Objectives: The aim of the present study was to assess the usefulness of positron emission tomography (PET) with the amino acid tracer ^sup 11^C-methionine (MET) as a predictor of time to progression (TTP) in patients with supratentorial grade 2 gliomas.
Methods: Twenty-seven patients with glioma grade 2 subjected to a baseline PET scan received no anti-tumour treatment except for a diagnostic operation, and were followed until tumour progression. The prognostic impact of the MET uptake and of other prognostic factors was studied.
Results: Twenty-five of the patients (93%) experienced tumour progression after a median of 103 weeks. Low uptake of MET was a predictor for long TTP in patients with oligodendrogliomas (p=0.04) but not in astrocytomas/oligoastrocytomas. Other predictors for long TTP were oligodendroglioma histology (p= 0.009) and seizures as presenting symptom (p=0.03). Favourable prognostic factors for overall survival were oligodendroglioma histology (p=0.002) and good performance status (p=0.03).
Conclusions: PET MET has a definite role in the therapeutic management of grade 2 gliomas. However, for the optimal use of PET MET in the clinical management of these patients, histological subclassification of the tumour is required. [Neurol Res 2005; 27: 516-521]
Keywords: Low-grade glioma; positron emission tomography; prognosis; time to progression
INTRODUCTION
Patients with low-grade gliomas are often previously healthy adults who, at the onset of disease, experience their first epileptic seizure. Since no treatment has been proven to prolong survival, it is tempting to the neurooncologist to just administer an anti-epileptic drug and then wait and see.
The interim results from the EORTC trial 28845 recently demonstrated a prolonged time to progression (TTP) but no survival benefit by radiotherapy1. The two earlier dose-response studies have not shown any advantage of high-dose radiation compared with moderate dose2,3. Data from the three radiation trials were used to determine the most important prognostic factors for TTP and overall survival: patient age, histological subtype, tumour size and clinical status4. The only published randomized chemotherapy trial so far showed no advantage in response rate or survival by CCNU5. Two recent trials on the alkylating agent temozolomide demonstrated response rates of 47%6 and 61 %7, respectively, in progressive low-grade gliomas. No controlled trial has investigated the effects of surgery.
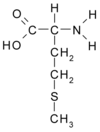
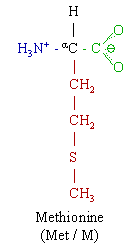
The uptake of ^sup 11^C-methionine (MET) measured by positron emission tomography (PET) is associated with the proliferative activity8,9 and microvessel density of gliomas10 and has shown prognostic value in low-grade gliomas11-13. In follow-up studies after radiotherapy, a decline in the MET uptake is observed early and may persist for years14,15. The aim of the present study was to analyse the impact of baseline MET uptake on TTP.
MATERIALS AND METHODS
Patients
A retrospective review of the medical records was performed on patients aged over 15 years who had given their informed consent to undergo a ^sup 11^C-MET PET scan as part of the diagnostic tumour investigation at the Neurosurgical Clinic of the University hospital in Uppsala from 1983 to 1999. Pilocytic astrocytomas, gangliogliomas, pleomorphic xanthoastrocytomas and tumours with ependymal foci were excluded. In the review of the histological reports, tumours with signs of necrosis, endothelial cell proliferation and more than single mitoses were excluded. All cases were reevaluated histologicalIy by a neuropathologist and excluded if signs of anaplasia were present. Twentyseven patients had no other treatment than the diagnostic biopsy or subtotal resection before tumour progression, and these were included in the study.
The following information was collected from the patient records: age, sex, presenting symptoms, radiological appearance [tumour size, location and presence of contrast enhancement on computed tomography (CT) or magnetic resonance imaging (MRI)], pre-operative and postoperative performance status according to the Karnofsky Performance status (KPS)16, date and extent of diagnostic surgery (biopsy or subtotal resection) and histology. The extent of tumour resection was based on postoperative CT and the surgeon's operative notes.
Survival was defined as the time period between the presenting symptoms and the date of death or end of the study (1 August, 2004). Time to tumour progression (TTP) was measured from the baseline PET scan to the first event of (1) clinical deterioration corresponding to the location of the original tumour, or (2) tumour growth or increasing contrast enhancement on CT or MRI. Data concerning the time and the cause of death were collected from the central health authorities (the National Cause of Death Register Data).
PET technique
The PET scans of patients 1-8 were performed in a Scanditronix PC-384 B PET camera providing three slices of ~11 mm, a slice separation of 13.5 mm and a spatial resolution of 8 mm (Camera 1). From November 1991 all patients were studied in a Scanditronix/GEMS PC2048-15B camera, providing 15 contiguous 6.5 mm slices with a 6 mm axial and transaxial resolution (Camera 2). The PET scans were performed as described by Bergstrom et al.17. The MET was injected intravenously, and dynamic emission scanning was performed. Summation images covering 20-40 minutes after the injection were used for the analysis. Doses of 50 to 200 MBq were used for Camera 1 and 300-400 MBq for Camera 2. The new cameras were calibrated on a routine basis at the PET centre using dose calibrator and well crystal. All the patients fasted for at least 4 hours before the investigation. No PET scan was performed within the first month after surgery or biopsy.
Analysis of the PET images
In each tumour, the uptake in two tumour-associated regions was measured and was related to a reference area in the healthy hemisphere (hot spot/cortex ratio). The reference area, cortex, consisted of six cortical areas covering the frontal, temporal and occipital cortices in the healthy hemisphere at the level of the thalami, each ~30 × 10 mm. The hot spot was defined as ten connected pixels with the highest MET uptake within the tumour, representing an area of 55-60 mm^sup 2^ (Figure 7). The categorization cut-off for the MET uptake was set 2.2 in the statistical analyses according to earlier studies on low-grade gliomas11,12 . For astrocytomas and oligoastrocytomas the alternative dichotomies from earlier studies, 2.0 and 2.1, were evaluated12,13.
Statistical methods
The log-rank test and Kaplan-Meier plots were used to compare the impact of the MET uptake and the other variables on TTP. The limited number of patients did not support multivariate models. The statistical calculations were performed in JMP, version 5.0.1 a (SAS Institute Inc., Cary, NC, USA).
RESULTS
Patient characteristics
The clinical data are presented in Table 1. The median patient age at the time of histological diagnosis was 41 years (range 17-68 years). The most common presenting symptom was seizures (26 patients, 96%), and occurred as the only presenting symptom in 20 patients (74%). Four patients had a KPS of 80, whereas the remaining patients had a higher ranking. Nine tumours (33%) were contrast enhancing at the time of the first PET scan. Fourteen tumours (52%) had a largest diameter of >4 cm. The histological diagnosis was oligodendroglioma in 12 cases (44%), astrocytoma in 10 cases (37%) and oligoastrocytoma in five cases (19%). A diagnostic biopsy was performed in 17 patients (63%) and subtotal resection in the remaining 10 cases. No patient received radiotherapy or chemotherapy before clinical or radiographie tumour progression.
Baseline MET uptake
The overall median hot spot/cortex ratio at baseline for the whole group was 1.8 (range 0.86-3.5). Four patients (15%) had no measurable tumour volumes on the PET scan and their hot spots were measured within the tumour delineation on MRI.
TTP, treatment and survival
Twenty-five patients (93%) experienced tumour progression. The median TTP was 103 weeks after the baseline PET scan (Kaplan-Meier estimate). Four patients were re-operated and in two cases the tumour had dedifferentiated to a more malignant grade. After tumour progression, radiotherapy was administered in 22 of the 25 patients at doses of 50-57.8 Gray (Gy) in 1.8 or 2 Gy fractions. Three patients received chemotherapy, in two cases PCV [procarbazine, lomustine (CCNLJ), and vincristine] in cycles over 42 days, and in one case temozolomide.
At the end of the study 17 patients (63%) had died, and for all of these individuals the tumour was noted as the direct or underlying cause of death in the National Cause of Death Register. The median overall survival time was 78 months after the baseline PET scan (Kaplan-Meier estimate). The median follow-up time for patients still alive (censored) was 77.5 months (range 62-114 months).
Prognostic factors
Significant prognostic factors for long TTP were oligodendroglioma histology (p=0.009) and seizures as the presenting symptom (p=0.03) (Table 2). The uptake of MET was not a prognostic factor in the whole patient sample, probably due to the relatively high uptake and favourable prognosis in oligodendrogliomas compared with astrocytomas. In the present study, the MET uptake was a median 1.6 in astrocytomas and 2.0 in oligodendrogliomas (p=0.13, Wilcoxon test). In patients with oligodendrogliomas, a low uptake of MET was a predictor for long TTP (p=0.04) (Figure 2), No other patient- or tumour-related prognostic factor was significant in oligodendrogliomas. Patients who had been subjected to subtotal tumour resection had a shorter TTP, probably due to a selection bias (p=0.02). The uptake of MET was not a prognostic predictor in astrocytomas/oligoastrocytomas (Figure 3).
Positive prognostic factors for overall survival were oligodendroglioma histology (p=0.002) and good performance status (p=0.03) (Table 3).
DISCUSSION
The present study demonstrates an association between baseline MET uptake and the natural course, in terms of time until progressive disease, in untreated patients with grade 2 oligodendrogliomas. Earlier prognostic PET studies have concentrated on correlations with histological grade13 or patient survival11,12,18. To our knowledge, no previous study has been able to assess the prognostic impact of PET in glioma patients, excluding the potential bias from radical surgery, radiotherapy, chemotherapy or other anti-tumour treatment.
There is no consensus regarding the best treatment of patients with grade 2 gliomas. No therapy has shown to increase patient survival1-3,5,19. It is likely that radical tumour resection19,20 and radiotherapy1 prolong TTP. It is not obvious, however, that all patients should receive early treatment. Recent reports have put forward the risk for long-term adverse effects by radiation3,21-24. A reasonable strategy would be to administer treatment at diagnosis for those who face a substantial risk of rapidly progressive disease25. PET may be one of the prognostic factors used in the selection of these high-risk patients.
Several tracers may assess the growth rate of brain tumours. The uptake of the amino acid tracer MET is mainly determined by a specific carrier-mediated mechanism26,27 and is correlated to the proliferative activity of the tumour cells8,9. To date, PET MET has been shown as useful in various clinical situations: in guiding stereotactic biopsies28, in differentiating between low-grade tumours and non-tumour lesions, and as a prognostic marker for survival11-13. A few reports have evaluated the method as a tool for follow-up after radiotherapy30. In a post-surgical follow-up of 30 low-grade astrocytomas using MET and18F-fluorodeoxyglucose (FDG), Roelcke et al. found no significant difference in tracer uptake between tumours with or without adjuvant radiotherapy31. PET MET has also shown to be of some value in disclosing residual tumour after radiotherapy in selected cases of low-grade astrocytomas15. In two studies PET MET was more suitable than FDG in monitoring therapeutic effects after brachytherapy with 125I seeds32,33.
In the present study, PET MET was not a prognostic indicator for astocytomas/oligodendrogliomas, neither analysed together nor as separate histological groups. The alternative cut-offs for the MET uptake: 2.0, 2.1, 2.2, were all evaluated. This lack of difference in outcome may be explained by the small sample size. However, previous studies have shown the same trend towards a clearer prognostic impact of PET MET in pure oligodendrogliomas12,14. The lack of prognostic significance for PET MET in the whole patient sample of grade 2 gliomas was expected. Oligodendrogliomas have a generally higher MET uptake that may be attributed to a higher cell density but probably also to other, thus far unknown, factors12,34,35. The paradoxical combination of a high MET uptake and a better prognosis compared with astrocytic tumours, makes it necessary to include the histology of the tumour to be able to use PET MET as a prognostic factor. This is a disadvantage for PET MET in the practical management of low-grade gliomas. On the other hand, the radiographie diagnosis of low-grade glioma is uncertain and histological verification is therefore essential for the correct management36. The prognostic significance of histological characteristics, presenting symptoms and Karnofsky performance status were confirmed in the current study (Tables 2 and 3).
The patient sample in this study is small and represents a selection of low-grade glioma patients with baseline PET scans. The sample size did not allow the use of multivariate analysis to adjust for confounding factors. The results concerning TTP are, however, not biased by treatment-related factors, which is often the case in retrospective studies. Furthermore, two different PET cameras with dissimilar spatial resolution and slice separation were used for imaging the tumours. This shortcoming suggests some caution in the interpretation of the data. However, the routine of calibrating new cameras at the PET-centre and the use of only relative MET values in the study should diminish the risk for this potential bias. Also, the results are well consistent with previous reports11,12,18,37,38, strengthening the reliability of the study.
In conclusion, PET MET was a prognostic indicator for TTP in untreated patients with grade 2 oligodendrogliomas. PET MET may be very useful in the therapeutic management of low-grade gliomas, but less valuable without histological diagnosis.
ACKNOWLEDGEMENTS
This work was supported by grants from the Lions Cancer Foundation and Erik, Karin and Costa Selanders Foundation. We acknowledge Henry Engler, MD, and the staff at the PET Centre in Uppsala for technical assistance.
REFERENCES
1 Karim AB, Afra D, Cornu P, et al. Randomized trial on the efficacy of radiotherapy for cerebral low-grade glioma in the adult: European Organization for Research and Treatment of Cancer Study 22845 with the Medical Research Council study BRO4: An interim analysis. Int J Radiat Oncol Biol Phys 2002; 52: 316-324
2 Karim AB, Maat B, Hatlevoll R, et al. A randomized trial on dose-response in radiation therapy of low-grade cerebral glioma: European Organization for Research and Treatment of Cancer (EORTC) Study 22844. Int J Radiat Oncol Biol Phys 1996; 36: 549556
3 Shaw E, Arusell R, Scheithauer B, et al. Prospective randomized trial of low- versus high-dose radiation therapy in adults with supratentorial low-grade glioma: Initial report of a north central cancer treatment group/radiation therapy oncology group/eastern cooperative oncology group study. J Clin Oncol 2002; 20: 22672276
4 Pignatti F, van den Bent M, Curran D, et al. Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin Oncol 2002; 20: 2076-2084
5 Eyre HJ, Crowley JJ, Townsend JJ, et al. A randomized trial of radiotherapy versus radiotherapy plus CCNU for incompletely resected low-grade gliomas: A Southwest Oncology Group study. J Neurosurg 1993; 78: 909-914
6 Pace A, Vidiri A, Galie E, et al. Temozolomide chemotherapy for progressive low-grade glioma: Clinical benefits and radiological response. Ann Oncol 2003; 14: 1722-1726
7 Quinn JA, Reardon DA, Friedman AH, et al. Phase II trial of temozolomide in patients with progressive low-grade glioma. J Clin Oncol 2003; 21: 646-651
8 Langen KJ, Muhlensiepen H, Holschbach M, et al. Transport mechanisms of 3-[123l]iodo-alpha-methyl-L-tyrosine in a human glioma cell line: Comparison with [3H]methyl]-L-methionine. J Nucl Med 2000; 41: 1250-1255
9 Sato N, Suzuki M, Kuwata N, et al. Evaluation of the malignancy of glioma using 11C-methionine positron emission tomography and proliferating cell nuclear antigen staining. Neurosurg Rev 1999; 22: 210-214
10 Kracht LW, Friese M, Herholz K, etal. Methyl-[11 C]-l-methionine uptake as measured by positron emission tomography correlates to microvessel density in patients with glioma. Eur J Nucl Med Mol Imaging 2003; 30: 868-873
11 De Witte O, Goldberg I, Wikler D, et al. Positron emission tomography with injection of methionine as a prognostic factor in glioma. ) Neurosurg 2001; 95: 746-750
12 Ribom D, Eriksson A, Hartman M, et al. Positron emission tomography 11C-methionine and survival in patients with lowgrade gliomas. Cancer 2001; 92: 1541-1549
13 Kaschten B, Stevenaert A, Sadzot B, et al. Preoperative evaluation of 54 gliomas by PET with fluorine-18-fluorodeoxyglucose and/or carbon-11 -methionine. J Nucl Med 1998; 39: 778-785
14 Ribom D, Engler H, Blomquist E, et al. Potential significance of (11)C-methionine PET as a marker for the radiosensitivity of low-grade gliomas. Eur J Nucl Med 2002; 29: 632-640
15 Nuutinen J, Sonninen P, Lehikoinen P, et al. Radiotherapy treatment planning and long-term follow-up with [(11)C]methionine PET in patients with low-grade astrocytoma [In Process Citation]. Int J Radiat Oncol Biol Phys 2000; 48: 43-52
16 Karnofsky DA, Abelmann WH, Craver LF. The use of nitrogen mustards in the palliative treatment of carcinoma. With particular reference to brochogenoc carcinoma. Cancer 1948; 1: 634-656
17 Bergstrom M, Lundqvist H, Ericson K, et al. Comparison of the accumulation kinetics of L-(methyl-11C)-methionine and D-(methyl-11C)-methionine in brain tumors studied with positron emission tomography. Acta Radiol 1987; 28: 225-229
18 De Witte O, Levivier M, Violon P, et al. Prognostic value positron emission tomography with [1 8F]fluoro-2-deoxy-D-glucose in the low-grade glioma. Neurosurgery 1996; 39: 470-477
19 Keles GE, Lamborn KR, Berger MS. Low-grade hemispheric gliomas in adults: A critical review of extent of resection as a factor influencing outcome. J Neurosurg 2001; 95: 735-745
20 Berger MS, Deliganis AV, Dobbins J, et al. The effect of extent of resection on recurrence in patients with low grade cerebral hemisphere gliomas. Cancer 1994; 74: 1784-1791
21 Olson JD, Riedel E, DeAngelis LM. Long-term outcome of low-grade oligodendroglioma and mixed glioma [see comments]. Neurology 2000; 54: 1442-1448
22 Armstrong CL, Hunter JV, Ledakis GL, et al. Late cognitive and radiographie changes related to radiotherapy: initial prospective findings. Neurology 2002; 59: 40-48
23 Postma TJ, Klein M, Verstappen CC, et al. Radiotherapy-induced cerebral abnormalities in patients with low-grade glioma. Neurology 2002; 59: 121-123
24 Surma-aho O, Niemela M, Vilkki J, et al. Adverse long-term effects of brain radiotherapy in adult low-grade glioma patients. Neurology 2001; 56: 1285-1290
25 Stupp R, Janzer RC, Hegi ML, et al. Prognostic factors for lowgrade gliomas. Sem in Oncol 2003; 30: 23-28
26 Jager PL, Vaalburg W, Pruim J, et al. Radiolabeled amino acids: Basic aspects and clinical applications in oncology. J Nucl Med 2001; 42: 432-445
27 Weber WA, Wester HJ, Grosu AL, et al. O-(2-[1 8F]fluoroethyl)-L-tyrosine and L-[methyl-11C]methionine uptake in brain tumours: initial results of a comparative study. Eur J Nucl Med 2000; 27: 542-549
28 Pirotte B, Goldman S, David P, et al. Stereotactic brain biopsy guided by positron emission tomography (PET) with [F-18]fluorodeoxyglucose and [C-11]methionine. Acta Neurochir Suppl (Wien) 1997; 68: 133-138
29 Herholz K, Holzer T, Bauer B, et al. 11C-methionine PET for differential diagnosis of low-grade gliomas. Neurology 1998; 50: 1316-1322
30 Roelcke U, Leenders KL. PLT in neuro-oncology. J Cancer Res Clin Oncol 2001; 127: 2-8
31 Roelcke U, von Ammon K, Hausmann O, et al. Operated low grade astrocytomas: a long term PET study on the effect of radiotherapy. J Neurol Neurosurg Psychiatry 1999; 66: 644647
32 Voges J, Herholz K, Holzer T, et al. 11C-methionine and 18F-2-fluorodeoxyglucose positron emission tomography: A tool for diagnosis of cerebral glioma and monitoring after brachytherapy with 1251 seeds. Stereotact Funct Neurosurg 1997; 69: 129-135
33 Wurker M, Herholz K, Voges J, et al. Glucose consumption and methionine uptake in low-grade gliomas after iodine-125 brachytherapy. Eur J Nucl Med 1996; 23: 583-586
34 Daumas-Duport C. Histological grading of gliomas. Curr Opin Neurol Neurosurg 1992; 5: 924-931
35 Derlon JM, Petit-Taboue MC, Chapon F, et al. The in vivo metabolic pattern of low-grade brain gliomas: a positron emission tomographic study using 18F-fluorodeoxyglucose and 11C-L-methylmethionine. Neurosurgery 1997; 40: discussion 287-288
36 Bell D, Grant R, Collie D, et al. How well do radiologists diagnose intracerebral tumour histology on CT? Findings from a prospective multicentre study. Br J Neurosurg 2002; 16: 573-577
37 Francavilla TL, Miletich RS, Di Chiro G, et al. Positron emission tomography in the detection of malignant degeneration of low-grade gliomas. Neurosurgery 1989; 24: 1-5
38 Patronas NJ, Di Chiro G, Kufta C, et al. Prediction of survival in glioma patients by means of positron emission tomography. J Neurosurg 1985; 62: 816-822
Dan Ribom*,[dagger] and Anja Smits*
* Department of Neuroscience, Neurology, University Hospital, SE-75 7 85 Uppsala, Sweden
[dagger] Department of Neurology, Länssjukhuset, SE-301 85 Halmstad, Sweden
Correspondence and reprint requests to: Dan Ribom, Department of Neurology, Länssjukhuset, SE-301 85 Halmstad, Sweden. [dan.ribom@ lthalland.se] Accepted for publication February 2005.
Copyright Maney Publishing Jul 2005
Provided by ProQuest Information and Learning Company. All rights Reserved