MMT in year 2000.3 US and Australian studies (1,4) have shown that the median death rate for persons dependent on opioids and who are receiving MMT is reduced to 30% of those not receiving treatment. However, all-cause mortality rate in MMT patients is still three to four times above that of the normal population. (5) Half of the deaths occur within 2 to 3 weeks of methadone initiation and may be related to inappropriate methadone dosing and/or concomitant drug use. (6,7) The other half of deaths in MMT occur after patients are stabilized on methadone, and in the majority of these deaths the cause is unknown. (8)
[micro]-Opioids depress respiration, at least in part by a direct effect on brainstem respiratory centers. (9) Acute opioid use significantly reduces the ventilatory responsiveness to carbon dioxide (10) and hypoxia. (11-13) Infants born to illicit substance-abusing mothers (ISAMs) have been shown to have reduced hypereapnic and hypoxic ventilatory responsiveness, and have a 5 to 10 times increased risk of sudden infant death syndrome (SIDS) compared to infants born to women who are not ISAMs. (14-16)
Very little is known about the effects of long-term opioid use on respiration during sleep. In a pilot study, (17) we showed that 6 of 10 clinically stable MMT patients had central sleep apnea (CSA), some with periodic breathing (PB), whereas 9 control subjects did not have CSA. Because of the small sample size and lack of blood toxicology data, we could not make definite conclusions regarding the prevalence and possible pathogenesis of CSA in these patients. More recently, Farney et al (18) reported CSA, "ataxic breathing," sustained hypoxemia, and obstructive hypopneas in three long-term opioid users. Conclusions regarding prevalence of sleep-disordered breathing (SDB) and its pathogenesis in long-term opioid users cannot be made from this study because of the small patient numbers and lack of toxicology data and of control subjects for comparison.
We hypothesize the following: (1) CSA is prevalent in clinically stable, long-term MMT patients, and (2) there are physiologic and/or pharmacologic causes for CSA in this group of patients. We therefore conducted the present study to further assess the prevalence of CSA in clinically stable MMT patients and to investigate possible pathogenic mechanisms associated with this. We studied 50 clinically stable MMT patients and 20 age-, sex-, and body mass index (BMI)-matched non-opioid-using subjects as control subjects. We performed overnight polysomnography, blood toxicology, hypoxic ventilatory response (HVR), and hypereapnic ventilatory response (HCVR) in both groups.
MATERIALS AND METHODS
Subject Selection
MMT patients and control subjects were recruited through advertisements placed in pharmacies licensed for distributing methadone across the inner suburbs of Melbourne, Australia. The advertisement did not mention the research topic. Patients included for study had been in an MMT program for [greater than or equal to] 2 months and receiving a stable dose of methadone. Normal subjects did not have a history of substance abuse, and none were receiving opioids at the time of study. All patients underwent a screening examination by a physician skilled in diagnosis of respiratory and sleep-disordered diseases. A detailed medical history was obtained with particular reference to respiratory illness, cigarette use, current substance abuse, medication use, sleep patterns, snoring history, and each subject completed an Epworth sleepiness scale (ESS) questionnaire. (19) Exclusion criteria for study were significant cardiorespiratory, neurologic, liver disease, and psychotic disorders, and pregnancy. The institutional Research and Ethics Committee approved the protocol. All subjects gave written informed consent prior to participation.
Procedures
MMT patients underwent echocardiography, ECG, and chest radiography. All subjects underwent acclimatization polysomnography on night 1. At 8 AM the next morning, MMT patients performed respiratory function tests and arterial blood was obtained at rest and breathing air for arterial blood gas (ABG) analysis. All subjects returned at 4 PM for the HVR and HCVR tests, having fasted for 4 h prior to the test procedure. Blood was obtained for toxicology and methadone concentration 30 min prior to tests and within 6 h of patient medication with methadone. HCVR and HVR were separately tested from 4 to 6 PM, and the HVR was always performed first with at least 30 min between the tests. Polysomnography was performed for analysis on each subject on the night of the ventilatory response tests.
Polysomnography: In-laboratory attended polysomnography was performed (Compumedics E series data acquisition system; Compumedics; Victoria, Australia). The methods used to score sleep stage, arousals, and SDB have been previously described. (17) Continuous transcutaneous PaC[O.sub.2] (PtcC[O.sub.2]) was recorded (Radiometer; Copenhagen, Denmark) in the MMT patients only. The PtcC[O.sub.2] monitor was calibrated for each patient utilizing the patient's ABG result obtained on the morning prior to polysomnography. All variables were recorded continuously. Respiratory events were scored blinded using modified American Academy of Sleep Medicine criteria. (20) Apnea-hypopnea index (AHI) was calculated as the number of apneas and hypopneas divided by total sleep time (TST) in hours. Central apnea index (CAI) was defined as the number of central apneas per TST (in hours), and obstructive sleep AHI (OSAHI) was defined as obstructive apneas plus hypopneas per TST (in hours). Sleep arousals were scored according to American Sleep Disorders Association Task Force criteria and scored as number of arousals per TST (in hours). (21)
HVR: A modification of the Rebuck and Campbell (22) hypoxic and isocapnic rebreathing method was used. The subjects breathed via a closed circuit (bag in a box system) consisting of a 15-L rebreathing bag filled with 6 L of 7% C[O.sub.2] 23% [O.sub.2], and balance [N.sub.2]. With nose clip in situ, subjects breathed room air through a mouthpiece for 3 min before the circuit was closed via a three-way valve. The subjects then took three deep breaths and breathed at tidal volume (VT) after that. Rebreathing continued until the arterial oxygen saturation measured by pulse oximetry (Sp[O.sub.2]) [Biox 3740; Ohmeda; Louisville, CO] dropped to 80% or if the subject became distressed. Expired fractional concentration of carbon dioxide (FAC[O.sub.2]) was measured by a rapid carbon dioxide analyzer (model 17630; VacuMed; Ventura, CA). Soda lime in the inspiratory limb of the circuit was used to keep FAC[O.sub.2] within the isocapnic range (< 7%). At no stage did any subject become hypercapnic during this test procedure.
HCVR: A modification of Bead's rebreathing method (23) was used. The equipment was similar to that of the HVR test. The differences were as follows: (1) the gas in the rebreathing bag contained a mixture of 7% C[O.sub.2] 50% [O.sub.2], and balance [N.sub.2]; the carbon dioxide absorber was absent; and (3) a fuel-cell rapid oxygen analyzer (Fisher & Paykel Healtheare; Victoria, Australia) was connected to the circuit to measure fractional inspired oxygen. The subjects were connected to the circuit as per the HVR test. They were asked to rebreathe on the circuit to a minimum fractional inspired oxygen of 22% or if the subject became distressed, whichever occurred first. At no stage did any subject exhibit a significant drop of Sp[O.sub.2] from baseline during the test procedure.
Data Processing and Analysis for the HVR and HCVR Tests,: Breath-by-breath minute ventilation (VE), VT, respiratory rate (RR), and the time stamp for each breath were measured (RSS100HR Research Pneumotach System; Hans Rudolph; Kansas City, MO) and recorded by software (RSS100HR) through the digital output of the system. The pneumotach system also had an analog output connected to an analog-to-digital card. The oximeter and carbon dioxide analyzer were also connected to the card. The software for the analog-to-digital card (Logger; Total Turnkey Solutions; Sydney, Australia) allowed for data acquisition. Second-by-second data of gas volume, FaC[O.sub.2]), and Sp[O.sub.2] were recorded to computer by Logger software together with breath-by-breath data recorded by RSS100HR. The data recorded were then merged (SPSS version 11; SPSS; Chicago, IL) to obtain the breath-by-breath VE, FAC[O.sub.2], and Sp[O.sub.2] data. All volumes were corrected to body temperature and pressure and saturated with water vapor. FaC[O.sub.2] was converted to tension of carbon dioxide in the mixed venous blood when saturated with oxygen (PvC[o.sub.2]) using the formula "PvC[O.sub.2] = FAC[O.sub.2] x (Pb - P[H.sub.2]O)," where (Pb - P[H.sub.2]O) is the pressure of dry gas in the lung at 37[degrees]C. Daily barometric pressure (Pb) values were obtained from the Melbourne Meteorology Bureau. [DELTA]VE/[DELTA]PvC[O.sub.2], and [DELTA]VE/[DELTA]Sp[O.sub.2] were calculated as the slope of linear regression (line of best fit). Similarly, the slopes of [DELTA]VT/[DELTA]PvC[O.sub.2] and [DELTA]RR/[DELTA]PvC[O.sub.2] in HCVR test and [DELTA]VT/[DELTA]Sp[O.sub.2] and [DELTA]RR/[DELTA]Sp[O.sub.2] in HVR test were also tested. To eliminate errors in the breath-by-breath analysis, those breaths lying > 2 SD outside the regression line were discarded, and the regression line was recalculated. (24) For the HVR test, the VE for Sp[O.sub.2] < 95% was used to calculate the regression line. The signal time delay of the oximeter was corrected for each analysis, and absolute values of slopes were applied to the HVR test. (25)
Toxicology: All subjects had blood obtained for toxicology. The collected blood samples were stored at -20[degrees]C until analysis. Testing included an alcohol screen by gas chromatography and an enzyme-linked immunosorbent assay screen (Microgenics; Freemont, CA) for drugs of abuse (amphetamines, benzodiazepines, cocaine, cannabinoids, and opioids). Blood was also screened for 3,4-methylenedioxymethamphetamine ("ecstasy"), methadone, meperidine, benzodiazepines, antidepressants, and other prescription and over-the-counter drugs using a validated gas chromatography-mass spectrometry technique. (26) Methadone blood concentrations were quantified using high-performance liquid chromatography procedures routinely used in the laboratory (Victorian Institute of Forensic Medicine). The precision of this assay is [+ or -] 5%.
Resting Cardiac and Respiratory Function Tests: The MMT patients underwent chest radiography, ECG, echocardiography, spirometry, carbon monoxide transfer measurement, and ABG estimation. For details of tests performed and the methods employed to assess resting cardiorespiratory function, see Teichtahl et al. (27)
Statistical Analysis
All values were expressed as mean [+ or -] SD unless otherwise stated. Paired and unpaired Student t tests were used tot between-group differences for normally distributed variables. Mann-Whitney rank-sum test (28) was used to test group difference between nonnormally distributed variables. All skewed variables were logarithmically or squarely transformed. Logarithmically transformed CAI was the dependent variable. Independent variables were screened from blood toxicology and respiratory function tests based on physiologically plausible, clinically significant, and significance on univariate regression with log CAI. All variables included in analysis were screened for collinearity. A correlation of 0.9 was set as the upper limit of noncollinearity. (29) Pearson correlation coefficient (30) was used to examine the association between dependent variable and individual independent variable. A multiple linear regression model (backward deletion) (29) was used to determine the factors associated with degree of CAI Statistical analysis was performed using software (SPSS 11; SPSS; Chicago, IL). Statistical significance was set at p < 0.05.
RESULTS
Sixty-two MMT patients consented to take part in the study. Three patients were excluded due to poorly controlled asthma. One patient was excluded because of previous severe head injury. Another patient was excluded because of pregnancy. In addition, two patients withdrew from the study due to family commitments. Four patients were unable to be contacted after consenting to participate in the study. One MMT patient died of drug overdose prior to performing study tests. This left 50 MMT patients who underwent study and who had data for analysis. All patients had previous heroin addiction, and most had additional polydrug abuse. The duration and extent of previous drug abuse history are difficult to document in this group of patients. The 20 normal subjects recruited to the study completed all test procedures. Table 1 shows the demographic data and blood toxicology of the patients and control subjects. The MMT patients and normal subjects were well matched for age, sex, and BMI.
SDB
Figure 1 shows the overall AHI for both MMT patients and normal subjects. The MMT patients had significantly higher total AHI then did the normal subjects (p < 0.05). No significant difference was found in OSAHI between the MMT and control groups (Fig 2). Fifteen MMT patients (30%) had a CAI > 5, and 10 patients (20%) had a CAI > 10. No normal subject had CAI > 1. Ten of the 15 MMT patients with a CAI > 5 had a coexistent OSAHI > 5, whereas the remaining 5 patients had an OSAHI < 5. The median CAI for MMT patients was 1.7 (range, 0 to 93), and the median CAI for control subjects was 0.15 (range, 0 to 1) [p < 0.001]. The distribution of CAI in MMT patients and normal subjects is listed in Table 2. Examples of the types of CSA found in MMT patients are shown in Figure 3. The central apnea events occurred predominantly in non-rapid eye movement (REM) sleep, whereas more obstructive SDB occurred in REM sleep than non-REM sleep for both the patients and normal subjects (Table 3).
[FIGURES 1-3 OMITTED]
Physiologic Parameters
MMT patients tended to have lower overnight Sp[O.sub.2] nadir compared to the control subjects (91.5 [+ or -] 3.3% vs 93.0 [+ or -] 2.5%, p = 0.059), and their average peak overnight PtcC[o.sub.2] was 46.6 [+ or -] 5.3 mm Hg. MMT patients were found to have significantly elevated HVR compared to control subjects (2.14 [+ or -] 1.58 L/min/% Sp[O.sub.2] vs 1.12 [+ or -] 0.7 L/min/% Sp[O.sub.2], p = 0.008), whereas their HCVR was significantly lower than control subjects (1.27 [+ or -] 0.61 L/min/mm Hg vs 1.64 [+ or -] 0.57 L/min/mm Hg, p = 0.01). Ten MMT patients (20%) had awake PaC[O.sub.2] > 45 mm Hg, and 14 patients (28%) had alveolar-arterial oxygen pressure gradient P(A-a)[O.sub.2] > 15 mm Hg. Further resting cardiorespiratory data for the MMT patients can be reviewed in our previous publication. (27) The MMT patients had normal resting cardiac function. (27)
Correlations Between CSA in MMT Patients, Physiologic Parameters, and Toxicology
After screening, 18 variables were selected as independent variables for predicting the presence of CSA. The variables were selected from blood toxicology, HVR, HCVR, respiratory function test results, and sleep data. Univariate regressions showed that log methadone blood concentration, P(A-a)[O.sub.2], overnight Sp[O.sub.2] nadir, Pa[O.sub.2], and the peak sleep PtcC[O.sub.2] were significantly correlated with log CAI (Table 4). Stepwise multiple linear regression revealed that log methadone blood concentration was the only statistically significant variable associated with log CAI (t = 2.33, p = 0.025) and is associated with 12% of the variance of log CAI. The next four associated variables were PaC[O.sub.2], antidepressant use, HCVR, and P(A-a)[O.sub.2], and these together were associated with a further 17% of the variance of CAI.
Sleep Architecture Parameters
Table 5 shows the sleep architecture, arousal index, and ESS for the MMT patients and normal subjects. MMT patients had significantly less REM sleep and stage 1 sleep and more stage 2 sleep compared to the normal subjects. In addition, the MMT patients had significantly more daytime sleepiness when compared to the normal subjects as measured by the ESS. However, only four of the MMT patients and no normal subject had ESS scores > 11. There was no significant difference in the above parameters for MMT patients with and without CSA.
DISCUSSION
To our knowledge, this is the first study to assess the prevalence of SDB in clinically stable MMT patients in a large number of patients and to have compared the data with a matched non-opioid-using control group. We have confirmed our previous findings of a high prevalence of CSA in stable MMT patients. (17) Our study has also shown that clinically stable MMT patients do not have significantly different obstructive SDB when compared to control subjects and that the difference in AHI found between the two groups is due to CSA in MMT patients. Of interest is our finding that central apneas occurred more often in non-REM sleep than REM sleep in MMT patients and that obstructive respiratory events occurred snore often in REM sleep than non-REM sleep in both groups tested. These findings are in keeping with current knowledge and hypotheses regarding the genesis of SDB. (31) Compared to our pilot study, we have also endeavored to delineate the pathogenesis of the CSA in clinically stable MMT patients using a multiple regression model with variables selected from a comprehensive suite of measurements including blood toxicology, resting cardiorespiratory function, and parameters of ventilatory control.
The sleep architecture, arousal index, and ESS data found in this study are similar to that of our pilot study. (17) There is no relationship noted in our current study between these parameters and CSA, possibly because of the relatively small number of patients with CSA in this study. The data, however, do show that clinically stable MMT patients have reduced REM sleep and increased daytime sleepiness when compared to normal subjects and that this in its own right may impact their ability to function in society. (17)
We have not shown a simple cause-and-effect relationship between the toxicology and physiologic variables we measured and CSA in clinically stable MMT patients. Our patients have normal resting cardiac function, and the CSA examples shown in Figure 2 are clearly not of the crescendo-decrescendo shape and have a much shorter cycle time than Cheyne-Stokes respiration seen in severe chronic heart failure. (27,32) The CSA in our patients is not typical of nonhypercapnic idiopathic CSA, as the latter is associated with frequent transition from wakefulness to sleep, (33,34) and our patients have the same arousal index as normal subjects. In addition, nonhypercapnic idiopathic CSA occurs after hyperventilation and has a striking male preponderance, (33) whereas CSA was noted in our study to occur in nine female and six male patients. It is unlikely that the CSA in MMT patients is of the purely hypercapnic type given the mild abnormalities of awake and asleep PC[O.sub.2] found in this group. In addition, the MMT patients have a mean awake Pa[O.sub.2] of 86.5 [+ or -] 13.2 mm Hg and Sp[O.sub.2] nadir of 91.4 [+ or -] 3.3% during sleep, which would exclude hypoxia alone as the main driver for the CSA found in the MMT patients. (27)
Because of the above, we believe that the CSA in clinically stable MMT patients may be multifactorial in nature and related to abnormalities of the central controller and central and peripheral metabolic control mechanisms. Indeed, each patient may have variable input from these abnormalities in the genesis of their CSA. We therefore hypothesize that for individual MMT patients with CSA, there may be variable input from the following potential pathophysiologic mechanisms.
Central Controller
Methadone is a [micro]-opioid receptor antagonist, and its central respiratory depressant effect may be a critical mechanism in the genesis of CSA in our patient group. (9) Our results show that methadone blood concentration is the most significant predictor of the severity of CSA in MMT patients, although it explains only 12% of CAI. In part, the relatively low predictive value of methadone blood concentration for CSA in our patients may be related to intersubject variability of methadone pharmacokinetics. (35) As we measured the methadone blood concentration at one point in time, we may have missed the relevant methadone blood concentration in some subjects.
Another mechanism that could be implicated causing CSA via central controller pathology in MMT patients is brainstem and/or midbrain structural abnormalities. Heroin use has been known to be associated with stroke through mechanisms such as thromboembolism, vasculitis, septic emboli, hypotension, and positional vascular compression. (36) Other complications include hypoxic ischemic changes with cerebral edema, ischemic neuronal damage, and neuronal loss, which are assumed to occur under conditions of prolonged heroin-induced respiratory depression. (36) In addition, substances used as adulterants such as amphetamineav-39 and cocaine (40,41) can cause brain damage either alone or in combination with heroin. As all of our clinically stable MMT patients were past heroin users, we cannot exclude structural brain damage as a major factor in the pathogenesis of the CSA described. Functional and structural MBI studies of the brain would be of value in evaluating this possibility.
Hypercapnic Type CSA
Hypercapnic type CSA may play a role in some of our patients. This type of CSA is characterized by elevated awake daytime PaC[O.sub.2] and blunted HCVB. (31,33) The mean awake PaC[O.sub.2] of the MMT patients was 42.2 [+ or -] 3.8 mm Hg, and their mean peak PtcC[O.sub.2] was 46.5 [+ or -] 5.4 mm Hg during sleep. Although 10 of the MMT patients had awake PaC[O.sub.2] of > 45 mm Hg, their hypereapnia was mild with the highest being 50 mm Hg, and we did not find a statistically significant relationship between awake PaC[O.sub.2] alone and CAI. (27) Our patients also have significantly decreased HCVR compared to the control group. The tendency to mildly raised awake PaC[O.sub.2] has previously been noted in clinically stable MMT patients. (42) The mean awake PaC[O.sub.2] and sleep PtcC[O.sub.2] in our MMT patient group tended to upper limits of normal, although not clearly in the more severe hypercapnic range noted in the hypercapnic type CSA. Nevertheless awake PaC[O.sub.2] and blunted HCVR combined were weak predictors for CSA in our patients.
Antidepressant use may in combination with blunted HCVR have a significant relationship with CSA in our patients. Four of seven patients (57%) receiving antidepressants had a CAI > 10. Antidepressants have been used for treatment of panic disorder and are known to acutely depress HCVB in this group of patients. (43-45) It is therefore possible that antidepressants act in synergy with methadone to further blunt HCVR in MMT patients and to predispose them to CSA. We have not shown a relationship between the use of benzodiazepines and cannabis and CSA in our patient group, and this may be due to the small number of patients in this study using the drugs. HCVR is increased after short-term dosing with cannabis and short-term use of benzodiazepines reduces HCVR in normal subjects. (46,47) Animal models suggest that short-term dosing with benzodiazepines potentiates the effects of opioids on ventilation. (48) To our knowledge, there is no literature regarding the effects of long-term use of antidepressants, benzodiazepines, and cannabis on respiratory control mechanisms or on respiration during sleep. Given the large number of subjects that use these drugs, this area of medical research needs to be addressed.
Hypoxia and CSA
CSA associated with hypoxia is seen in high-altitude PB during sleep (49) and in chronic heart failure patients. (32) The narrowing of the proximity of eupneic and apneic end-tidal PC[O.sub.2] threshold ([DELTA]PETC[O.sub.2]) has been suggested as a major mechanism for CSA. (31) A typical example is that patients with CHF and CSA show a decreased [DELTA]PETC[O.sub.2] and a greater hypocapnic ventilatory response below eupnea compared to patients with chronic heart failure but without CSA. (50) Xie et al (51) found that hypoxia can decrease the [DELTA]PETC[O.sub.2] by mainly decreasing eupneic PaC[O.sub.2]. The combination of a low eupneie PaC[O.sub.2] and a relatively high apneic PaC[O.sub.2] threshold makes it easier for transient reductions of PaC[O.sub.2] to reach the apneic threshold and cause breathing instability. In our study, multiple regression analysis revealed that P(A-a)[O.sub.2] is an important although weakly associated variable with CSA severity in the MMT patients. As there was unacceptable collinearity between Pa[O.sub.2] and P(A-a)[O.sub.2], Pa[O.sub.2] was not included as an independent variable in our statistical model. Nevertheless, bivariate Pearson correlation between Pa[O.sub.2] and log CAI is significant (r =- 0.31, p < 0.05), suggesting an association between resting Pa[O.sub.2] and CSA in the MMT patients. Polysomnography data revealed that MMT patients tended to have a lower Sp[O.sub.2] nadir (91.5 [+ or -] 3.3%) than the control subjects (93.1 [+ or -] 2.5%) [p = 0.059]. Fourteen of our MMT patients (28%) had P(A-a)[O.sub.2] > 15 mm Hg, including 7 patients with Pa[O.sub.2] < 70 mm Hg. (27) Therefore, we believe the mild hypoxia found in our patients could contribute to their CSA via the mechanism described above.
It has been reported that exposing subjects to very mild and short-term hypoxia can cause an increase in HVR. (52) Our MMT patients have significantly higher HVR compared to the control subjects, and high peripheral chemoreceptor activity has been reported to be a predisposing factor for SDB. (53) Dunai et al (53) demonstrated that subjects with high peripheral chemoreceptor drive experienced significantly greater amplification of state-related ventilatory fluctuations than those with low peripheral chemoreceptor drive. We therefore suspect that the high HVR in our MMT patients may be another predisposing factor for their CSA.
We believe the three major mechanisms related to the genesis of CSA as described above may contribute to the CSA we have found in stable MMT patients. Each mechanism alone may not be sufficient to cause CSA in this group of patients. A varying interplay between the mechanisms is probably responsible for our findings. Support for this postulate can be found in the study of Nakayama et al, (54) who found that an imbalance between high peripheral and low central chemosensitivity poses a risk for PB. Indeed, Nakayama et al (55) believe that instability of breathing patterns tends to occur when carotid chemoreceptor stimulation becomes the dominant sensory input to the respiratory controller relative to the level of medullary chemoreceptors.
The causes of the high mortality rate in clinically stable MMT patients cannot be explained by our study. ISAMs have a higher total duration of apneas (56) and an impaired repertoire of protective responses to hypercapnia and hypoxia during sleep, (16) and these may play a role in their increased risk of SIDS. Infants born to mothers receiving MMT also have decreased HVR and a higher than normal prevalence of SIDS. (57,58) There may be a unifying mechanism to explain the CSA and deaths in our MMT patients, ISAMs, and infants born to mothers receiving MMT. Our study did not address the issue of excess mortality in clinically stable MMT patients; nevertheless, our findings suggest that the role of SDB in stable MMT patients deaths needs further evaluation.
In conclusion, our results show that 30% of stable MMT patients have CSA. Methadone blood concentration is significantly associated with the severity of CSA found but accounts for only 12% of CSA. The pathogenesis of CSA in clinically stable MMT patients needs to be further explored by studying the potential roles of antidepressant use, brainstem structural abnormalities, and central and peripheral ventilatory control mechanisms.
ACKNOWLEDGMENT: The authors thank the Department of Statistics, University of Melbourne, for statistical assistance.
REFERENCES
(1) NIH Consensus Conference. Effective medical treatment of opiate addiction. National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction. JAMA 1998; 280:1936-1943
(2) Caplehorn JRM, Batty RG. Methadone maintenance in Australia. J Drug Issues 1992; 22:661-678
(3) Ministerial Council on Drug Safety. National background plan on illicit drugs, 2001 to 2002-2003; background paper. Canberra, Australia, 2001; 34
(4) Caplehorn JR, Dalton MS, Cluff MC, et al. Retention in methadone maintenance and heroin addicts' risk of death. Addiction 1994; 89:203-209
(5) Zador D, Sunjie S, Basili H. All-cause mortality rate and risk of dying in methadone maintenance treatment in New South Wales in 1990 95. International Opioid Overdose Symposium. Sydney, Australia: National Drug and Alcohol Research Centre, 1997
(6) Caplehorn JR. Deaths in the first two weeks of maintenance treatment in NSW in 1994: identifying cases of iatrogenic toxicity. Drug Alcohol Rev 1998; 17:9-17
(7) White JM, Irvine RJ. Mechanisms of fatal opioid overdose. Addiction 1999; 94:961-972
(8) Caplehorn JR, Drummer OH. Mortality associated with New South Wales methadone programs in 1994: lives lost and saved. Med J Aust 1999; 170:104-109
(9) Gutstein H, Akil H, eds. Opioid analgesics. New York, NY: McGraw-Hill, 2001
(10) Bailey PL, Stanley TH. Intravenous opioid anesthetics. In: Miller RD, ed. Anesthesia. New York, NY: Churchill Livingston, 1994; 291-389
(11) Weil JV, McCullough RE, Kline JS, et al. Diminished ventilatory response to hypoxia and hypercapnia after morphine in normal man. N Engl J Med 1975; 292:1103-1106
(12) Berkenbosch A, Teppema LJ, Olievier CN, et al. Influences of morphine on the ventilatory response to isocapnic hypoxia. Anesthesiology 1997; 86:1342-1349
(13) Bailey PL, Lu JK, Pace NL, et al. Effects of intrathecal morphine on the ventilatory response to hypoxia. N Engl J Med 2000; 343:1228-1234
(14) Wingkun JG, Knisely JS, Schnoll SH, et al. Decreased carbon dioxide sensitivity in infants of substance-abusing mothers. Pediatrics 1995; 95:864-867
(15) Ward SL, Bautista D, Chan L, et al. Sudden infant death syndrome in infants of substance-abusing mothers. J Pediatr 1990; 117:876-881
(16) Ward SL, Bautista DB, Woo MS, et al. Responses to hypoxia and hypercapnia in infants of substance-abusing mothers. J Pediatr 1992; 121:704-709
(17) Teichtahl H, Prodromidis A, Miller B, et al. Sleep-disordered breathing in stable methadone programme patients: a pilot study. Addiction 2001; 96:395-403
(18) Farney RJ, Walker JM, Cloward TV, et al. Sleep-disordered breathing associated with long-term opioid therapy. Chest 2003; 123:632-639
(19) Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991; 14:540-545
(20) AASM Task Force. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement technique in clinical research. Sleep 1999; 22:667-689
(21) American Sleep Disorders Association. EEG arousals: scoring rules and examples; a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep 1992; 15:173-184
(22) Rebuck AS, Campbell EJ. A clinical method for assessing the ventilatory response to hypoxia. Am Rev Respir Dis 1974; 109:345-350
(23) Read DJ. A clinical method for assessing the ventilatory response to carbon dioxide. Australas Ann Med 1967; 16: 20-32
(24) Prisk GK, Elliott AR, West JB. Sustained microgravity reduces the human ventilatory response to hypoxia but not to hypercapnia. J Appl Physiol 2000; 88:1421-1430
(25) Shaw RA, Schonfeld SA, Whitcomb ME. Progressive and transient hypoxie ventilatory drive tests in healthy subjects. Am Rev Respir Dis 1982; 126:37-40
(26) Drummer OH, Horomidis S, Kourtis S, et al. Capillary gas chromatographic drug screen for use in forensic toxicology. J Anal Toxieol 1994; 18:134-138
(27) Teichtahl H, Wang D, Cunnington D, et al. Cardiorespiratory function in stable methadone maintenance program patients. Addict Biol 2004; 3-4:247-253
(28) Siegel S, Castellan NJ. Non parametric statistics for the bahavioral sciences. 2nd ed. New York, NY: McGraw-Hill, 1988
(29) Tabachnick B, Fidell L. Using multivariate statistics. 4th ed. Boston, MA: Allyn and Bacon, 2001
(30) Portney LG, Watkins MP. Foundations of clinical research applications to practice. Stamford, CT: Appleton & Lange, 1993
(31) Bradley TD. Crossing the threshold: implications for central sleep apnea. Am J Respir Crit Care Med 2002; 165:1203-1204
(32) Naughton MT. Pathophysiology and treatment of Cheyne-Stokes respiration. Thorax 1998; 53:514-518
(33) Bradley TD, Phillipson EA. Central sleep apnea. Clin Chest Med 1992; 13:493-505
(34) Bradley TD, McNicholas WT, Rutherford R, et al. Clinical and physiologic heterogeneity of the central sleep apnea syndrome. Am Rev Respir Dis 1986; 134:217-221
(35) Eap C, Buclin T, Baumann P. Interindividual variability of the clinical pharmacokinetics of methadone: implications for the treatment of opioid dependence. Clin Pharmacokinet 2002; 41:11503-11593
(36) Buttner A, Mall G, Penning R, et al. The neuropathology of heroin abuse. Forensic Sci Int 2000; 113:435-442
(37) Manchanda S, Connolly MJ. Cerebral infarction in association with Ecstasy abuse. Postgrad Med J 1993; 69:874-875
(38) Yen DJ, Wang SJ, Ju TH, et al. Stroke associated with methamphetamine inhalation. Eur Neurol 1994; 34:16-22
(39) Perez JA Jr, Arsura EL, Strategos S. Methamphetamine-related stroke: four cases. J Emerg Med 1999; 17:469-471
(40) O'Brien CP. Stroke in young women who use cocaine or amphetamines. Epidemiology 1998; 9:587-588
(41) Petitti DB, Sidney S, Quesenberry C, et al. Stroke and cocaine or amphetamine use. Epidemiology 1998; 9:596-600
(42) Marks CE Jr, Goldring RM. Chronic hypercapnia during methadone maintenance. Am Rev Respir Dis 1973; 108: 1088-1093
(43) Bocola V, Trecco MD, Fabbrini G, et al. Antipanic effect of fluoxetine measured by C[O.sub.2] challenge test. Biol Psychiatry 1998; 43:612-615
(44) Pols H, Lousberg H, Zandbergen J, et al. Panic disorder patients show decrease in ventilatory response to C[O.sub.2] after clomipramine treatment. Psychiatry Res 1993; 47:295-296
(45) Klein DF. False suffocation alarms, spontaneous panics, and related conditions: an integrative hypothesis. Arch Gen Psychiatry 1993; 50:306-317
(46) Zwillich CW, Doekel R, Hammill S, et al. The effects of smoked marijuana on metabolism and respiratory control. Am Rev Respir Dis 1978; 118:885-891
(47) Gross JB, Blouin RT, Zandsberg S, et al. Effect of flumazenil on ventilatory drive during sedation with midazolam and alfentanil. Anesthesiology 1996; 85:713-720
(48) Gerak LR, Brandt MR, France CP. Studies on benzodiazepines and opioids administered alone and in combination in rhesus monkeys: ventilation and drug discrimination. Psychopharmacology (Berl) 1998; 137:164-174
(49) Lahiri S, Maret K, Sherpa MG. Dependence of high altitude sleep apnea on ventilatory sensitivity to hypoxia. Respir Physiol 1983; 52:281-301
(50) Xie A, Skatrud JB, Puleo DS, et al. Apnea-hypopnea threshold for C[O.sub.2] in patients with congestive heart failure. Am J Respir Crit Care Med 2002; 165:1245-1250
(51) Xie A, Skatrud JB, Dempsey JA. Effect of hypoxia on the hypopnoeic and apnoeic threshold for C[O.sub.2] in sleeping humans. J Physiol 2001; 535:269-278
(52) Fatemian M, Kim DY, Poulin MJ, et al. Very mild exposure to hypoxia for 8 h can induce ventilatory acclimatization in humans. Pflugers Arch 2001; 441:840-843
(53) Dunai J, Kleiman J, Trinder J. Ventilatory instability during sleep onset in individuals with high peripheral chemosensitivity. J Appl Physiol 1999; 87:661-672
(54) Nakayama H, Smith CA, Rodman JR, et al. Effect of ventilatory drive on carbon dioxide sensitivity below eupnea during sleep. Am J Respir Crit Care Med 2002; 165:1251-1260
(55) Nakayama H, Smith CA, Dempsey J. Effects of background ventilatory stimuli on the apneic threshold (AT) in sleeping dogs [abstract]. Am J Respir Crit Care Med 2001; 163:A179
(56) Ward SL, Schuetz S, Kirshna V, et al. Abnormal sleeping ventilatory pattern in infants of substance-abusing mothers. Am J Dis Child 1986; 140:1015-1020
(57) Olsen GD, Lees MH. Ventilatory response to carbon dioxide of infants following chronic prenatal methadone exposure. J Pediatr 1980; 96:983-989
(58) Pierson PS, Howard P, Kleber HD. Sudden deaths in infants born to methadone-maintained addicts. JAMA 1972; 220: 1733-1734
* From the Department of Respiratory & Sleep Disorders Medicine (Drs. Wang, Teichtahl, and Cunnington and Ms. Cherry), Drug and Alcohol Service (Dr. Kronborg and Ms. Goodman), Western Hospital; and Victorian Institute of Forensic Medicine (Dr. Drummer), Victoria, Australia.
This study was supported by the Australian Postgraduate Awards (D.W.) the Western Hospital Education, Equipment and Research Fund, and the Western Hospital Liver Research Fund.
Manuscript received December 13, 2004; revision accepted February 17, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Harry Teichtahl, MBBS, Department of Bespiratory & Sleep Disorders Medicine, Western Hospital, Gordon St, Footscray, Victoria, Australia 3011; e-mail: harry.teichtahl@wh.org.au
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group