Rationale: Methadone is a long-acting [mu]-opioid and is an effective treatment for heroin addiction. Opioids depress respiration, and patients receiving methadone maintenance treatment (MMT) have higher mortality than the general population. Few studies have investigated ventilatory responses to both hypercapnia and hypoxia in these patients.
Study objectives: We measured hypercapnic ventilatory response (HCVR) and hypoxic ventilatory response (HVR) and investigated possible factors associated with both in clinically stable patients receiving MMT.
Design and setting: Patients receiving long-term, stable doses of methadone recruited from a statewide MMT program, and normal, non-opioid-using subjects matched for age, sex, height, and body mass index were studied with HCVR and HVR.
Results: Fifty MMT patients and 20 normal subjects were studied, and significantly decreased HCVR and increased HVR were found in MMT patients compared to normal subjects (HCVR [mean [+ or -] SD], 1.27 [+ or -] 0.61 L/min/mm Hg vs 1.64 [+ or -] 0.57 L/min/mm Hg [p = 0.01]; HVR, 2.14 [+ or -] 1.58 L/min/% arterial oxygen saturation measured by pulse oximetry [Sp[O.sub.2]] vs 1.12 [+ or -] 0.7 L/min/% Sp[O.sub.2] [p = 0.008]). Respiratory rate and not tidal volume changes were the major physiologic responses contributing to both HCVR and HVR differences between the groups. Variables associated with HCVR in the MMT patients are as follows: obstructive sleep apnea/ hypopnea index (t = 5.1, p = 0.00001), PaC[O.sub.2] (t = - 3.6, p = 0.001), body height (t = 2.6, p = 0.01) and alveolar-arterial oxygen pressure gradient (t = 2.5, p = 0.02). Variables associated with HVR in MMT patients are body height (t = 3.2, p = 0.002) and Pac[O.sub.2] (t = - 2.8, p = 0.008).
Conclusions: Stable long-term MMT patients have blunted central and elevated peripheral chemoreceptor responses. The mechanisms and clinical significance of these findings need further investigation.
Key words: chronic opioids; hypercapnic ventilatory response; hypoxic ventilatory response; respiratory rate; tidal
Abbreviations: CAI = central apnea index; DLCO = diffusion capacity of the lung for carbon monoxide; FAC[O.sub.2] = expired fractional concentration of carbon dioxide; HCVR = hypercapnic ventilatory response; HVR = hypoxic ventilatory response; MMT = methadone maintenance treatment; OSAHI = obstructive sleep apnea/hypopnea index; P(A-a)[O.sub.2] = alveolar arterial oxygen pressure gradient; PvC[O.sub.2] = tension of carbon dioxide in the mixed venous blood when saturated with oxygen; RR = respiratory rate; Sp[O.sub.2] = arterial oxygen saturation measured by pulse oximetry; VE = minute ventilation; VT = tidal volume
**********
Illicit opiate use is a major worldwide problem. The prevalence of heroin use in the United States was 3 million in 1999 (1) and 74,000 from 1997 to 1998 in Australia. (2) The population prevalence of heroin dependence is 6.9 per 1,000 adults aged 15 to 54 years in Australia and is the same as in Britain (7 per 1,000) and in the European Union (3 to 8 per 1,000). (2)
Methadone, a long-acting [mu]-opioid agonist blocks the narcotic effects of heroin and relieves craving and the abstinence syndrome,a Methadone maintenance treatment (MMT) is recognized as an effective treatment for heroin addiction. (3-5( Although MMT reduces the risk of death of opioid users by a factor of three to four, all-cause mortality in MMT patients is three to four times higher than that of the general population. (6,7)
[mu]-Opioids depress respiration, at least in part by virtue of a direct effect on the brainstem respiratory centers. (8) Acute respiratory depression occurs with most commonly used opioid anesthetics. (9-12) In humans, the primary receptors are assumed to be [mu]-receptor type. (13) All [mu]-receptor-stimulating opioids cause acute dose-dependent depression of respiration, (14) primarily through direct action on brainstem respiratory centers. (15) Acute opioid use significantly reduces the responsiveness of the brainstem respiratory centers to carbon dioxide (13) and the slopes of the hypereapnic ventilatory response (HCVR) are decreased and shifted to the right. (16) In addition, studies (16-18) have reported that acute, low-dose opioid analgesia use can acutely decrease hypoxie ventilatory response (HVR).
Few studies have investigated HCVR (19-21) and HVR (20) in long-term opioid users such as MMT patients. To our knowledge, only one study (20) assessed both HCVR and HVR in the same group of patients, and the gender distribution in the three other studies was skewed to male MMT patients. (19-21) MMT patients often ingest other drags that may significantly confound HCVR and HVR, and the previous studies (3,19-21) did not assess blood toxicology of the patients studied. The combination of concomitant opioid, alcohol, antidepressants, or benzodiazapine use in this patient group may present a greater risk of respiratory depression. (8)
We have previously shown that MMT patients have a high prevalence of central sleep apnea. (22,23) As part of a project addressing the potential mechanisms of central sleep apnea in stable MMT patients, we wished to assess the HVR and HCVR in this patient group. The hypotheses for this study are as follows: (1) HVR and HCVR findings are abnormal in clinically stable MMT patients compared to normal, non-opioid-using subjects; and (2) physiologic and toxicologic factors explain these abnormalities.
MATERIALS AND METHODS
This study forms part of a project assessing sleep architecture and sleep-disordered breathing in stable MMT patients.
Subject Selection
MMT patients and normal, non-opioid-using subjects were recruited through advertisements placed in pharmacies licensed for distributing methadone across the inner suburbs of Melbourne, Australia. The advertisement did not mention the research topic. The patients had been receiving MMT for [greater than or equal to] 2 months with a stable dose of methadone. The normal subjects did not have a history of substance abuse, and none were using opioids at the time of study. All subjects underwent a screening examination by a physician skilled in the diagnosis of respiratory and sleep-disordered diseases. A detailed medical history was obtained with particular reference to respiratory illness, cigarette use, current substance abuse, medication use, sleep patterns, and snoring history. Exclusion criteria for study were significant cardiorespiratory, neurologic, liver, and psychotic disorders, and pregnancy. The institutional Research and Ethics committee approved the protocol. All subjects gave written informed consent prior to participation.
Procedures
MMT patients underwent echocardiography, ECG, and chest radiography. M1 subjects underwent acclimatization polysomnography on night 1. At 8 AM the next morning, MMT patients underwent respiratory function tests, and arterial blood was sampled at rest and when breathing air for arterial blood gas analysis. All subjects returned at 4 PM for the HVR and HCVR tests, having fasted for 4 h prior to the test procedure. Blood was taken for toxicology and methadone concentration 30 min prior to tests and within 6 h of medication with methadone. HCVR and HVR were separately tested from 4 to 6 PM, and the HVR was always performed first with at least 30 min between the tests. Polysomnography was performed for analysis on each subject on the night of the ventilatory response tests.
HVR: A modification of the Rebuck and Campbell (24) hypoxic, isocapnic rebreathing method was used. The subjects breathed via a closed circuit (bag in a box system) consisting of a I5-L rebreathing bag filled with 6 L of 7% C[O.sub.2], 23% [O.sub.2], and balance [N.sub.2]. With nose clip in situ, subjects breathed room air through a mouthpiece for 3 min before the circuit was closed via a three-way valve. The subjects then took three deep breaths and breathed at tidal volume (VT) after that. Rebreathing continued until the oxygen saturation measured by pulse oxianetry (Sp[O.sub.2]) [Ohmeda Biox 3740; Louisville, CO] dropped to 80% or if the subject became distressed. End-tidal C[O.sub.2] percentage was measured by a rapid C[O.sub.2] analyzer (model 17630; VacuMed; Ventura, CA). Soda lime in the inspiratory limb of the circuit was used to keep expired fractional concentration of C[O.sub.2] (FAC[O.sub.2]) at < 7% for all subjects. There was no evidence of hypercapnia on expired gases on this test procedure for patients and normal subjects.
HCVR: A modification of Read's rebreathing method (25) was used. The equipment was similar to that of the HVR test. The differences were as follows: (1) gas in the rebreathing bag contained a mixture of 7% C[O.sub.2], 50% [O.sub.2], and balance [N.sub.2]; (2) the carbon dioxide absorber was absent; (3) a fuel-cell rapid oxygen analyzer (Fisher & Paykel Healthcare; Victoria, Australia) was connected to the circuit to measure fractional inspired oxygen. The subjects were connected to the circuit as per the HVR test. They were asked to rebreathe on the circuit to a minimum fractional inspired oxygen of 22% or if the subject became distressed, whichever occurred first.
For both the HVR and HCVR tests, breath-by-breath minute ventilation (VE), VT, respiratory rate (RR), and the time stamp for each breath were measured (RSS100HR Research Pneumotach System; Hans Rudolph; Kansas City, MO) and recorded (RSS100HR software; Hans Rudolph) through the digital output of the system. The pneumotach system also had an analog output connected to an analog-to-digital card. The oximeter and C[O.sub.2] analyzer were also connected to the card. The software for the analog-to-digital card (Logger; Total Turnkey Solutions; Sydney, Australia) allowed for data acquisition. Second-by-second data of gas volume, FAC[O.sub.2], and Sp[O.sub.2] were recorded to computer by Logger software together with breath-by-breath data recorded by RSS100HR. The data recorded were then merged (SPSS version 11; SPSS; Chicago, IL) to obtain the breath-by-breath VE, FAC[O.sub.2], and Sp[O.sub.2] data. All volumes were corrected to body temperature and pressure and saturated with water vapor. FAC[O.sub.2] was converted to tension of carbon dioxide in the mixed venous blood when saturated with oxygen (PvC[O.sub.2]) using the formula "PvC[O.sub.2] = FAC[O.sub.2] x (Pb -P[H.sub.2]O)," where (Pb-P[H.sub.2]O) is the pressure of dry gas in the lung at 37[degrees]C. Daily barometric pressure (Pb) values were obtained from the Melbourne Meteorology Bureau. [DELTA]VE/[DELTA]PvC[O.sub.2], and [DELTA]VE/[DELTA]Sp[O.sub.2] were calculated as the slope of linear regression (line of best fit). Similarly, the slopes of [DELTA]VT/[DELTA]PvC[O.sub.2] and [DELTA]RR/[DELTA]PvC[O.sub.2] in the HCVR test and [DELTA]VT/ [DELTA]Sp[O.sub.2] and [DELTA]RR/[DELTA]Sp[O.sub.2] in the HVR test were also tested. To eliminate errors in the breath-by-breath analysis, those breaths lying > 2 SD outside the regression line were discarded, and the regression line recalculated. (26) For the HVR test, the VE for Sp[O.sub.2] < 95% was used to calculate the regression line. The signal time delay of the oximeter was corrected for each analysis, and absolute values of slopes were applied to the HVR testy. (27)
Toxicology: All subjects underwent blood toxicology. The collected blood samples were stored at -20[degrees]C until analysis. Testing included an alcohol screen by validated gas chromatography and an enzyme-linked immunosorbent assay screen (Microgenics; Freemont, CA) for drugs of abuse (amphetamines, benzodiazepines, cocaine, cannabinoids, and opioids). Blood was also screened for 3,4-methylenedioxyamphetamine ("ecstasy"), methadone, meperidine, benzodiazepines, antidepressants, and other prescription and over-the-counter drugs using a validated gas chromatography/mass spectrometry technique. (28) Methadone blood concentrations were quantified using high-performance liquid chromatography procedures routinely used in the laboratory (Victorian Institute of Forensic Medicine). The precision of this assay is [+ or -] 5%.
Polysomnography: In-laboratory, attended, full polysomnography was performed (Compumedics E Series data acquisition system; Compumedics; Victoria, Australia). Detailed methods for scoring of sleep and sleep-disordered breathing have been previously published. (22,23)
Respiratory Function Tests: FE[V.sub.1] and FVC were performed before and after inhalation of salbutamol, 300 [micro]g, via a spacer device. (29) Diffusion capacity of the lung for carbon monoxide (DLCO) and alveolar volume were measured after bronchodilator. (30) DLCO was corrected for alveolar volume and hemoglobin. In addition, the DLCO was corrected for carboxyhemoglobin in 27 of the 50 patients. (30) Carboxyhemoglobin adjustment for DLCO was as recommended by American Thoracic Society. (30) The P(A-a)[O.sub.2] (alveolar arterial oxygen pressure gradient) was calculated as the balance of Pa[O.sub.2] minus Pao[O.sub.2]. (31) Further details of respiratory function tests methods can be found in Teichtahl et al. (32)
Chest Radiograph: Standard posterior-anterior and lateral chest radiographs were performed to specifically assess cardiac size and pulmonary abnormalities. Radiographs were assessed and reported by a consultant respiratory physician and a consultant radiologist.
Resting Echocardiogram: Analysis of left and right heart size and function, and valwdar function was assessed using three-modality, two-dimensional, M-mode and Doppler eehocardiography (Sonos 4500; Philips; Audover, MA) based on the American Society of Echoeardiography standards. (33) As recommended, the 16-segment model for the assessment of regional wall motion abnormalities was adopted to measure left ventricular systolic function. (33) Echocardiograms were reported by an experienced consultant cardiologist.
Resting ECG: ECGs were performed on a standard cardiograph (Pagewriter XLi, model M1700A; Hewlett Packard; Andover, MA) and reported by an experienced consultant cardiologist.
Statistical Analysis
All values were expressed as mean [+ or -] SD unless otherwise stated. Between-group difference was tested by Mann-Whitney rank-stun test for skewed variables and unpaired Student t test for normally distributed variables. Pearson correlation coefficient was used for measuring linear association between two normally distributed variables. Multiple linear regression (stepwise backward deletion) was used to determine the factors influencing the variance of HCVR and HVR in MMT patients. HCVR and HVR were used as the dependent variable, respectively. Independent variables were chosen from blood toxicology, lung function data, demographic data, and sleep-disordered breathing data based on physiologic and clinical plausibility, and significance on univariate linear regression with the dependent variable. All variables included in analysis were screened for collinearity. A correlation of 0.9 was set as the upper limit of noncollinearity. (34) Nonnormally distributed variables were logarithmically or square transformed for linear regression analysis. Statistical analysis was performed (SPSS version 11; SPSS; Chicago, IL); p < 5% was considered statistically significant.
RESULTS
Demographics
Fifty stable MMT patients (25 men and 25 women) and 20 normal, nonopioid-using subjects (10 men and 10 women) matched by age, sex, height, and body mass index were studied. Demographic data and blood toxicology results are shown in Table 1. All MMT patients had methadone in their blood. Five patients used a selective serotonin reuptake inhibitor, one patient used a selective noradrenaline reuptake inhibitor, and one patient used a monoamine oxidase inhibitor antidepressant.
HCVR and HVR
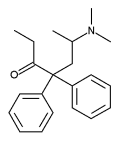
MMT patients had significantly decreased HCVR compared to the normal subjects (1.27 [+ or -] 0.61 L/min/mm Hg vs 1.64 [+ or -] 0.57 L/min/mm Hg, p = 0.01). HVR in MMT patients was significantly higher than the normal subjects (2.14 [+ or -] 1.58 L/min/% Sp[O.sub.2] vs 1.12 [+ or -] 0.7 L/min/% Sp[O.sub.2], p = 0.008) [Fig 1]. The differences in HCVR and HVR between MMT patients and normal subjects are due to RR rather than VT responses (Fig 2).
[FIGURES 1-2 OMITTED]
Arterial Blood Gas and Sleep-Disordered Breathing
Fourteen MMT patients had widened P(A-a)[O.sub.2] (> 15 mm Hg), and 10 patients had PaC[O.sub.2] > 45 mm Hg. (32) MMT patients had similar obstructive sleep apnea/hypopnea index (OSAHI) to the normal subjects (11.0 [+ or -] 10.3 vs 9.6 [+ or -] 9.2, p = 0.54). However, 30% of MMT patients had a central apnea index (CAI) > 5, and 20% patients had CAI > 10, whereas the highest CAI in normal subjects was 1. (23)
Toxicology
Methadone blood concentration and the use of benzodiazepines, antidepressants, and cannabis were not associated with HCVR or HVR in the MMT patients. However, within-group comparisons revealed MMT patients with an antidepressant in the blood had significantly reduced HCVR compared to patients without (0.83 [+ or -] 0.59 L/min/mm Hg vs 1.34 [+ or -] 0.59 L/min/mm Hg, p < 0.05). If we exclude the seven patients receiving antidepressants from the analysis, the trend in the difference of HCVR between the remaining MMT patients and normal subjects is confirmed (1.33 [+ or -] 0.59 L/min/mm Hg vs 1.64 [+ or -] 0.57 SD L/min/mm Hg, p = 0.06) but no longer reaches statistical significance.
Regression Analysis
Stepwise multiple regression analysis shows that significant variables associated with HCVR are OSAHI ([beta] = 0.28, t = 5.1, p = 0.00001), PaC[O.sub.2] ([beta] = - 0.06, t = - 3.6, p = 0.001), body height ([beta] = 2.1, t = 2.6, p = 0.01), and P(A-a)[O.sub.2] ([beta] = - 0.01, t = - 2.5, p = 0.02). These variables together explain 54% of variance of HCVR in MMT patients. Multiple linear regression analysis shows that significant variables associated with HVR in MMT patients are body height ([beta] = 4.9, t = 3.2, p = 0.002) and PaC[O.sub.2] ([beta] = -0.09, t = -2.8, p = 0.008), and these explain 26% of variance of HVR.
DISCUSSION
To our knowledge, this is the first cross-sectional study to investigate both HCVR and HVR in a large cohort of stable MMT patients receiving methadone for [greater than or equal to] 2 months, and to compare the data with that from normal, non-opioid-using normal subjects. We found that HCVR and HVR are significantly different in the subject groups. Interestingly, change in RR was the major component responsible for the differences in the ventilatory responses to both hypoxia and hypercapnia between the patients and normal subjects.
HVR
We have demonstrated that stable MMT patients have significantly heightened HVR compared to normal subjects. Our cross-sectional data support the concept that patients who are in an MMT program for > 2 months and who are receiving a stable dose of methadone have significantly heightened HVR when compared to a matched normal group of subjects. We do not have a clear explanation for the heightened HVR noted in our MMT patient group. Multiple regression analysis of our data indicates that PaC[O.sub.2] is negatively associated, and body height is positively associated with HVR in the M MT patients. It is well known that an elevated HVR will result in decreased PaC[O.sub.2] as is seen in patients with acute high-altitude central sleep apnea (35) and in patients with severe left ventricular failure. (36) We believe that the relationship found between HVR and PaC[O.sub.2] is one of HVR causing a reduction in PaC[O.sub.2] rather than the reverse. Height is related to HVR, (37) and we found a similar relationship between height and HVR for both the MMT patients and normal subjects. Therefore, height cannot explain the difference we found between our patient and normal groups. It is of interest that we did not find an association between methadone blood concentration, benzodiazepine, antidepressant, and cannabis use and HVR in the MMT patients. To our knowledge, there are no studies assessing the effects of long-term use of benzodiazepine, antidepressants, and cannabis on HVR. Benzodiazepines acutely reduce HVR, and they may potentiate the acute effects of opioids on HVR. (38) Cannabis does not change HVR acutely, (39) and the acute effects of an antidepressant on HVR have not been studied (to our knowledge). There may indeed be a relationship between the long-term use of the above drugs/therapies and HVR; however, due to our relatively small sample size for drugs other than methadone and the fact we did not measure blood concentrations, we may have missed the relationship. Given our data, we believe that no linear or nonlinear relationship exists between methadone blood concentration and the raised HVR in clinically stable MMT patients. We cannot exclude the possibility that a bimodal relationship exists between the two, and this is possible given that the blood drawn for toxicology and HVR tests was done at a single point in time within 6 h of methadone ingestion. In addition, there is significant interindividual variability of the pharmacokineties of methadone that may have impacted on the methadone blood concentration we measured. (40) Acute opioid use can significantly reduce HVR (16,18) and may therefore cause hypoxia.
In the other study assessing HVR in MMT patients, Santiago et al (20) compared HVR in two groups of MMT patients: group 1 consisted of six patients receiving methadone for < 2 months, and group 2 consisted of six patients receiving the drug for 8 to 43 months. They also compared HVR before and after ingestion of methadone in both groups. There was an HVR decline after methadone ingestion in both groups; however, post-methadone ingestion mean HVR in group 2 subjects (84 [+ or -] 26 L/min/mm Hg) was four times higher than that of group 1 subjects (21 [+ or -] 11 L/min/mm Hg) [p < 0.05]. The authors (20) discuss the significance of the decline in HVR immediately after methadone dose in both group 1 and group 2 patients, suggesting that the patients continue to tolerate hypoxia even after long-term use of methadone. However, the authors make no reference to the fact that there appears to be an elevation in HVR before and after methadone after long-term use of methadone compared with baseline, which would suggest a lack of tolerance to hypoxic stimulation over a period of time. The limitations of the Santiago et al (20) study were the lack of blood toxicology data, small sample size, all male subjects, and a lack of normal-subject data. The last point is particularly important, as it is unclear whether the premethadone HVR is normakreduced or elevated in those patients starting MMT. Recurrent acute after opioid reduction in HVR, as shown by Santiago et al (20) in MMT patients, may lead to recurrent episodic hypoxia, which may in the long term stimulate peripheral chemoreceptors and lead to long-term rise in HVR if there is ongoing opioid use. (20) This potential mechanism for heightened HVR in long-term MMT patients can explain both our findings and those of Santiago et al, (20) and may also explain why we found no correlation between blood methadone concentration and HVR. We therefore postulate that the raised HVR in stable MMT patients is produced by long-term daily use of methadone with or without ingestion of other drugs/therapies taken long term by these patients. The mechanism(s) driving the increased HVR in stable MMT patients needs to be further explored.
HCVR
We have shown that HCVR in stable MMT patients is significantly reduced when compared to our normal subjects. There are three previous studies (19-21) that have investigated HCVR in MMT patients. Marks and Goldring (19) studied eight subjects before institution of MMT, during 8 months in an MMT program, and after discontinuing from a MMT program. They found that after the institution of MMT, the mean HCVR in the eight subjects decreased, and returned to baseline levels after cessation of MMT. However, because of the small sample size, the changes were not statistically significant. Interestingly, the PaC[O.sub.2] rose significantly from 1 to 8 months after institution of MMT. This strongly suggests that the HCVR in their MMT patients did indeed drop from baseline and that it returned to pre-MMT level after eessation of the MMT program. Santiago et al (21) investigated HCVR in seven stable MMT patients and seven normal subjects. Unlike our study, they found the pre-methadone dose HCVR in their patients and normal subjects to be the same. However, HCVR measured soon after administration of methadone was reduced in the normal subjects, whereas there was no significant change found in the MMT group. The authors (21) conclude that full tolerance had developed with long-term intake of methadone. By studying only seven stable MMT and seven normal subjects, the study of Santiago et al (21) is prone to type 2 statistical error. Power calculations based on our study suggest that the Santiago et al (21) study had a power of 22% to detect a difference of 23% between the patient and normal group at a level of significance of 0.05. Nevertheless, Santiago et al (21) did show that HCVR is blunted acutely after methadone ingestion in normal subjects but not in the clinically stable MMT patients, suggesting that there is long-term tolerance to the acute effects of methadone with respect to HCVR. We believe our data show that in clinically stable MMT patients, there is a chronic reduction in ventilatory response to hypercapnia compared to normal subjects, and that the data of Santiago et al (21) suggest that there is development of compensatory mechanisms to the acute effects of methadone on HCVR with long-term methadone use.
We have not shown a linear correlation between blood methadone concentration and HCVR in the MMT patients, and this is not surprising given the discussion above. Because we performed the blood toxicology within 6 h of but not immediately after methadone ingestion, we have probably missed the acute effects of methadone on HCVR, but measured the chronic blunting of HCVR in this group of patients. As mentioned in this discussion, our data suggest that the relationship between long-term intake of methadone, methadone blood concentrations within 6 h of methadone ingestion, and HCVR is complex in nature, not linear, and probably subject to individual variation in methadone pharmacokinetics. (40) The research model for this study does not allow us to add further to the discussion of this interesting issue. Although the clinically stable MMT patients receiving antidepressants had much lower HCVR than clinically stable MMT patients not receiving antidepressants, the use of antidepressants in itself is not in our study associated with reduced HCVR in the group. We believe this is probably a function of the small sample size and needs further investigation. HCVR is reduced after acute dosing with selective serotonin reuptake inhibitor and tricyclic antidepressants in panic disorder patients. (41,42) Zwillich et al (39) showed an increase in HCVR after acute dosing with cannabis in eight normal subjects, and acute dosing with benzodiazepines also reduces HCVR in normal subjects. (43) Animal models suggest that acute dosing with benzodiazepines potentiates the acute effect of opioids on HCVR. (44) To our knowledge, there is no literature on the effects of long-term use of cannabis, antidepressants, and benzodiazepines on HCVR. Our data suggest that cannabis and benzodiazepines do not have a major independent association with HCVR in clinically stable MMT patients; however, we cannot say whether these drugs/therapies do or do not have an effect on HCVR when combined with other drugs.
Multiple regression analysis of our data shows that OSAHI, body height, P(A-a)[O.sub.2], and PC[O.sub.2] are significantly associated with HCVR in clinically stable MMT patients. (23,32) There are conflicting reports in the literature regarding HCVR in obstructive sleep apnea patients. (45-47) However, since in our study both MMT patients and normal subjects have similar OSAHI, it is unlikely that OSAHI contributes to the difference in HCVR between the two groups. (23) As for HVR, HCVR has been previously shown to relate to body height. (48) But body height did not contribute to the difference in HCVR between the two groups, as they were matched for body height. Fourteen MMT patients had widened P(A-a)[O.sub.2], and 10 patients had PaC[O.sub.2] > 45 mm Hg. (32) None of our patients had cardiorespiratory disease of severity that could explain a raised PaC[O.sub.2]; therefore it would seem reasonable to attribute the elevated PaC[O.sub.2] in some of our MMT patients to long-term blunting of HCVR. (32) Indeed, Greenwald (49) has shown that nonopioid-using smokers had significantly higher HCVR then MMT patients with similar smoking habits. Therefore, it is unlikely that smoking habit differences between our patients and normal subjects account for the difference found in HCVR between them. The reason for the association of widened P(A-a)[O.sub.2] and HCVR is less clear, although on our analysis widened P(A-a)[O.sub.2] explains only 7% of variance of HCVR. Blunted HCVR per se should not cause a widened P(A-a)[O.sub.2], nor can we postulate a sound physiologic reason for the widened P(A-a)[O.sub.2] causing blunting of HCVR. The widened P(A-a)[O.sub.2] in 14 of our MMT patients is explained by our findings of mildly decreased DLCO in MMT patients that we believe is secondary to their ongoing cigarette abuse and/or a manifestation of subclinical interstitial/granulomatous lung damage due to previous illicit drug use. (32,50-53) We therefore believe that the raised P(A-a)[O.sub.2] association with HCVR is a statistical aberration and is not physiologically related to HCVR.
The difference in HCVR we found between the stable MMT patients and normal subjects, although significant, was not of a high magnitude. The clinical significance of the finding is unclear. Nevertheless, chronic blunting of HCVR has potential to cause harm to subjects particularly if they are ingesting other illicit or prescribed drugs that have potential to cause further blunting of HCVR. This is illustrated in our study, in which we found that the MMT patients with antidepressants in their blood had HCVR of nearly half compared to MMT patients not receiving antidepressants.
BR and VT Responses
Our results show that RR and not VT response contributes to both the higher HVR and lower HCVR in MMT patients. No significant difference was found between the MMT patients and normal subjects in VT response to hypoxia and hypercapnia. To our knowledge, this is the first study reporting VT and RR responses to hypercapnia and hypoxia in stable MMT patients. Santiago et al (21) found that VT and not RR changed after taking methadone in normal subjects when breathing air and that the decrease in ventilation found was primarily a consequence of reduction of VT. Similarly, other studies reporting VT and RR changes after acute opioid ingestion were performed breathing air and were not testing HCVR or HVR. (54,55) Dripps and Comroe (54) reported that the reduction of VT is the primary reason for diminished ventilation after acute morphine ingestion in normal subjects breathing air. Eckenhoff and Oech (55) found that RR breathing air is usually unaffected by opioid use unless large opioid doses are used. It has been shown that therapeutic doses of morphine in humans depress all phases of respiratory activity including RR, X/E, and VT while breathing air. (8) Duffin and colleagues (56) examined chemoreflex control of breathing on 22 normal subjects using a modified Read rebreathing method. VT and RR responses to hypercapnia were measured. They found that VT and RR increase as the inspired carbon dioxide increases and that the responses of both VT and RR are nonlinear as the inspired carbon dioxide increases. They conclude that the breakpoint of the responses is the point at which the pattern of responses changes from primarily increasing VT to one of increasing RR as the inspired carbon dioxide increases. (56) In our HCVR test, the expired PC[O.sub.2] ranged from 45 to 65 mm Hg, and therefore the majority of our data points would be in the second phase of the responses in the data set of Duffin et al. (56) This is where the RR increase played the major role for ventilatory response to hypercapnia in their normal subjects. Our data therefore are compatible with a diminished RR response as the major component of the HCVR difference between MMT patients and normal subjects. There are no studies to our knowledge that have assessed the individual RR and VT responses to hypoxia. Our data show that it is the RR and not the VT response to hypoxia that is the major reason for the heightened HVR in the MMT patients compared to the normal subjects. The reason(s) for the up-regulation in the RR response of the peripheral chemoreceptors to hypoxia in our patient group is unclear and needs further study.
We have shown that clinically stable patients receiving long-term methadone have blunted HCVR and heightened HVR. These changes are related to changes in RR and not VT. We cannot assess whether these ventilatory responses contribute to the increased mortality rate noted in this patient group. At least 50% of deaths in MMT programs occur within 2 weeks of initiating methadone treatment, with the remainder occurring in clinically stable, long-standing MMT patients. (57) This suggests that the first weeks of illicit drug withdrawal and dosing of methadone are the most dangerous to the patient. However, our data suggest that patients may still be at risk after 2 to 3 months in an MMT program due to blunting of HCVR. Physicians and patients should be aware of our findings and be circumspect about prescribing therapies that may in addition acutely blunt HCVR in long-term MMT patients.
REFERENCES
(1) Substance Abuse and Mental Health Services Administration. 1999 national household survey on drug abuse (NHSDA). Available at: www.samhsa.gov/. Accessed August 15, 2005
(2) Hall WD, Ross JE, Lynskey MT, et at. How many dependent heroin users are there in Australia? Med J Aust 2000; 173:528-531
(3) NIH Consensus Conference. Effective medical treatment of opiate addiction. National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction. JAMA 1998; 280:1936-1943
(4) Institute of Medicine. Federal regulation of methadone treatment. Washington, DC: National Academy Press, 1995
(5) Ward J, Mattick RP, Hall W. Methadone maintenance treatment and other opioid replacement therapies. Amsterdam, the Netherlands: Harwood Academic, 1998
(6) Caplehorn JR, Dalton MS, Cluff MC, et at. Retention in methadone maintenance and heroin addicts' risk of death. Addiction 1994; 89:203-209
(7) Zador D, Sunjic S, Basili H. All-cause mortality rate and risk of dying in methadone maintenance treatment in New South Wales in 1990-95. International Opioid Overdose Symposium. Sydney, Australia: National Drug and Alcohol Research Centre, 1997
(8) Gutstein H, Akil H, eds. Opioid analgesics. New York, NY: McGraw-Hill, 2001
(9) Stanski DR, Greenblatt DJ, Lowenstein E. Kinetics of intravenous and intramuscular morphine. Clin Pharmacol Ther 1978; 24:52-59
(10) Chan K, Kendall MJ, Mitchard M, et al. The effect of ageing on plasma pethidine concentration. Br J Clin Pharmacol 1975; 2:297-302
(11) Mahla ME, White SE, Moneta MD. Delayed respiratory depression after alfentanil. Anesthesiology 1988; 69:593-595
(12) Chang J, Fish KJ. Acute respiratory arrest and rigidity after anesthesia with sufentanil: a case report. Anesthesiology 1985; 63:710-711
(13) Bailey PL, Stanley TH. Intravenous opioid anaesthetics. In: Miller RD, ed. Anesthesia. New York, NY: Churchill Livingston, 1994; 291-389
(14) Hickey RF, Severinghaus JW. Regulation of breathing: drug effects. In: Hornbein T, ed. Lung biology in health and disease. New York, NY: Marcel Dekker, 1981
(15) Tabatabai M, Kitahata LM, Collins JG. Disruption of the rhythmic activity of the medullary inspiratory neurons and phrenic nerve by fentanyl and reversal with nalbuphine. Anesthesiology 1989; 70:489-495
(16) Weil JV, McCullough RE, Kline JS, et at. Diminished ventilatory response to hypoxia and hypercapnia after morphine in normal man. N Engl J Med 1975; 292:1103-1106
(17) Berkenbosch A, Teppema LJ, Olievier CN, et al. Influences of morphine on the ventilatory response to isocapnic hypoxia. Anesthesiology 1997; 86:1342-1349
(18) Bailey PL, Lu JK, Pace NL, et al. Effects of intrathecal morphine on the ventilatory response to hypoxia. N Engl J Med 2000; 343:1228-1234
(19) Marks CE Jr, Goldring RM. Chronic hypercapnia during methadone maintenance. Am Rev Respir Dis 1973; 108: 1088-1093
(20) Santiago TV, Pugliese AC, Edelman NH. Control of breathing during methadone addiction. Am J Med 1977; 62:347-354
(21) Santiago TV, Goldblatt K, Winters K, et al. Respiratory consequences of methadone: the response to added resistance to breathing. Am Rev Respir Dis 1980; 122:623-628
(22) Teichtahl H, Prodromidis A, Miller B, et al. Sleep-disordered breathing in stable methadone programme patients: a pilot study. Addiction 2001; 96:395-403
(23) Wang D, Teichtahl H, Drummer OH, et al. Central sleep apnea in stable methadone maintenance treatment patients. Chest 2005; 2:1348-1356
(24) Rebuck AS, Campbell EJ. A clinical method for assessing the ventilatory response to hypoxia. Am Rev Respir Dis 1974; 199:345-350
(25) Read DJ. A clinical method for assessing the ventilatory response to carbon dioxide. Australas Ann Med 1967; 16: 20-32
(26) Prisk GK, Elliott AR, West JB. Sustained microgravity reduces the human ventilatory response to hypoxia but not to hypercapnia. J Appl Physiol 2000; 88:1421-1430
(27) Shaw RA, Schonfeld SA, Whitcomb ME. Progressive and transient hypoxic ventilatory drive tests in healthy subjects. Am Rev Respir Dis 1982; 126:37-40
(28) Drummer OH, Horomidis S, Kourtis S, et at. Capillary gas chromatographic drug screen for use in forensic toxicology. J Anal Toxicol 1994; 18:134-138
(29) American Thoracic Society. Standardization of spirometry, 1994 update. Am J Respir Crit Care Med 1995a; 152:1107-1136
(30) American Thoracic Society. Single-breath carbon monoxide diffusing capacity (transfer factor): recommendations for a standard technique, 1995 update. Am J Respir Crit Care Med 1995b; 152:2185-2198
(31) Hughes JMB, Pride NB. Lung function tests: physiological principles and clinical applications. London, UK: WB Saunders, 1999
(32) Teichtahl H, Wang D, Cunnington D, et al. Cardiorespiratory function in stable methadone maintenance program patients. Addict Biol 2004; 3-4:247-253
(33) Schiller NB, Shah PM, Crawford M, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 1989; 2:358-367
(34) Tabachnick B, Fidell L. Using multivariate statistics. 4th ed. Boston, MA: Allyn and Bacon, 2001
(35) Douglas CG, Haldane JS, Henderson Y, et at. Physiological observations made on Pike's Peak, Colorado, with special reference to adaption to low barometric pressure. Philos Trans R Soc Lond B Biol Sci 1913; 203:185-318
(36) Naughton MT. Pathophysiology and treatment of Cheyne-Stokes respiration. Thorax 1998; 53:514-518
(37) Aitken ML, Franklin JL, Pierson DJ, et al. Influence of body size and gender on control of ventilation. J Appl Physiol 1986; 60:1894-1899
(38) Bailey PL, Pace NL, Ashburn MA, et al. Frequent hypoxemia and apnea after sedation with midazolam and fentanyl. Anesthesiology 1990; 73:826-830
(39) Zwillich CW, Doekel R, Hammill S, et al. The effects of smoked marijuana on metabolism and respiratory control. Am Rev Respir Dis 1978; 118:885-891
(40) Eap C, Buelin T, Baumann P. Interindividual variability of the clinical pharmacokinetics of methadone: implications for the treatment of opioid dependence. Clin Pharmacokinet 2002; 41:11503-11593
(41) Bocola V, Treeco MD, Fabbrini G, et al. Antipanic effect of fluoxetine measured by C[O.sub.2] challenge test. Biol Psychiatry 1998; 43:612-615
(42) Pols H, Lousberg H, Zandbergen J, et al. Panic disorder patients show decrease in ventilatory response to C[O.sub.2] after clomipramine treatment. Psychiatry Res 1993; 47:295-296
(43) Gross JB, Blouin RT, Zandsberg S, et al. Effect of flumazenil on ventilatory drive during sedation with midazolam and alfentanil. Anesthesiology 1996; 85:713-720
(44) Gerak LR, Brandt MR, France CP. Studies on benzodiazepines and opioids administered alone and in combination in rhesus monkeys: ventilation and drug discrimination. Psychopharmacology (Berlin) 1998; 137:164-174
(45) Verbraecken J, De Backer W, Willemen M, et al. Chronic C[O.sub.2] drive in patients with obstructive sleep apnea and effect of CPAP. Respir Physiol 1995; 101:279-287
(46) Garay SM, Rapoport D, Sorkin B, et al. Regulation of ventilation in the obstructive sleep apnea syndrome. Am Rev Respir Dis 1981; 124:451-457
(47) Lopata M, Onal E. Mass loading, sleep apnea, and the pathogenesis of obesity hypoventilation. Am Rev Respir Dis 1982; 126:640-645
(48) Kafer ER. Idiopathic scoliosis: mechanical properties of the respiratory system and the ventilatory response to carbon dioxide. J Clin Invest 1975; 55:1153-1163
(49) Greenwald M. Effects of opioid dependence and tobacco use on ventilatory response to progressive hypercapnia. Pharmacol Biochem Behav 2004; 77:39-47
(50) Taylor DR, Hall W. Respiratory health effects of cannabis: position statement of the Thoracic Society of Australia and New Zealand. Intern Med J 2003; 33:310-313
(51) Overland ES, Nolan AJ, Hopewell PC. Alteration of pulmonary function in intravenous drug abusers: prevalence, severity, and characterization of gas exchange abnormalities. Am J Med 1980; 68:231-237
(52) Cunnington D, Teichtahl H, Hunt JM, et al. Necrotizing pulmonary granulomata in a marijuana smoker. Chest 2000; 117:1511-1515
(53) Douglas FG, Kafilmout KJ, Patt NL. Foreign particle embolism in drug addicts: respiratory pathophysiology. Ann Intern Med 1971; 75:865-880
(54) Dripps RL, Comroe JH. Clinical studies on morphine: I. The immediate effect of morphine administered intravenously and intramuscularly upon the respiration of normal man. Anesthesiology 1945; 6:462-468
(55) Eckenhoff JE, Oech R. The effects of narcotics and antagonists upon respiration and circulation in man. Clin Pharmacol Ther 1960; 1:483-524
(56) Duffin J, Mohan RM, Vasiliou P, et al. A model of the chemoreflex control of breathing in humans: model parameters measurement. Respir Physiol 2000; 120:13-26
(57) Caplehorn JR, Drummer OH. Mortality associated with New South Wales methadone programs in 1994: lives lost and saved. Med J Aust 1999; 170:104-109
* From the Department of Respiratory & Sleep Disorders Medicine (Drs. Teichtahl, Quinnell, Tran, Dr. Cunnington, and Mr Wang); Drug and Alcohol Service (Dr. Kronborg), Western Hospital; and Victorian Institute of Forensic Medicine (Dr. Drummer), Department of Forensic Medicine, Monash University, Victoria, Australia.
Manuscript received March 15, 2005; revision accepted May 3, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Harry Teichtahl, MBBS, Department of Respiratory & Sleep Disorders Medicine, Western Hospital, Victoria, Australia, 3011; e-mail: harry.teichtahl@wh.org.au
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group